Mass. leaders look beyond Steward crisis toward more stable health care system

- Oops!Something went wrong.Please try again later.
Correction: An earlier version of this story inaccurately reported that Good Samaritan Hospital in Brockton had closed due to a fire. Brockton Hospital, owned by Signature Health Care, is the hospital that closed.
As the black storm clouds of the Steward Health Care system financial boondoggle start to rain ramifications, state lawmakers are seeking silver linings.
“This crisis creates an opportunity, allows us to preemptively design what the health care system should look like in this region and across the commonwealth,” said Sen. Paul Feeney, D-Foxborough, the vice chair of the Senate Committee on Post-Audit and Oversight at its April 24 meeting, held at the International Brotherhood of Electrical Workers 223 building in Taunton. “It’s an opportunity for a more global view on the way to deliver health care services across Massachusetts.”
The meeting brought together legislators, state officials, policy advisers and the leaders of hospitals most affected by the possible closure of the Steward facilities.
The conversations extended beyond the crisis at hand to include other issues facing the state’s health care system. Loss of the facilities currently owned by Steward, legislators and their invited guests concluded, would destabilize the entire system of health care delivery in the state.
The financially strapped Steward administers nine hospitals in the state, which it purchased in 2010 from the former Caritas Christi Health Care, a nonprofit Catholic health provider that was established in 1985 and then sold to the private equity firm Cerberus Capital Management, later renamed Steward Health Care System. Overall, the firm operates 33 hospitals and employs 30,000 workers; roughly half, 16,000 employees, work in Massachusetts.
Which Mass. hospitals are part of the Steward network?
Steward’s properties in Massachusetts include St. Elizabeth’s Medical Center and Carney Hospital in Boston, Holy Family Hospital in Haverhill and Methuen, Nashoba Valley Medical Center in Ayer, Good Samaritan Medical Center in Brockton, Morton Hospital in Taunton and St. Anne’s Hospital in Fall River.
The Norwood Hospital was closed in 2020 and remains shuttered due to severe flooding.
“When private equity owns the real estate of a hospital, it has public consequences,” said Sen. Marc Pacheco, D-Taunton, dean of the Senate. “We need to be careful with all the other components of the system and their relationships. Providers can’t do the work without a physical structure to perform it in.”

Even as Massachusetts faces the Steward crisis, the state faces other health care issues that have been the focus of legislators and officials for years, according to officials discussing the release of a 97-page bill that would clarify how the state handles health care in the future.
That bill addresses issues ranging from financial oversight of service and insurance providers, to creating a survey that would assess existing health care providers including where they are located. The proposed survey could also determine what medical services and assets are needed and where.
The bill would also create a new commission that would oversee the industry and tease health care insurance out of the overall insurance industry.

“The bill aims to create healthier balances between the distribution of patients insured through Medicaid and MassHealth and those insured by commercial providers,” said Sen. John Cronin, D-Lunenburg, vice chair of the Joint Committee on Health Care Financing, the group that released the bill. Providers frequently lose money for servicing patients insured through government sources.
Cronin said he's "hopeful the House and Senate will reach consensus on the provisions before the session ends,”
Gateway cities in Massachusetts, as well as rural areas, have higher percentages of patients insured through governmental plans, Cronin said. Fitchburg and Leominster are the two Gateway cities in his district.
Included in the bill are provisions that address the Steward hospital crisis so that it doesn’t happen again, Cronin said. That includes allowing more financial oversight into health care providers, their owners, investors, financial assets and liabilities as well as oversight of acquisitions and sales of providers in the Massachusetts marketplace. That proposed oversight would extend to insurance providers as well.
“It would prevent future hospital executives from selling the land out from under the system,” Cronin said, referencing the sale of the land occupied by the Steward hospitals to a hospital real estate trust company. After the sale, the hospitals were to pay rent to the trust company.
Bill would allow AG more leeway
“The bill expands the civil authority the attorney general has over transactions and includes oversight of equity investors,” Cronin said.
Even before the Steward quagmire crystalized, state officials had been seeking the company’s financial records through legal action. Cronin believes the state must do more to strengthen its laws to prevent another “bad actor” from decimating the system.
