IUD placement can be painful. These women used their phones to record it.
As Nicole Marpaung lay on an exam table, the 22-year-old turned on her phone camera to record the experience of getting an intrauterine device, or IUD. In the video, a clinician tells her to expect “lots and lots of pressure.”
Marpaung grimaces and cries in pain: “Oh! Ow, ow, ow, ow, ow ow!”
Marpaung, of Estill Springs, Tenn., is one of numerous women who have posted TikTok videos documenting their distressed and pained reactions during insertion of the birth control device. Although women have been talking about IUD pain for years, the complaint has become more prominent as younger IUD users make the case on social media that women are not given adequate options to manage their pain.
Researchers at Duke University recently analyzed the top 100 TikTok videos with the hashtag #IUD. They found that when users shared details of their experiences, most of them focused on the pain and other side effects of the procedure.
Jenny Wu, an obstetrics and gynecology resident who led the research, said the findings shed light on the gap in pain management.
“It’s just really heartbreaking to me when patients feel like they went through some traumatic experience getting a really great form of birth control,” Wu said.
The American College of Obstetricians and Gynecologists (ACOG) acknowledged in an opinion eight years ago that IUD insertion “is painful for many women.” In January, the organization reaffirmed the 2016 opinion, which notes that research has not demonstrated “an effective strategy to mitigate this discomfort.”
Research also shows that physicians and other providers underestimate women’s pain during IUD insertions. In a study of 200 women, most of whom had given birth, the women reported an average maximum pain score of nearly 65 on a scale of 0 to 100.
The providers, however, rated the women’s pain at about 35.
Local anesthetics, sedation and other options are available for IUD placement, but many clinicians do not readily offer them. Physicians said that determining the best pain control can be difficult because women’s preferences and experiences vary, and there are not enough effective options or guidelines on when to use them.
- - -
Unprepared for pain
Before her IUD procedure in 2021, Marpaung had been told it would be uncomfortable, but not painful. She said she was not offered pain-control options or advised to have someone drive her home.
After the procedure, Marpaung was still in intense pain and asked workers at a nearby restaurant for ibuprofen. Then she walked next door to a sporting goods store and sat on the toilet “because I didn’t know what else to do. It hurt so bad.”
“The disbelief that I had to go through that, and there was no warning - it just disgusts me,” Marpaung said.
Merrily Ruetsche also was not prepared for her IUD insertion in March 2023. She said she was told to expect cramping, but was instructed not to take ibuprofen beforehand because it can increase bleeding risk. No alternative pain-control options were discussed, she said.
Minutes into the procedure, Ruetsche said she “felt instant regret.” In a video after it was over, she describes the pain as “horrible,” “terrible” and “awful.”
“I had an urge to kick the doctor. I didn’t. It’s just an instinct I had because it was so painful,” said Ruetsche, 26, of Carpentersville, Ill. She said she wanted other women to be better prepared.
Why pain management often isn’t discussed
The percentage of women ages 15 to 44 who had used an IUD almost tripled from 7.7 percent in a 2006-2010 survey to 21.4 percent in a 2015-2019 survey of sexually experienced women, data shows. IUDs have become an increasingly popular contraceptive option for younger women and teens because evidence shows IUDs are safe and highly effective for them, and are more reliable than remembering to take a daily pill.
The problem, physicians said, is that the demographics of the women interested in getting IUDs has changed, but pain-management approaches have not.
In the past, IUDs were recommended mostly for women who had given birth because they were believed, incorrectly at that time, to be dangerous for young women and those who had never given birth, said Eve Espey, chair of ACOG’s Contraceptive Equity Expert Work Group. That may have skewed the pain scores as IUD insertion often is less painful for women who have delivered vaginally, Espey said.
In one study, nearly 8 out of 10 women who had never given birth reported moderate to severe pain with IUD insertion.
Some women who have delivered vaginally experience pain, too. One smaller study showed that women who had given birth reported a median pain score of 5 out of 10, vs. 7 for those who had never given birth.
ACOG is considering new guidance for pain management of in-office gynecological procedures, including IUD insertions, though a spokeswoman didn’t have further details about which pain-management options are being considered.
“Physicians are left without a clear direction,” meaning some patients may not be offered any pain-control options, said Lauren Kus, a complex family planning fellow at Mount Sinai Hospital. “I think trivializing or failing to address pain associated with IUD insertion undermines the physician-patient relationship at best and can actually traumatize patients at worst.”
