Mila’s legacy: The little girl who could change how medicines are made in Britain

Julia Vitarello and her family lived an outdoor life against the backdrop of the Rocky Mountains in Colorado. Her daughter Mila was adventurous. She was skiing at the age of two and could hike for hours in her tiny hiking boots.
But at the age of about three and a half, Mila started to lose her agility, became clumsy and was often covered in bruises. Her mother became increasingly scared and nervous as problems with her co-ordination, speech and vision emerged.
Mila went to a hundred different medical and therapy appointments but was told she would grow out of her conditions. Julia was told she was crazy.
Yet it wasn’t until they ended up in a busy emergency room in Colorado in 2016, when Mila was six, that doctors noticed her condition was serious. Within a week Julia received a diagnosis that would chill the heart of every parent. She had a neurological condition called Batten’s disease – a rare and fatal genetic disorder.
Batten disease is a cruel thief of children’s lives. It progressively robs them of their vision, speech, and movement, leading to an early death. Julia set out to raise millions of dollars in the faint hope of finding a gene therapy could treat her daughter.

This journey led her to the door of Timothy Yu, a neurologist and geneticist at Boston Children’s Hospital who offered to help find the exact mutation that caused Mila’s disease.
When he and his team found it, they realised it could be fixed with a small synthetic piece of DNA or RNA – something known as an antisense oligonucleotide or ASO. Even more incredibly they realised it was something that could be ordered inexpensively from a laboratory research catalogue.
But most countries have strict rules about how drugs are made and what evidence is needed before they can be given to patients. Not only was there limited time to conduct trials, Mila’s mutation was unique making a traditional trial impossible.
Dr Yu found a pathway called “compassionate use” that allowed him to use investigational medicines on a patient with a life-threatening conditions. In a heroic effort, almost exactly a year later the drug they called Milasen was given to Mila. It was the world’s first customised medicine.
Did Milasen work? “It did… and it didn’t,” says Dr Yu. The first year was amazing, recalls Julia, as her daughter’s disease was stable and she stopped having seizures. Yet in the third year Mila’s disease started to take its course.
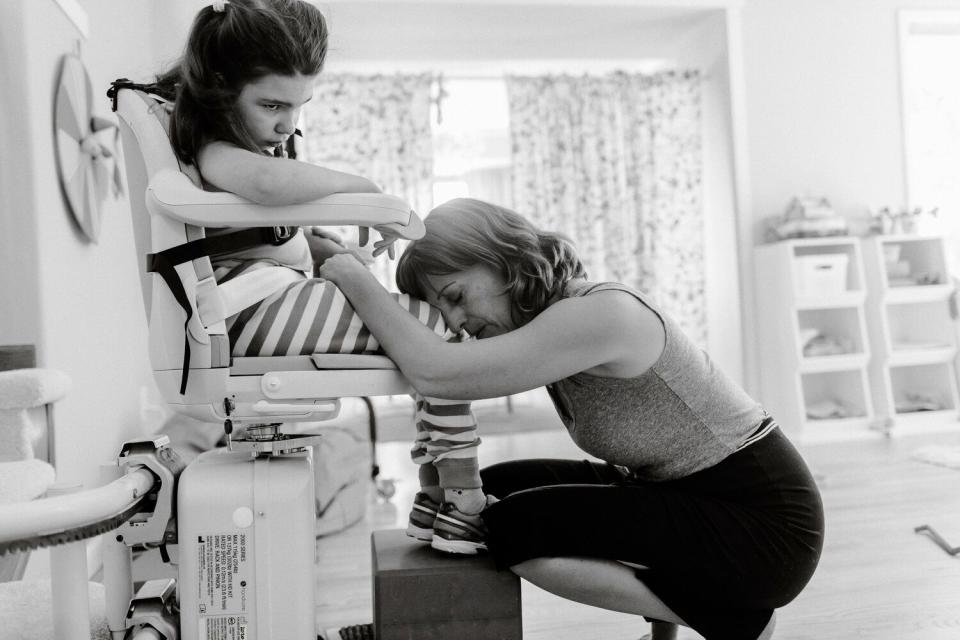
Julia recalls trying hard not to imagine what might have happened if Mila had received the drug before so much neurological damage had been done. Eventually Mila couldn’t eat, see or speak and at the end of that third year, Julia says Mila’s “very big spirit left her little body and it was just unbearable”.
For many parents this devastation might be the end of the story. But Julia had already decided that what had happened was “bigger than Mila” and set out on a journey to bring the technology to millions of children. Her progress is chronicled in a new BBC Radio 4 documentary, Mila’s Legacy.
Achieving her goals will mean changing the way that medicines are made and tested – because the pathway used for Mila is too costly and difficult to use for more than a tiny number of children. Julia’s efforts to convince America’s drug regulator, the Food and Drug Regulator, got nowhere.
Then she turned to Britain. It had a unique set of attributes that made it attractive. First it has leading academic centres interested in rare diseases in children such as the University of Oxford. Second, it has a strong clinical genetics body in the form of Genomics England, which is planning work to sequence the genomes of newborn children which will one day help detect fatal genetic diseases earlier in life.
Finally it has a drug regulator – the Medicines and Healthcare products Regulatory Agency – that is keen to make use of its post-Brexit freedoms to innovate.
The result is a pilot project called the Rare Therapies Launch Pad, which will find, treat and trial customised medicines in ten or fifteen children with fatal brain diseases.
It will gather the evidence to show that such treatments are safe and effective allowing them to be used more routinely.
Success in this will mark the beginning of a new era of medicine where drugs are more routinely tailored to individuals. Julia’s journey from a mother seeking a miracle for her child to a catalyst for change in medicine is a testament to the power of hope.
The next steps in Mila’s legacy will be here, in Britain, but the impact could be felt around the world.
Listen to Mila’s Legacy, a Radio 4 documentary presented by Natasha Loder broadcast on March 29th at 11am. Ms Loder is Health Editor at The Economist
Protect yourself and your family by learning more about Global Health Security