The bill addresses many of those contingencies:
Barring repossession of equipment and supplies from health care providers even if the provider is in arrears.
Setting longer lead times to allow the state Department of Public Health to review proposed changes in service. Those changes in service include everything from shuttering of services to proposed expansions, corporate mergers, transactions with equity investors, transfers of assets including real estate transactions and leasebacks, and proposed transitions from nonprofit to for-profit models.
The bill also sets a rate of growth for health care costs, with state oversight of all changes that increase health care costs beyond the set standard, within a specific market and statewide.
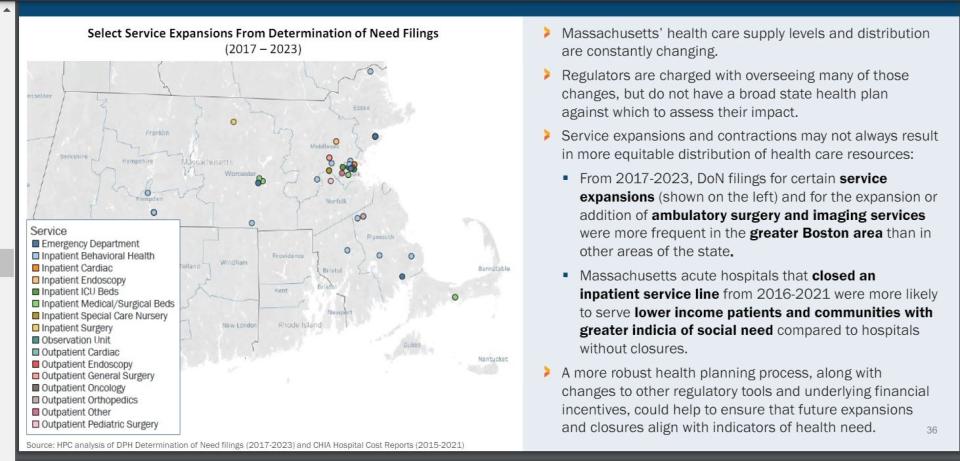
In order to develop a state health plan, Massachusetts must complete a survey of what exists and where. It must also determine what services are needed in the immediate future and in the long run.
The full impact of the Steward bankruptcy proceedings and possible sale to Optum Care, a subsidiary of United Health Group, is an unknown factor, partially because the state is unaware of the total health care picture in the state.
Unknowns could be addressed by statewide, industrywide survey
“There are a lot of unknowns that we don’t have the answers for,” said David Seltz, executive director of the Health Policy Commission, at a Thursday meeting of the Market Oversight and Transparency Committee of the Massachusetts Health Care Policy Commission.
“Do other hospital systems have the resources to absorb the patients? It’s been befuddling to us, to the administration and the Legislature,” said Seltz. “We don’t have the tools, the knowledge and that makes it harder.”
The bill would authorize a comprehensive survey of the state’s resources — everything from acute care services to free clinics as well as hospice and palliative care, and public health initiatives including screenings and early interventions. The Health Policy Commission has already started work on different aspects of the survey.
“We need to redesign the system to take the burden off of emergency care providers,” said Public Health Commissioner Dr. Robert Goldstein. He indicated that he would like to see an expanded role played by public health within the care system in Massachusetts. “What can public health do to care for people and keep them out of the system?”
