MDs Reveal the Top 2 Stomach Ulcer Causes (Stress Isn't One of Them) + How to Block a Flare-Up
You likely already know that there’s a connection between anxiety-inducing gastrointestinal (GI) pain and stomach ulcers. But what you might not know is that there are two common stomach ulcer causes — and stress is surprisingly not one of them. Here, experts explain the biggest ulcer triggers and the best ways to protect yourself from a flare-up.
What is a stomach ulcer?
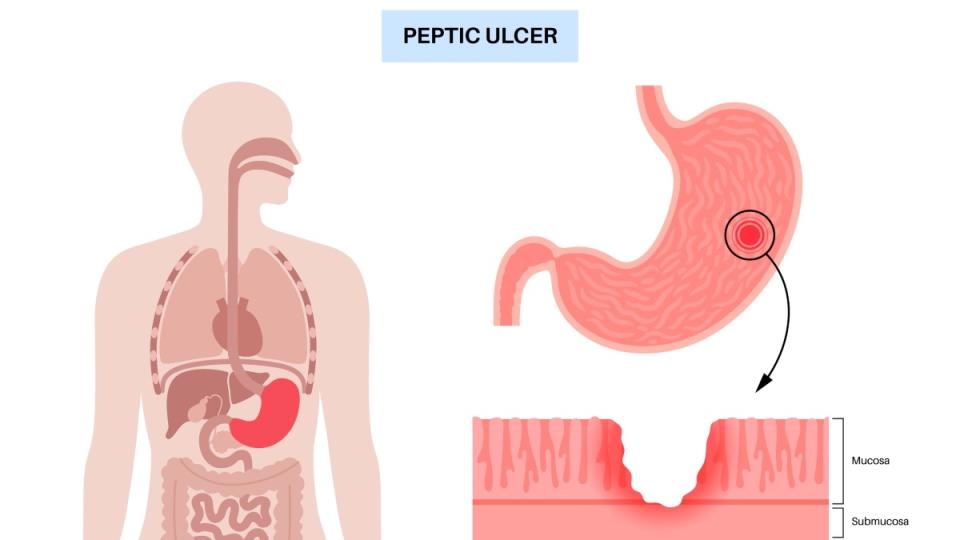
“Stomach ulcers are basically when the lining of the stomach becomes damaged,” explains Lance Uradomo, MD, MPH, an interventional gastroenterologist at City of Hope Orange County in Irvine, CA. Instead of a normal, smooth stomach lining, there’s an indentation (almost like a divot). The problem is that this indentation can cause pain and other issues like bleeding and swelling, he says.
Ulcers, which are sometimes referred to as peptic ulcers or duodenal ulcers, typically occur in two places: The stomach, of course, or in the duodenum, which is the “first part of the intestine, just after the stomach meets the intestine,” explains Dr. Uradomo.
They affect upwards of 6% of the population, which translates to some 20 million people. But on the upside, “they’re actually becoming less common than they used to be,” says Dr. Uradomo. That’s in part because experts have a better understanding of what causes a stomach ulcer, he says.
The 2 top stomach ulcer causes
Typically, a stomach ulcer has one of two main causes:
1. NSAIDs (non-steroidal anti-inflammatory drugs)
You know these as over-the-counter (OTC) pain relievers like ibuprofen, naproxen and aspirin. “These medications can irritate the stomach lining and increase the risk of developing ulcers,” says Lauren Bleich, MD, MPH, a gastroenterologist with Gastro Health in Acton, MA. Worth noting: NSAIDs can be an ingredient in multi-symptom cold medications, too, says Dr. Uradomo.
Part of the issue with NSAIDs is that there’s no clear-cut definition of what amount or frequency can cause an ulcer. As Dr. Uradomo explains, “In general, we say the more you take, the more likely you are to have a problem. But an ulcer can occur with any dose.”
Since people don’t always track their NSAID use, it can be tough to gauge how much they’re taking, says Natasha Chhabra, MD, a gastroenterologist at Gastroenterology Associates of New Jersey. “If they mention to you that [they’re] taking it multiple times a week, every week, then you get a sense of frequent use,” she says.
Corticosteroids like prednisone, an anti-inflammatory often used for arthritis, can also promote ulcers, especially when it’s used with NSAIDs, says Dr. Chhabra.

2. H. pylori (Helicobacter pylori)
This is a type of bacteria that lives in the stomach. It has “a special ability to protect itself from the acid in the stomach, so it can survive in a very inhospitable environment — a very acidic situation,” says Dr. Uradomo. About 36% of people in the US have it. “It’s typically a chronic infection. Many people acquire it early in life, but it doesn’t lead to problems or symptoms until they’re adults.”
It’s not yet known exactly how H. pylori is transmitted. “Factors such as crowded living conditions and exposure to contaminated food or water may contribute to the spread of H. pylori,” says Dr. Bleich, who also notes that infections tend to be more common in developing countries.
Additional stomach ulcer causes
Excessive alcohol use and smoking can also be risk factors for stomach ulcers, as can certain conditions like Crohn’s disease. Genetics may play a role, too. “We do take into account family history,” adds Dr. Chhabra.
Rarely, stomach ulcers may point to cancer. Sometimes, the cancer looks like an ulcer instead of a tumor, Dr. Uradomo says. That's why it’s important to get checked out, especially if you’re experiencing other symptoms like weight loss, vomiting or bleeding.
Stress and diet are not stomach ulcer causes
“Stress and diet, previously thought to trigger ulcer formation, do not put patients at increased risk,” Dr. Bleich reveals. The symptoms of stress and ulcers can overlap, which may mistakenly lead people to think they’re dealing with an ulcer.
"We have all experienced stomach cramps, nausea or stomach issues with stress,” says Dr. Uradomo. “I’m not saying that the GI tract and the brain are not connected — they certainly are — but that won’t cause the actual tear or disruption in the lining of the stomach.”
Symptoms of a stomach ulcer
Abdominal pain is usually the most prominent sign. “It’s typically upper abdominal pain, above the belly button,” says Dr. Uradomo.

