Homeless people stay sicker for longer and cost the health system more money, data shows

Homeless people spend twice as long in hospital and cost the system more than double than people who have a place to live, a new analysis of data shows.
Last year across Canada, nearly 30,000 people who were homeless were hospitalized and spent an average of 15 days in the hospital, compared to an eight-day average stay for people who are not homeless.
"Housing has to be considered a health issue. Homelessness is a health problem," said study co-author Cheryl Forchuk, the assistant scientific director at the Lawson Health Research Institute. "We need to see housing as a health intervention, and an integral part of a health strategy."
The average cost per stay for someone without a home was $16,800, compared with a national average of $7,800, researchers say.
The top three most common reasons for hospital stays were substance use, schizophrenic disorders, and cellulitis, a bacterial infection, the data shows. A quarter of hospitalizations are for issues related to substance use.
"Imagine trying to maintain your health on the street or even in shelters. Basic things like nutritional status, exposure to the elements, exposure to infectious diseases, the ability to sleep properly at night — a lot of the things that would for any of us act as protective factors for our health are really a challenge with homelessness," Forchuk told CBC News.

A graphic shows the difference in average length of stay and estimated cost for patients experiencing homelessness and the national average. (Lawson Health Research Institute)
Homeless people who get sick get sicker than the average person, and stay sicker for longer, she added. "It also takes longer to recover."
Since 2018, Canadian hospitals have had to document whether a patient is experiencing homelessness. Researchers have used that information to look at the demographics of those experiencing homelessness in an effort to help more people, said Brad Campbell, an executive at the London Health Science's Centre, the region's largest hospital.
"As health care providers, we recognize the importance of accurate data for understanding an individual's care journey across sectors and organizations, especially when addressing homelessness," Campbell said.
"For example, hospital and service utilization data has been essential to understanding emergency department patterns for those living without stable housing in our community, enabling us to improve care for marginalized people through different service delivery models."
Lack of primary care
The number of homeless people who went to hospital is likely higher than the 30,000 documented, because some didn't identify themselves as such, researchers said.
Almost all of the homeless patients admitted to hospital came through the emergency room, confirming what experts have long pointed out: that there is a lack of adequate access to primary care to address people's health needs before they become severe, the data shows.
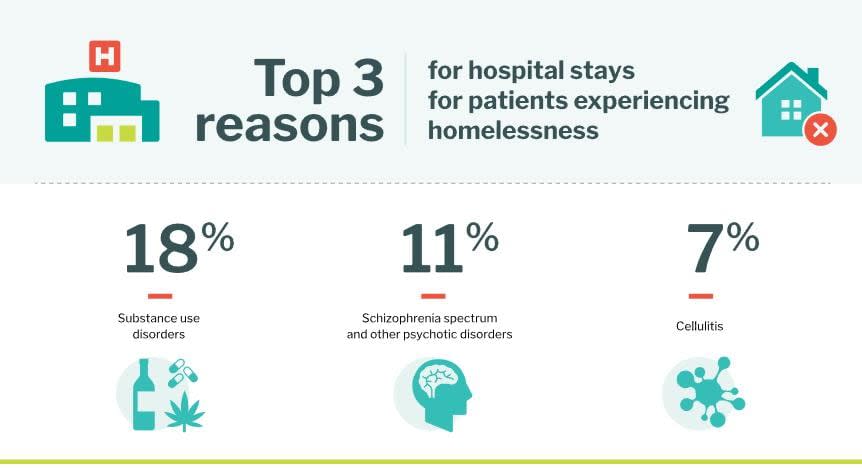
Of the Top 10 reasons for hospitalization, more than a quarter are related to substance use disorder. (Supplied by Lawson Health Research Institute)
"Most patients or people experiencing homelessness were male and more than half were younger adults," researchers said. "Indigenous peoples are disproportionately impacted by homelessness. While five per cent of the population identified as Indigenous in the 2021 Census, at least 31 per cent of people experiencing homelessness identified as Indigenous."
The numbers show that housing is connected to health and wellbeing, Forchuck said. "Housing is health care," she said. "Gathering and analyzing this data gives us more tools to find workable solutions to the complex problem of how people experiencing homelessness receive, or don't receive, the health care they need."
In London, hospitals have partnered with social agencies so people aren't discharged into homelessness, and those in hospital are given priority for housing, she added.
"I'm hoping that other communities and other hospitals will recognize housing as a strategy," Forchuk said. "If we're blind to a person's housing status, we cannot solve health problems."