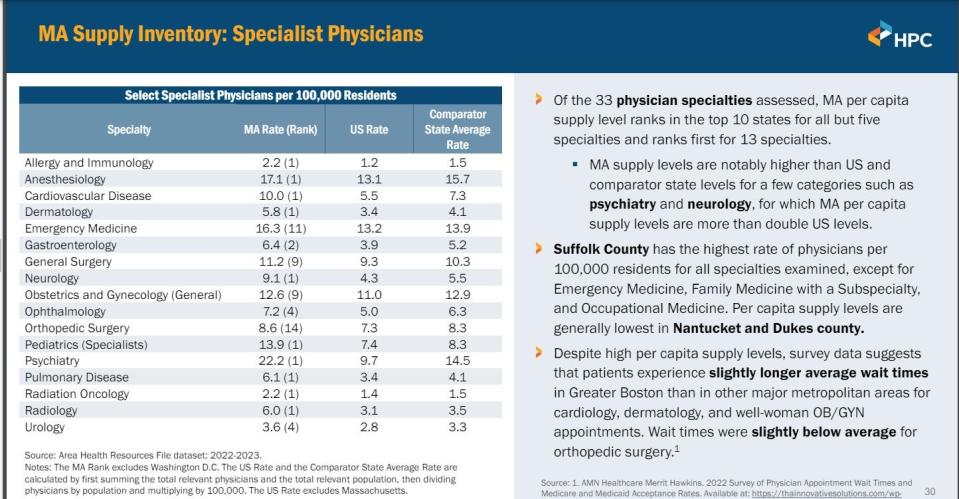
While Massachusetts has a high level of resources, more than any other state in the nation, these are not distributed evenly across the state.
The Health Policy Commission suggested the state:
Prioritize health care affordability and equity for all by setting benchmarks for service.
Control high prices charged by providers.
Oversee pharmaceutical spending.
Make health plans accountable for affordability.
Advance health equity for all.
Reduce administrative complexity.
Strengthen tools that monitor the market and align supply and service distribution with community needs.
Support and invest in the state’s health care workforce.
Strengthen primary and behavioral health care access.
Senators meeting last month learned from hospital administrators operating in the same region as the Steward hospitals that their facilities lack the capacity to absorb the 200,000-plus residents who currently receive care from those hospitals. About 20% of the state’s population lives in that region, one of the fastest-growing in the state.
The lack of capacity stems from several factors, but the most prevalent is staffing. In 2020, the region had 3,148 licensed beds but had only enough staff to accommodate patients in 82% of them; in the fiscal year that ended July 1, 2023, licensed beds dipped to 3,071 with staffing to fill 2,420, or only 78%, of them.
Legislative action seeks to ease workforce crunch
“Vacancies in health care jobs are prevalent across the state; it’s the No. 1 issue in Massachusetts,” said Feeney at the April meeting. “Why aren’t we filling these health care positions? Is it a question of housing, salaries? What can the legislature do?”
Secretary of Health and Human Services Kate Walsh said the state can help in three areas: increasing the salaries for nursing and related staff, expanding and increasing access to nursing education programs, and setting up pathways for career advancements, including help with tuition reimbursement and student loans.
“The biggest challenge is when the nurses work understaffed and under-supplied. It’s hard for them to work to the full extent of their licenses if they are chasing linens or IV tubes,” Walsh said.
Katie Murphy, president of the Massachusetts Nurses Association, said the issue is not a lack of nurses, since about 1,000 new nurses graduate every year. There are more nurses in Massachusetts in the past year than before the pandemic, she said; however, many are leaving the profession within five years of graduating.
“The conditions under which we work are the issue,” Murphy said. “We cannot provide the care that is needed to patients without enough resources.”
Another workplace condition revolves around safety. Overcrowded emergency departments can trigger stress reactions among patients and family members.
“We have been physically and verbally assaulted; people should not have to fear for their lives on a job,” Murphy said.
Despite recent state investments in behavioral health care for both adults and children, the issue of borders — patients seeking mental health care who stay in emergency departments while waiting for a bed in a behavioral health unit — is still pressing.
The Massachusetts Health and Hospital Association issued an analysis of borders throughout the system that found more than 50% of emergency department beds are occupied by behavioral health patients waiting for an appropriate bed.
It will be hard for Massachusetts to grow as a state if the health care system continues to contract, Cronin said. He said the bill offers the state an opportunity to address the inequities in the system and to allow new economic development in areas outside of Greater Boston.
He hopes simultaneous investments in health care, housing and the environment will spur economic development and attract new, younger residents.
“Our demographic: Massachusetts is an aging population and that doesn’t bode well for health care and the state’s workforce,” Cronin said. “We have to change the demographic, attract young residents to settle in the state, raise families here.”
This article originally appeared on Telegram & Gazette: Steward crisis: Opportunity to create more stable health care system?

