He went to get medication for ADHD. MercyOne charged him nearly $1,500 in facility fees.

Colby Grabill only recently started to grasp the link between his untreated ADHD and depression, and was referred by his physician to a MercyOne psychiatrist last year to get medication to help.
He said he went to three appointments from July to October at the hospital’s behavioral health center in Des Moines ― the first for about a half hour, the others lasting about 10 to 15 minutes.
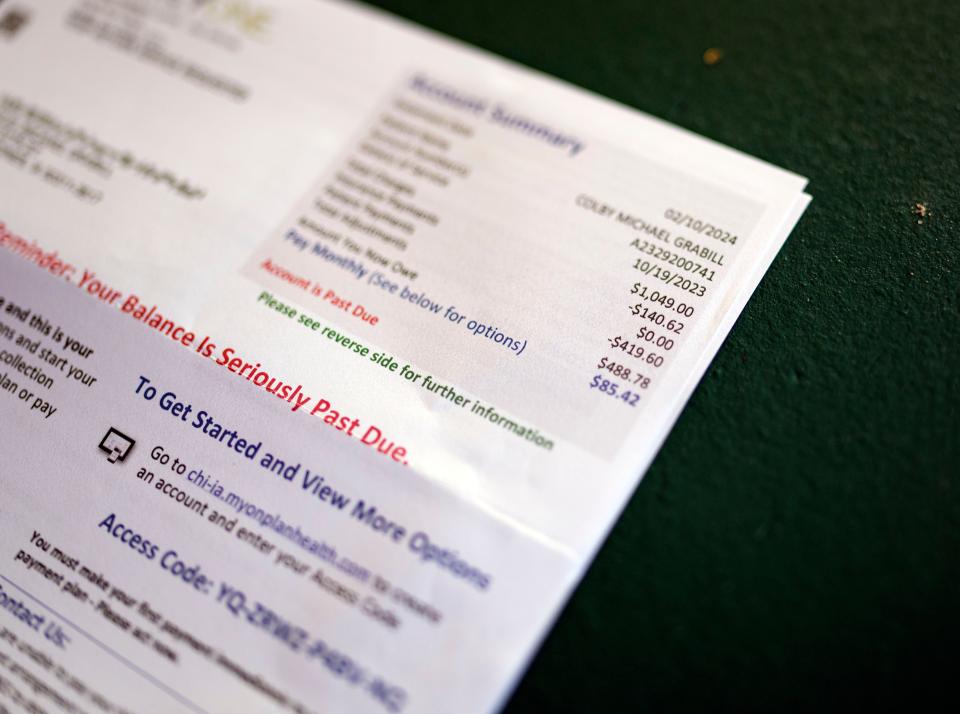
When the 35-year-old father of six finally got bills for those visits, he said, he thought surely there’d been a mistake. Cigna Healthcare paid all but $20 of the $150 doctor bill for each visit, but Grabill was told he was personally responsible for paying $488.78 in hospital facility fees to MercyOne for each visit. For all three visits, the amount due was $1,466.34.
More: Biden is targeting the ‘junk fees’ you’re always paying. But it may not save you money.
“At first, I was in a little bit of a panic, but I just thought it was an error. Something must have gotten screwed up,” he said. “By the time I realized this was legitimate, I was just flabbergasted. I couldn’t believe they could charge me that much.”
The sticker shock that caused Grabill and his wife to contest the bill with MercyOne is being felt across the country.
Hospital facility fees increase dramatically for variety of care
While federal regulations have long allowed hospitals to charge patients a facility fee to offset the cost of providing care, those fees have been increasing dramatically and have expanded from emergency rooms to outpatient clinics, online telehealth visits, surgery centers and off-campus doctor’s offices owned by hospitals and their health systems, health care research has shown.
From 2004 to 2021, facility fee charges increased by 531%, according to an analysis of industry data from the Peterson-KFF Health System Tracker, an online information hub that monitors and assesses the performance of the U.S. health system. That was four times faster than increases to professional fees for emergency department evaluations and management services, which rose 132% during the same span.
Hospitals have said facility fees are needed to provide round-the-clock care to patients, regardless of their ability to pay, and that they pay a high price to provide that care.
The American Hospital Association says overall median hospital operating margins were negative through 2022 and into the beginning of 2023, and Medicare pays only about 84 cents on the dollar for the cost of care provided to beneficiaries.
But facility fees also have become a big reason why consumers are finding it increasingly difficult to pay their medical bills. The fees can far exceed those for the care itself and often aren’t covered by insurance. Especially vulnerable are those who need to meet high deductibles before insurance starts to cover some of the bill.
Grabill said he signed a form all patients are required to sign before his visits saying he would pay for his medical care. But he wasn’t told ahead of time about the facility fees ― or that other providers not under the hospital's ownership could render the same service without those fees.
Specifics on facility fees not readily available from Iowa's largest providers
A federal rule that went into effect in January 2021 requires all hospitals operating in the United States to provide clear, accessible pricing information online about the items and services they provide. The goal was to make it easier for consumers to shop and compare the cost of care before going forward.
More: Hidden hospital prices harm patients: Can this new pricing tool make a difference?
But getting hospitals to comply with that rule, which is poorly enforced, has been an issue across the country, numerous media outlets have reported.
MercyOne, UnityPoint Health and the University of Iowa Hospitals & Clinics, Iowa’s largest medical providers, declined to provide Watchdog with a list of their facility fees or to say where those fees aren’t charged. They also did not respond to a question about whether they post anywhere online how much facility fees will be at hospital-owned providers.
