Campaign heats up to make heroin-overdose reversal drug available everywhere
Jennifer Plumb, MD, was driving through downtown Salt Lake City with her son in tow when she saw a woman lying face-up on the sidewalk. She parked her car and got out, pushing her way through the commotion. The woman’s skin was turning blue and her pupils were as small as pinpoints — “a hallmark sign of an opioid overdose.”
Plumb, who is an assistant professor of pediatrics at the University of Utah and has spearheaded the campaign to make naloxone kits more readily available to Utahans, had just come from a naloxone training session with a local fire department and happened to have the opioid-overdose reversal drug in the trunk of her car. Moments later, she was sinking the needle into the woman’s arm. Plumb waited. Then she injected a second dose a minute later. The woman immediately sat up. “Where are my sunglasses?” she asked the small group of people that had now circled around her.
“It’s really bizarre, to be honest,” said Plumb. “Naloxone is sometimes called the Lazarus drug, because it really feels like you’re raising someone from the dead.”
Plumb has a personal connection to the debilitating addiction. Her brother overdosed on heroin 20 years ago, his friends leaving him dead in a basement. A paramedic on the scene said to Plumb at the time, “I wish he would have had naloxone.” The comment has remained burned in her memory.
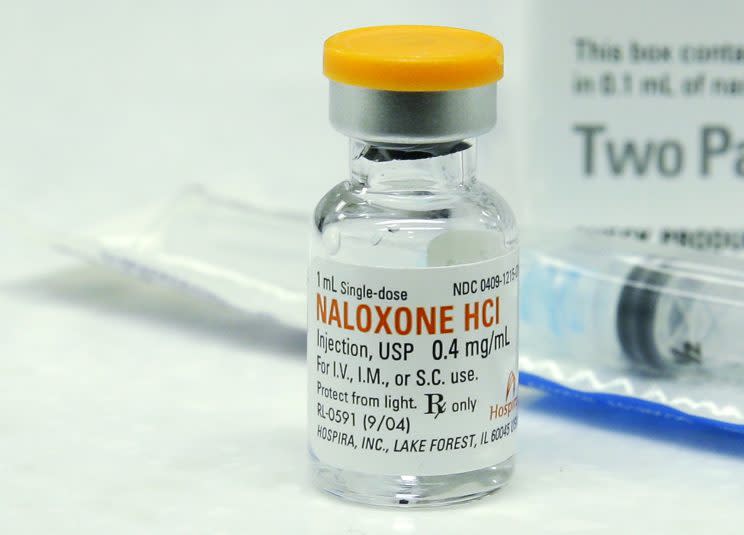
Naloxone, sold under the brand names Narcan and Evzio among others, is a medication that reverses the effects of an opioid overdose. Patented in 1961 and approved by the FDA in 1971, the drug is not addictive and most commonly administered intravenously, though a more user-friendly nasal spray is now available.
As the opioid addiction crisis has exploded throughout the U.S., experts across the country are working to make naloxone more readily available to the public — to law enforcement, fire fighters, first responders, departments of health, local school districts, colleges, community-based organizations and homeless shelters. “No area of this country is safe from this epidemic,” said Plumb, whose home state ranks seventh highest in the nation for the rate of opioid overdose deaths.
While the FDA technically requires a person to obtain a prescription for the drug, the majority of U.S. states now allow a person to purchase naloxone from a pharmacist without one. Over the past year, CVS and Walgreens, among other pharmacy chains, have also expanded over-the-counter availability of the reversal drug.
Some critics have pegged naloxone as a Band-Aid to a much more complex issue, dismissing naloxone’s accessibility as an excuse for opioid users to continue using. But most experts, while trying to get a handle on the crisis, praise the expanded efforts, especially on the heels of a new CDC review that found heroin-related overdose deaths have more than quadrupled since 2010.
Opioids, both prescription medications and street drugs like heroin, now are the leading cause of accidental death in the U.S., killing more than 33,000 people in 2015, more than any year on record, according to the CDC. About half of those deaths involved prescription opioids. That number surpasses HIV/AIDS deaths in 1995, at the peak of the AIDS epidemic.