- - -
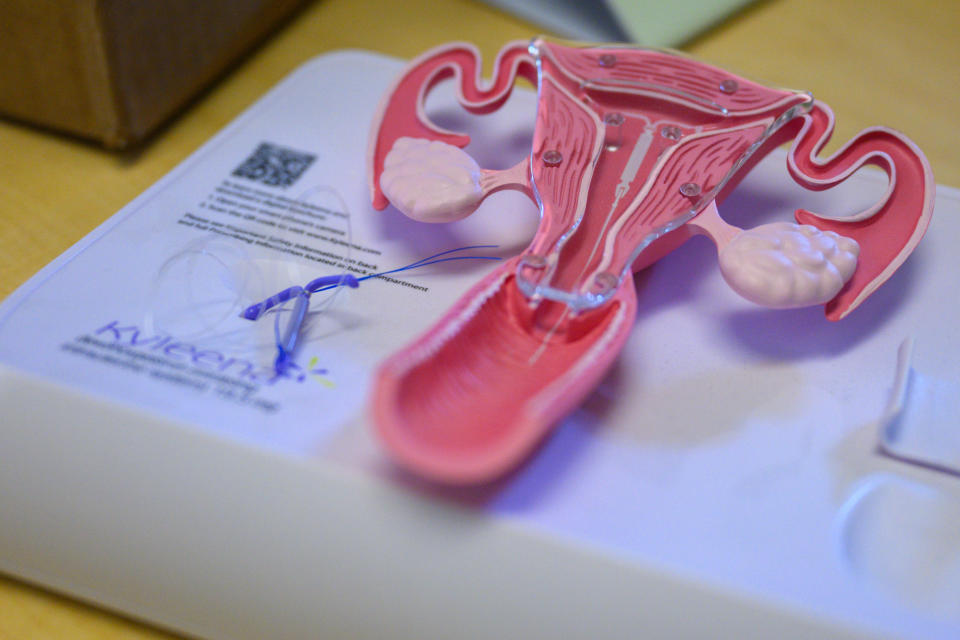
How IUDs are placed
An IUD is a small, T-shaped device that is inserted through the cervix into the uterus. During the procedure, which usually takes less than about five minutes, a clinician inserts a speculum into the vagina and uses a tenaculum, a type of forceps, to hold onto and stabilize the cervix, which can cause pain and some bleeding.
Women also experience pain when a small probe is inserted to measure the uterus. Placement of the IUD in the uterus can then cause severe cramping and dizziness, according to patients and physicians. Some women also continue to experience discomfort and cramping in the days after the procedure.
Often, over-the-counter anti-inflammatory medications such as ibuprofen are the only recommended option for pain.
Other options include numbing agents, such as a lidocaine spray or gel, or a lidocaine injection in the cervix called a paracervical block. Misoprostol, a medication that helps soften the cervix, may also be used.
But research shows that topical lidocaine, misoprostol and most anti-inflammatory drugs do not reduce pain. Some studies show paracervical blocks do not help while others have shown a benefit, but some physicians said women are hesitant to have injections in the cervix because they can be painful.
And misoprostol is not recommended for routine IUD insertions because it does not usually help with pain and can cause cramping and gastrointestinal issues, said Katherine Pocius, medical director of family planning at Massachusetts General Hospital.
Oral or intravenous sedation can be used for pain control, physicians said, but it can be expensive and require an escort home.
General anesthesia is rarely considered because it carries risk and requires special equipment and the presence of an anesthesiologist.
Some physicians said anti-anxiety medications such as Xanax or Valium can help reduce anxiety before the procedure. Studies have shown that anxiety leading up to the procedure, concerns about and anticipation of pain and negative perceptions of IUDs may lead some women to feel increased pain.
“As providers, our job is to take our patients’ concerns about IUD pain seriously and individualize care in the context of shared decision-making,” Monica Dragoman, director of the complex family planning division at Mount Sinai Health System, said in an email.
- - -
Phone videos of IUD procedures
Bridget, 22, who asked not to use her last name for privacy reasons, said she experienced “the worst pain of my life” during her first IUD insertion at 16. Years later, when she told clinicians about the experience, they downplayed it, saying the second time would not be as bad. She said she asked for but was not offered any pain-control options other than ibuprofen, “which did nothing.”
Bridget, who lives in New Jersey, said she wondered if she had misremembered the agony she felt as a teen. So she used her phone to record the procedure in 2022. The video shows Bridget scream, “Oh, my God! Ow!” as she bursts into tears.
“Settle down. You’re okay,” a clinician tells her.
As clinicians continue to work, she cries out again. “It hurts! Why does it still hurt?” she shouts. “It hurts. It hurts.”
She said she felt a sharp, stabbing pain like her insides were “about to pop open.”
Bridget said she still believes IUDs are a good option, but she wants women to know how painful it can be without adequate pain control. She has since found a gynecologist who is willing to use anesthesia for future IUDs, she said.
- - -
Listening to women
A video shows Mallory Tatman, 26, of Houston, writhing on an exam table and moaning in pain during her procedure in 2022.
She said she felt a long, intense abdominal pain that shot down her legs, making her jolt back on the table. “I was biting my lip, hoping it would be over soon,” she said. “I was trying not to cry.”
The procedure was so painful, she said, she decided to post the video to warn others.
When Savannah Watson, of Woodruff, S.C., got an IUD in February 2023, it was “excruciating,” she said.
The 25-year-old stays composed in her video, but she said that the insertion felt like “getting punched and stabbed in the uterus at the same time” and that she nearly passed out from the pain, even after taking ibuprofen as directed. “It was like the worst period cramps of your life where they completely take you out and you’re lying in the fetal position in bed,” she said.
Although research and pain-control options are limited, physicians said clinicians should work with their patients on ways to minimize pain. Women should ask about pain-control options before the procedure and look for another provider if their concerns are not addressed.
“I really hope that we are listening to patients and responding when we hear that there are so many videos on TikTok,” about negative IUD experiences, said Espey, chair of the OB/GYN department at the University of New Mexico. “It’s important that we listen and make sure that patient-centered outcomes really guide both the research we do and the way we practice medicine.”
Related Content
Abortions outside medical system increased sharply after Roe fell, study finds
Putting chaplains in public school is the latest battle in culture wars
After voting to legalize weed, Marylanders are mixed on impact, poll finds