R.I. health care spending skyrocketed after COVID. Now it’s coming back down to Earth.

Rhode Island has already seen some success is in reducing inpatient hospital visits by performing the same procedures in outpatient settings. (Courtesy of Lifespan)
Chalk it up to a post-pandemic comedown.
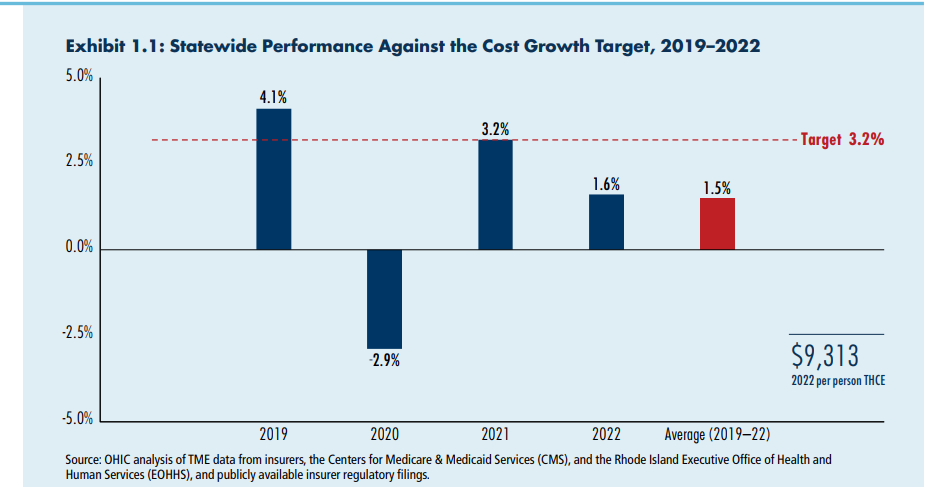
The nearly $9 billion price tag associated with health care spending in Rhode Island in 2022 marks a 1.6% per-person jump over 2021.
That’s half the rate of increase in the prior year, and safely below the 3.2% benchmark set by a state panel focused on tracking health care costs, according to a report published Monday by the Office of the Health Insurance Commissioner.
But like many analyses thrown off balance by the pandemic, the year-to-year comparison on state health care spending doesn’t tell the whole story.
“The COVID years have created a lot of aberrations in data that need to be contextualized,” Cory King, state health insurance commissioner, said in an interview.
Per-person health care spending in Rhode Island fluctuated dramatically in recent years due to the pandemic. (Rhode Island Office of the Health Insurance Commissioner)
Indeed, per-capita health care spending in Rhode Island decreased 2.9% from 2019 to 2020. Pent-up demand spilled over in 2021, as patients flooded hospital rooms and doctor’s offices, eager to complete the elective procedures and routine checkups postponed due to the pandemic.
By 2022, the spike flattened out, with less severe annual spending increases reported by private insurers and government-funded programs, according to the report.
The $8.92 billion in total health care spending reported in 2022 translates to $9,313 per person.
Rhode Island Health Care Spending Trends Public Forum
The Rhode Island Office of the Health Insurance Commissioner and the Rhode Island Cost Trends Steering Committee will host a public forum Monday to talk more about the latest findings in Rhode Island health care spending and how it compares to the rest of the region.
The event is from 9 a.m. to noon at the Crowne Plaza in Warwick. Featured panelists are Cory King, Rhode Island’s health insurance commissioner; Dr. Deidre Gifford, executive director for Connecticut’s Office of Health Strategy; and David Seltz, executive director of the Massachusetts Health Policy Commission.
Beware Big Pharma
King sees trouble ahead, with inflation, provider shortages and expensive pharmaceutical drugs looming over Rhode Island’s health care landscape.
“I expect 2023 spending to be much higher,” he said, adding “it would not surprise me” if the upcoming data shows an annual growth rate above the 3.2% benchmark.
The biggest problem, said King, are drug costs, which are already spiking at alarming rates with little opportunity for relief at the state level, since drug prices are, for the most part, controlled under federal regulations.
“We characterize prescription drug cost growth as a threat to affordability,” King said. “It’s crowding out other opportunities to make investments in delivery in our system.”
In other words, keeping up with rising drug prices from pharmaceutical companies takes money away from government and private insurance companies, and their patients, that could be otherwise spent paying more to attract and retain providers, for example.
State lawmakers are considering a flurry of policies aimed at easing access to, and costs of, prescription drugs. But King was skeptical any state-level policies could stand up to fights by pharmaceutical giants.
“They are going to litigate every single time,” he said.
Outpatient services up
Powerless over drug prices, King stressed the importance of cutting costs elsewhere. One area where the state has already seen some success is in reducing inpatient hospital visits by performing the same services in outpatient settings.
In 2022, inpatient hospital spending dropped 5.4%, while outpatient costs rose 4.4%, according to the report.
The trend was driven by new technology and equipment allowing hip and knee replacement surgeries to be done in an outpatient setting rather than a hospital.