You may also have burning or gnawing pain, nausea, vomiting (particularly after meals or on an empty stomach), bloating and loss of appetite, says Dr. Bleich. “Others can experience indigestion, including symptoms such as bloating, belching and heartburn,” she adds.
Take note of dark or tarry stools, which could be a sign of a bleeding ulcer, Dr. Bleich says. “If you notice your stools are black, you should contact your healthcare provider,” she advises.
Anemia, especially iron-deficiency anemia, may also be a sign of an ulcer. “If you’re doing a routine blood test with your doctor and they tell you you’re anemic, the source of that could be an ulcer that’s releasing blood,” says Dr. Uradomo. That’s particularly true if you’re post-menopausal. Since anemia is often related to menstrual blood loss, if post-menopausal women have a sudden drop in blood count, it’s a good idea to be evaluated for an ulcer, he says.
Related: Doctors Say These Kitchen Staples Speed Healing of a Painful Skin Ulcer
Stomach ulcer causes: How to diagnose them
If you’re experiencing symptoms, talk to your doctor. You can start with your primary care physician or go directly to a gastroenterologist. Dr. Uradomo stresses that because of the concern for cancer, if you’re over 50 and have any new, unexplained abdominal pain, you should get checked out.
Testing-wise, the gold standard for ulcer diagnosis is an endoscopy, says Dr. Uradomo. There are also tests to check specifically for H. pylori, including a stool and breath test.
If you do have an ulcer, you’ll be put on a course of medication. Typically, it will be a proton pump inhibitor (PPI), a type of medicine that helps decrease stomach acid. You’ll often start to feel better within days, says Dr. Uradomo. For ulcers that stem from H. pylori infections, you’ll usually be given antibiotics plus a PPI, since it’s a “pretty resilient bacteria,” he says.
How to prevent stomach ulcers caused by NSAIDs
Research shows taking PPIs along with NSAIDs can help protect against ulcers, says Dr. Uradomo. That’s why if you regularly take NSAIDs for conditions such as rheumatoid arthritis, for example, you should talk to your doctor about whether or not you should also be on a PPI, he says. The same holds true if you’re on corticosteroids, since that can also increase your risk of ulcer formation.
Want to avoid NSAIDs altogether? Talk to your doctor about specific alternatives for your situation, Dr. Uradomo advises. For instance, you may consider switching to acetaminophen. “Acetaminophen (Tylenol) is safe for the stomach,” notes Dr. Uradomo.
How to prevent stomach ulcers caused by H. pylori
To ward off painful ulcers caused by this troublemaking bacteria, try these simple tips:
1. Wash your hands
We know you’re already doing this, but it bears repeating. “The route by which infection occurs remains unknown, but person-to-person transmission of H. pylori seems most likely,” says Dr. Uradomo. That’s why practicing good hygiene, like washing your hands and making sure your drinking clean water, can help. Also smart: “While there are no national guidelines for this, household contacts of people with H. pylori can consider getting tested,” advises Dr. Uradomo.
2. Sprinkle some cinnamon

Animal studies suggest that cinnamon may help prevent certain types of ulcers, says Dr. Uradomo. “Cinnamon has been used in many traditions for its healing effects," he explains. "Modern scientists think it has antioxidant and anti-inflammatory effect."
Cinnamon can also help alleviate an H. pylori infection when taken alongside medication. The proof: A study in the Journal of Herbmed Pharmacology found that folks given antibiotics and cinnamon extract saw a decrease in symptoms such as nausea, vomiting, and diarrhea.
3. Sip tea and honey
Research in Diagnostic Microbiology and Infectious Disease found that those with H. pylori infections who had black or green tea and/or honey just once a week saw a significant decrease in the bacteria compared those who didn’t.
Note: Dr. Bleich says natural treatments like tea and honey are helpful, but don’t necessarily get rid of the bacteria completely. “Studies have shown that while these treatments reduce the number of bacteria in the stomach, they fail to permanently eradicate the bacteria,” she explains. Her advice? Talk to your doctor to see if natural remedies can be used in conjunction with medication.

Related: Does Green Tea Help With Bloating? Yes! Plus, It Speeds Weight Loss + Helps Blood Sugar
4. Spoon up yogurt
The creamy snack is rich in beneficial bacteria known as probiotics, which are vital for GI health. “Probiotics help maintain the normal balance between good and bad gut bacteria,” explains Dr. Bleich. “According to one study, taking probiotics before or after standard H. pylori treatment — antibiotics — may improve treatment rates.” (Learn how to make your own probiotic-rich yogurt, which is also a top natural treatment for SIBO.)
Additionally, research in the American Journal of Clinical Nutrition found that those who ate yogurt with the probiotics lactobacillus and bifidobacterium saw a reduction in H. pylori in about six weeks. Two options to try: Siggis or Activia, which have both strains of the probiotics.
For more ways to treat — and prevent — common GI bothers:
These Home Remedies Help Stop Burning Stomach Pain in Its Tracks, Doctors Say
These 4 Gut-Friendly Sweeteners Satisfy Your Sweet Tooth Without the GI Upset
MD: Your ‘Heartburn’ May Be Caused By *Low* Stomach Acid — The Easy At-Home Test and Cure
This content is not a substitute for professional medical advice or diagnosis. Always consult your physician before pursuing any treatment plan.

