Symptoms That May Signal Early Colon Cancer
Not Everyone Is Symptomatic in the Beginning
Medically reviewed by Robert Burakoff, MD
Diagnosing colon cancer early is important so that it can be treated most effectively. Paying attention to any possible symptoms is key. While there may be symptoms of early colon cancer, sometimes there aren’t.
Early symptoms can be vague and nonspecific, such as changes in bowel habits (frequency, volume, consistency, color, control of defecation) or blood in the stool.
See a healthcare provider if you notice any changes in your bowel habits or any symptoms that don’t feel right. These can be symptoms of various ailments, and getting an appropriate diagnosis and subsequent treatment as soon as possible helps with the likelihood of positive outcomes.
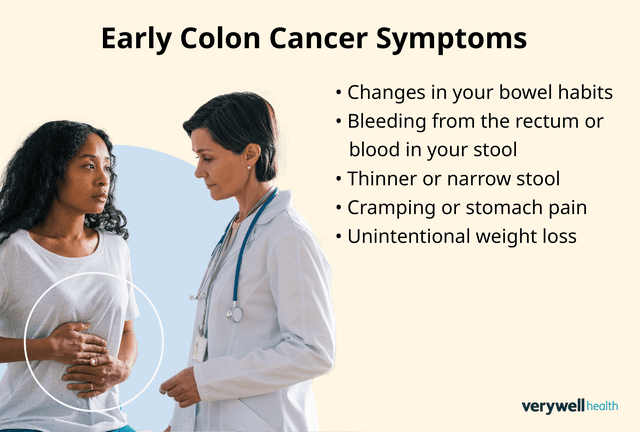
Photo composite by Tara Anand for Verywell Health; Getty Images
Early Colon Cancer: Symptoms to Know
People tend to use the terms symptoms and signs interchangeably, but they have different medical definitions. Symptoms are things you feel in your body, and signs are changes that can be measured, like blood work numbers or blood pressure.
Very early colon cancer is typically asymptomatic (doesn’t have any symptoms), which makes regular screening extra important.
Colon cancer usually arises from a polyp—a clump of cells. Many polyps are not cancerous, but even for cancerous polyps, they can take 10 to 15 years to turn into cancer. It then takes time to grow and spread, causing symptoms.
However, symptoms can occur, and it’s important to be aware of them. These symptoms might also indicate other conditions. If you have any symptoms, see a healthcare provider.
Colon Cancer and Young Adults
The incidence of colon cancer is rising in young adults. They’re more likely to ignore symptoms that may indicate disease, which leads to later diagnosis and treatment. Don’t put off seeing a healthcare provider if you notice any symptoms. Early diagnosis and treatment are key for optimal results and a greater chance of survival.
Common in Early Colon Cancer
Symptoms that can occur, especially in the earlier stages of colon cancer, include:
Changes in your bowel habits, such as having more diarrhea or constipation than usual
A feeling that you haven't emptied your bowels completely after a bowel movement
Bleeding from the rectum or blood in your stool
Cramping or stomach pain
Unintentional weight loss
Less Common in Early Colon Cancer
While fatigue may be present in early colon cancer, it’s more likely to show up as time goes on. This is because colon cancer causes bleeding from the rectum or digestive tract. Over time, this blood loss becomes more significant, causing a low red blood cell count (anemia), which causes fatigue.
What If You're Asymptomatic?
As colon cancer progresses, symptoms will eventually show up. But in the earlier stages, there is the chance of being asymptomatic.
If you are at elevated risk for colon cancer because of family history, genetics, or lifestyle factors, talk with a healthcare provider about your concerns. Sometimes, you may be able to be screened for colon cancer based on established risk, but this is not always the case.
Colon Cancer and Overlapping Symptoms in Other Conditions
Many symptoms of colon cancer are similar to symptoms of other conditions, which is why it's so important to see a healthcare provider if you notice any symptoms. They can do an exam, get a thorough medical history, and order any screening or diagnostic tests that can help with an accurate diagnosis.