Watchdog checked websites for all three and found that while fees for some individual services are disclosed, facility fees are not.
Neither Eve Lederhouse, listed online as MercyOne's communications director, nor Todd Mizener, its public relations manager, responded to several calls and emails related to the facility fees.
MercyOne’s website refers people to its insurance and Medicare handbooks to learn what’s covered and what’s not. It has an online price estimator, but the link doesn’t work for Des Moines.
UIHC tells people they will be charged facility fees for rooms, equipment, tests and labs, but it doesn’t say how much those fees are. Instead, it tells consumers online to review their health plans or call their insurers.
Kevin Kirkpatrick, spokesman for UnityPoint Health, sent Watchdog a statement saying the company provides services and tools that make it easier for patients to understand their costs, pay their bills, learn about coverage options or get financial assistance when needed.
But nothing on its webpages details the amounts of facility fees, and those fees ― included in the price of procedures ― aren’t included in its self-service cost estimator tool.
The Iowa Hospital Association has a service online called Hospital Charges Compare, but that provides only data based on average charges for procedures and services. It’s based on what’s coded for claims processing.
When asked about facility fees, Craig Borchard, the association's vice president of communications, said that "if 'facility fees' means charges for an inpatient or procedure room, you’d have to get that from the hospitals."
Advocacy group: Voters want clear information on medical charges
Voters are in favor of requiring transparency in medical billing, eliminating facility fees and mandating uniform prices for service, regardless of where a patient seeks care, according to the Washington, D.C.-based national research and affordable health care advocacy organization United States of Care.
A 2023 poll for the group found 74% of voters supported banning facility fees everywhere for outpatient, same-day services, and 81% wanted medical providers to disclose their facility fees upfront to patients, before they are treated. The poll was conducted by Morning Consult and had a reported margin of error of plus or minus 2 percentage points.
In December, the U.S. House of Representatives passed the bipartisan Lower Costs, More Transparency Act, which would require that hospitals, insurance companies, and other health care facilities publicly list the prices they charge patients. The bill also includes a reform that would require the same price for drug administration under Medicare at an outpatient setting. The policy, known as “site neutral payment,” has been opposed by organizations like the American Hospital Association.
Committees in the Senate, meanwhile, also have discussed banning facility fees and instituting site-neutral payment reform.
“There’s a constellation of activity happening, and pretty remarkable progress,” said Lisa Hunter, senior director for policy and external affairs at United States of Care.
In an interview with watchdog, Hunter said hospitals have been buying up independent doctor practices and outpatient services at a rapid pace because Medicare for years has allowed upcharges for services at hospitals’ off-campus facilities.
United States of Care's research found that when a hospital acquires an independent physician’s practice, the prices patients pay increase on average 14%.
“There’s other research on this with cancer patients or those who receive IV drugs” at outpatient clinics, Hunter said. “They are hit with 20% more of an out-of-pocket cost. The differential in what is being charged is outrageous.”
In the meantime, several states have passed measures aimed at controlling facility fees.
“Some states are banning facility fees for things like preventive services, or some have for telehealth,” Hunter said. “Some states are wading in a little more delicately because the data around this is very uneven and highly variable depending on where you are.”
In recent years, no one in the Iowa Legislature has taken any steps to limit or eliminate facility fees, or to make them more transparent to health care consumers, she said.
Grabill said he and his wife are still waiting to see what MercyOne will ultimately do about the facility fees the health system tried to charge him. He said his bills have been resubmitted to the hospital for review.
Officials from Iowa's Department of Insurance said they would acquaint Grabill with another new federal law, the No Surprises Act, which prevents insurance companies from forcing consumers to pay too much for unexpected bills in some circumstances.
The act, which went into effect in 2022, protects patients from surprise bills for covered emergency out-of-network services, including air ambulance services (but not ground ambulance services) and for covered non-emergency services at an in-network facility. It also protects patients from surprise bills from a facility, such as a hospital or freestanding emergency room, or a provider, such as a doctor, for in-network coinsurance, copays, or deductibles for emergency services, even if the facility or provider is out-of-network.
Grabill said he would have shopped around had he known three simple visits were going to cost him so much.
"I can't believe they are just dumping these huge costs on people," he said. "I don't know how people are tolerating this. ... I'm still not OK with paying it."
How to fight facility fees
Before you see a new provider, ask your insurer if it covers facility fees. If so, ask what portion of those fees will be covered and how much you will be responsible for paying.
When your doctor refers you to a new provider or specialist, ask whether the provider is hospital-owned or works for the same hospital health system.
More: Worried about what you'll pay for hospital care? These tips may help you get a better deal
When you make an appointment, ask whether you will be charged a facility fee. If there is one, ask if there is another location where you can go where a facility fee isn't charged. Some doctors may practice at a location that doesn't charge one.
It's difficult to fight facility fees because they are legal in most places. But you can always talk to the health care provider about waiving or lowering the fee. You can also appeal to your insurer to cover more of the cost.
For more about the No Surprises Act, go to iid.iowa.gov and search for No Surprises Act.

Lee Rood's Reader's Watchdog column helps Iowans get answers and accountability from public officials, the justice system, businesses and nonprofits. Reach her at lrood@registermedia.com, at 515-284-8549, on Twitter at @leerood or on Facebook at Facebook.com/readerswatchdog.
This article originally appeared on Des Moines Register: What are facility fees? They can drastically increase doctor bills.