“Naloxone isn’t going to cure this crisis, but until we get a better grip on getting people the help they need, it’s acting as the proverbial fire extinguisher,” said Plumb. “Having greater access will also inspire a lot of dialogue in school about drug use as well.”
When she co-founded Utah Naloxone to coordinate the purchase and handout of naloxone kits nearly two years ago, Plumb said she expected heavy pushback, because of the stigma attached to heroin use. She armed herself with the proper research and arguments to explain to other community leaders why naloxone access is important. Unexpectedly, her pitch was met with “nothing but open arms.”
“It’s an undeniable issue at this point, so everyone said, ‘Yes, let’s do something,’” she said.
In fact, the rate of naloxone kit availability has increased exponentially in the last two decades, with state and city governments all over the U.S. seeking to obtain them and provide them free for residents. In 2015, the Harm Reduction Coalition, a national advocacy and capacity-building organization, surveyed 140 managers of organizations in the United States known to provide naloxone kits to laypersons. From 1996 through June 2014, the surveyed organizations provided naloxone kits to 152,283 laypersons and received reports of 26,463 overdose reversals.
The continued overprescribing of opioids has led to excess availability, said John F. Kelly, MD, director of the Recovery Research Institute at Harvard Medical School, and the idea that these pills are prescribed leads to a dangerous belief that they are safe.
In the last few years, opioid makers have sought to create abuse-deterrent properties, meaning the pills are designed to prevent crushing into powder for swallowing, snorting or injecting. Some say these new pill traits have been one of the factors that have forced people to seek alternative drugs, like heroin, which offer a high without such barriers at a much cheaper price. Still, even with the industry changes, in 2013 the FDA approved Zohydro, a timed-released hydrocodone painkiller that does not have an abuse-deterrent property.
Many doctors are now prescribing naloxone when they prescribe an opioid, and in 2014, the FDA approved Targiniq ER, an extended release oxycodone opioid combined with naloxone. The naloxone blocks the euphoric effects of oxycodone, making it less liked by abusers than oxycodone alone. Purdue Pharma, also the maker of Oxycontin, manufactures the drug.
In a statement, the FDA told Yahoo News, “The FDA is committed to looking at all facets of this complex issue, including encouraging informed and appropriate prescribing of opioids, encouraging the development of alternative pain medicines that are not addictive, advancing technologies that may make it more difficult to abuse prescription opioids and supporting the development and review of additional options for medication-assisted treatment and the life-saving overdose medication, naloxone.”
To date, Adapt Pharma, the manufacturer of Narcan, has supplied free of charge more than 3,000 doses of Narcan Nasal Spray, which was approved by the FDA in 2015, to high schools in 32 states, including statewide programs in Pennsylvania, Kentucky, and Connecticut, which are among the states hardest hit by the heroin epidemic. The needle-free option makes many people without a health care background more comfortable administering it.
“The stigma associated with drug use and addiction is a major barrier inhibiting our country from fully addressing the opioid epidemic,” said Thom Duddy, executive director of communications at Adapt Pharma. “By increasing naloxone availability, we are providing a potentially life-saving solution to countless Americans who are close to someone or are themselves currently facing addiction and vulnerable to an opioid-related overdose.”
Right now, Plumb said the U.S. is faced with a complex and multilayered problem related to opioids, and while experts and law enforcement work to unravel its causes and horrors, naloxone offers second chances to thousands who have gotten swept up in the drugs’ path.
“We have a prescriptionized, medicalized generation of opioid users,” said Plumb, “so while we’re getting those people the recovery services they need, we also have to create preventive measures so that a new generation coming up does not see that same access and excess.”
Read more from Yahoo News:
Sean Spicer spars with White House press corps over wiretapping
How an L.A. House district’s special election could mark a new direction for Dems
Health care fight raises concerns about Paul Ryan’s leadership
Cuts to poverty programs are ‘as compassionate as you can get,’ Trump budget chief says
Photos: Man killed after trying to grab soldier’s gun at Paris airport