Other conditions that have overlapping or similar symptoms can include:
Polyps
Screening to Detect Early Colon Cancer
Early colon cancer can often be found or prevented through screenings, which can find and remove polyps before they become cancerous or when they start to become cancerous. Your provider should discuss with you when screening starts based on your age, family history, medical history, and lifestyle.
Certain risk factors indicate that you should start screening at an earlier age and/or have screening more often, and these include:
A personal history of colon cancer
Strong family history of colon cancer or polyps (i.e., in a first-degree relative such as a parent or sibling younger than 60 or two first-degree relatives of any age)
Personal history of inflammatory bowel disease
Family history of any hereditary colon cancer syndrome, including familial adenomatous polyposis (FAP) or Lynch syndrome
The United States Preventive Services Task Force (USPSTF) recommends that people between the ages of 45 and 75 get regular screening. However, they don’t recommend a specific test. For most people of average risk, insurance will cover a colonoscopy every 10 years.
Tests that can be used for screening include:
Colonoscopy: Uses a thin tube with a camera and tools on it inserted through the rectum to examine the entire rectum and colon and also remove polyps
Computed tomography (CT) colonography: Also called “virtual” colonoscopy, it uses CT to produce detailed images of the colon and rectum.
Sigmoidoscopy: This procedure is similar to colonoscopy, but it cannot check the upper part of the colon.
Fecal occult blood test (FOBT) and fecal immunochemical test (FIT): These are tests to find blood in the stool.
Stool DNA test: This test checks the stool for signs of tumor genetic material.
Localized colon cancer, or cancer that has not spread beyond any local tissues to lymph nodes or any distant organs or tissues, has a five-year survival rate of 91%. Localized colon cancer typically refers to stages 0 through 2A.
When to Get a Provider Opinion
So when should you see a healthcare provider?
If you have any chronic bowel issues and notice a change in your bowel habits, blood in your stool, or unexplained bloating or fatigue, it’s worth calling a healthcare provider to see if there’s something that needs addressing.
If you have a family history of colon cancer, polyps, or any hereditary colorectal cancer syndrome, your screening guidelines are likely different than the general population. You should speak with a healthcare provider about when you should get screened, and any signs or symptoms to watch for.
Tell a healthcare provider about your concerns or anxiety about symptoms getting worse or your risk factors. They may be able to provide you with concrete information that may help ease your fears or help mitigate your anxiety.
Can You Lower Your Colon Cancer Risk?
Anyone can get colon cancer, but certain risk factors can increase the likelihood of the cancer developing. However, it’s important to remember that risk factors don’t necessarily mean you will develop cancer; they increase your risk. It’s also possible to develop colon cancer with no risk factors.
Some risk factors that are out of your control include things like:
Older age: Your risk of colon cancer increases as you get older.
Having inflammatory bowel disease (IBD) like Crohn’s disease or ulcerative colitis
Genetic syndromes like familial adenomatous polyposis (FAP) or Lynch syndrome
Talk with a healthcare provider about these risk factors and how they may impact screening for you.
Some other risk factors relate to behavior or lifestyle and can be modified. High-risk lifestyle factors include:
Using alcohol and tobacco
A diet low in fiber and high in fat or a diet high in processed meats
Lack of fruits and vegetables in your diet
Minimal physical activity
Overweight or obesity
If you have one or more modifiable risk factors, talk with a healthcare provider about steps you can take to address your risk and reduce it. Sometimes, you may want additional help, like a nutritionist or a counselor, to help change behaviors and choices.
Summary
Early colon cancer doesn’t always have symptoms, but when they do arise, they are often general and nonspecific, like bloating, gas, or changes in bowel habits. Sometimes, more serious symptoms like bloody stools, significant weight loss, or fatigue may occur.
It’s important to note any changes in bowel habits and see a healthcare provider if you notice anything different about your body or how you feel. Talk with them about when you should start screening for colon cancer, depending on your family and medical history, and what steps you can take to help reduce your risk of developing colon cancer.
Read the original article on Verywell Health.