A shift from inpatient to outpatient settings for hip and knee replacements has helped curtail health care spending growth in Rhode Isand. (Rhode Island Office of the Health Insurance Commissioner)
“While these surgeries are among the outpatient services with the highest per unit payment, they cost significantly less when performed on an outpatient basis instead of an inpatient basis,” the report stated.
King named the growth of outpatient care as a prime example of how efficiencies can cut costs without compromising service. Another avenue for potential relief: the resumption of eligibility review for Medicaid patients.
Managing the Medicaid monster
The federal government stopped states from kicking people off government-subsidized health care in 2020 to ensure people could still access critical health services during the pandemic. However, some of those Medicaid patients moved to other states, died, or became eligible for another form of insurance, such as by aging into Medicare.
Per-person spending on Medicaid in Rhode Island increased 3.1% from 2021 to 2022, in part reflecting the continued coverage federal requirement, the report noted. States including Rhode Island began reviewing eligibility in 2023, which may lessen per-person costs in upcoming years if ineligible patients are removed, King said.
Commercial health care costs per person rose 3.3% in 2022, while Medicare costs increased by 1.8%, according to the report.

Rising Medicaid costs remain a concern for lawmakers and policy experts. In 2022, Rhode Island spent nearly $3 billion on Medicaid services. (Rhode Island Office of the Health Insurance Commissioner).
Ballooning costs associated with the state’s Medicaid program, which already eats up a third of the annual budget, are a top concern for lawmakers. At the same time, legislators and Gov. Dan McKee in his fiscal 2025 budget proposal included phased-in increases in fee-for-service reimbursements to certain Medicaid providers, citing the need to bring Rhode Island’s rates up-to-snuff with neighboring states.
King backed the proposed increases, which originated out of a September 2023 report authored by OHIC.
These rate increases do not address the state’s primary care shortage, which remains a top concern of health experts and lawmakers. However, McKee in an April 8 budget amendment proposed adding primary care services to the scope of OHIC’s biennial rate review. Legislation introduced in March by Senate Majority Leader Ryan Pearson, a Cumberland Democrat, would achieve the same result.
King, who has been credited with helping OHIC bolster its information gathering and transparency through public dashboards, welcomed the prospect of more data. But he was not on board with another legislative proposal aiming to reconcile Rhode Island provider rates with its New England neighbors.
The companion bills, sponsored by Sen. Susan Sosnowski and Rep. Teresa Tanzi, both South Kingstown Democrats, set minimums for Rhode Island provider rates based on average rates in Connecticut and Massachusetts, with oversight and review by OHIC.
“It’s similar to saying to a teacher who works for Providence Public Schools who rents an apartment in Providence’s West End should pay Boston rent for that Providence apartment,” King said.
“I am not opposed to rate increases, but that’s not a good framework,” he added.
Another area where King backed increased spending: mental health services. Per-person spending on mental health in the commercial market has “exploded” in the last five years, according to the report, increasing 70% from 2018 to 2022 for children and adolescents, and up 60% for adults in the same time frame.
“That really is driven by an increase in utilization, which I see as a good thing,” King said.
The rise of telehealth during the pandemic, coupled with temporary relaxation of interstate licensing rules allowing providers to treat patients in other states, eased access to health care across the board, including mental health services.
Based on the success demonstrated during the pandemic, state lawmakers subsequently passed a law, which took effect July 1, 2023, permanently authorizing residents to receive therapy from out-of-state psychologists as part of an interstate agreement known as the Psychology Interjurisdictional Compact.
What about the Centurion sale?
Hovering above OHIC’s newly released report: the pending sale of Roger Williams Medical Center and Our Lady of Fatima Hospital.
Atlanta-based nonprofit Centurion Foundation has offered $80 million to buy the two hospitals plus affiliated physician groups, home care and hospice agencies and offices, promising to inject another $80 million into the hospital balance sheets to bring in much-needed equipment and staff, according to its application filed with the Rhode Island Office of the Attorney General and the Rhode Island Department of Health. The two state agencies, which must approve hospital sales that involve a conversion to nonprofit ownership, have until June 11 to accept, reject or impose conditions on the sale.
King said he did not know enough about the terms of the proposed agreement to say how it might affect hospital costs and spending.
However, the threat of closing the two community-based hospitals, a possibility given its current owner’s financial woes, risks resource strains on nearby Rhode Island and Miriam Hospitals, both of which are owned by Lifespan Corporation. Lifespan’s Providence hospitals also have higher per-patient costs for both inpatient and outpatient services compared with Roger Williams and Fatima, according to data included in a Rhode Island Foundation-commissioned study published in April.
The OHIC report for the first time this year included recommendations for strengthening health care performance and oversight. They are:
Invest in primary care and community-based providers
Maintain the office’s affordability standards regulating hospital price growth
Publish more consumer-focused analysis of health care costs
Collect, analyze and publicly report data on provider finances, operating costs and physician practice group acquisitions.
GET THE MORNING HEADLINES DELIVERED TO YOUR INBOX
The post R.I. health care spending skyrocketed after COVID. Now it’s coming back down to Earth. appeared first on Rhode Island Current.

