Frontotemporal dementia: What is it, symptoms and stages
Frontotemporal dementia is one of the most common types of dementia that hits before the age of 65. Although symptoms typically begin in the late 60s, it can strike as young as 30 or as old as 90.
The good news is that it’s the most fast-moving research area in the dementia space with high hopes of effective treatments on the horizon. So what is it and why could we be on the cusp of a breakthrough?
Stages of FTD: from speech stopping, frailty and loss of balance
What’s the difference between frontotemporal dementia and Alzheimer’s?
What is frontotemporal dementia (FTD)?
“It’s a group of illnesses marked by damage and shrinkage in the frontal and temporal areas of the brain,” says Dr Teresa Niccoli from the Institute of Healthy Ageing at UCL. The temporal lobes are behind the ears and the frontal lobe is right at the front, just behind the forehead.
What are the symptoms of FTD?
Personality and behaviour changes
“The frontal part of the brain gives us so much of our personality, our social knowledge and behaviour, our motivation and impulse control,” says James Rowe, a professor of cognitive neurology and the chairman of Alzheimer’s Research UK’s scientific advisory board. “It stores all the deep-seated knowledge we learn about how to behave, how to be social and what’s normal.” Symptoms of damage to the frontal lobes include:
A change in personality and sense of humour
Loss of empathy
Poor impulse control
Risky and disinhibited behaviour
Apathy and withdrawal
A very sweet tooth
Language changes
“The temporal lobes are where our language centres are based,” says Prof Rowe. “Damage here can mean we lose the ability to produce speech, and also lose the deeper understanding of what words and objects mean (called semantics).”
Symptoms include:
Fragmented, effortful speech
Inability to recall what certain words mean (‘What is a ‘lemon’?’ ‘What is a ‘tin’?’)
Inability to understand what a familiar object is or how it is used (for example, which foods are edible, how to use a kettle, what to do with a whisk)
Stages of FTD: from speech stopping, frailty and loss of balance
The progress of the disease is different for everyone and depends on many factors, including the type of FTD; if there is a genetic mutation; age of onset and areas of the brain most impacted.
“It tends to progress slowly but relentlessly,” says Prof Rowe. “While in the early years, it can be very dramatic, disruptive and challenging to live with, over time, there tends to be an increasing withdrawal.
“Language and communication slowly dry up. First the spontaneity reduces, and later speech has usually stopped altogether.
Frailty also increases. There are often problems with mobility and balance and increased nursing needs.
“The last few days of life, if managed well, tend to be calmer – for example slipping away in sleep. Keeping up the quality of life in the years before is very important.”
The average survival time after diagnosis is seven to eight years but this is highly variable, between one and 15 years.
What causes FTD?
There are three gene mutations thought to cause around a third of all cases. “Unlike many other dementias, this is heavily genetic,” says Dr Nichols.
In the other two-thirds, there are several theories. One is that it’s still genetic – but caused by our individual unique shuffling of genes, as yet not understood. Another is that it’s a small fault in the brain’s “waste disposal system”.
“The brain is constantly getting rid of junk proteins and it only needs a slight imbalance to stop it clearing the junk proteins fully every day, to set off a very slow build-up,” says Prof Rowe. Research shows that changes in the brain can start silently and gradually 25 years before symptoms begin.
How is it diagnosed?
Diagnosis should start with an in-depth conversation between the patient, the patient’s family and a specialist, such as a neurologist or psychiatrist, who knows what to ask.
“It’s almost all in the history – the story of change, the pattern that shows the person is clearly different from the person they once were,” says Prof Rowe, who leads specialist clinics for people with FTD.
A brain scan can then confirm the diagnosis, while genetic testing will identify whether someone’s illness is due to one of the genetic mutations.
While the language variants of FTD tend to be diagnosed sooner, the correct diagnosis can take several years when behaviour changes are the primary symptoms. “It’s often wrongly put down to depression, stress or relationship problems in the beginning,” says Prof Rowe.
What are the treatment options?
Medications
Antidepressants
Physiotherapy, speech and language therapy
Early stage gene neutralising technology
“Treatment needs to be tailored and individualised,” says Prof Rowe. “There are many medications that can help with the symptoms – whether it’s to do with mood, anxiety and agitation, delusions, obsessional or sexually disinhibited behaviour or disruptive sleep.”
SSRI antidepressants can be useful for a wide range of behavioural symptoms. “There’s also scope for physiotherapy, speech and language therapy, and psychological support for the family – all are important. They can be accessed by referral from a GP or memory clinic. Private providers exist in many areas for self-referral, but NHS services also exist in most areas.”
Although there are no current disease-modifying treatments to halt FTD, Prof Rowe believes that for the genetic variants at least, there soon could be. “We’re on the cusp of a revolution here,” he says.
“There are currently multiple trials using different techniques to neutralise the faulty genes which cause FTD. The background evidence looks really strong.”
These techniques include new “designer virus” to deliver replacement genes, or designer antibodies and drugs which block the faulty gene. These current technologies need to be given by drip, or injection, or an operation, but possibly a tablet in the future.
Gene neutralising technology is already licensed for the devastating childhood illness spinal muscular atrophy and seems to stop the illness in its tracks.
“We should start to see the results for FTD in the next year or two,” says Prof Rowe. “They won’t all work, but the rate of progress is so fast, that we can be optimistic. In principle, after that, it would also be possible to treat family members who have the gene but no symptoms. That would mean prevention is also on the cards.”
What’s the difference between FTD and Alzheimer’s?
The primary difference is the affected brain region which causes different symptoms. Alzheimer’s generally starts in the memory centres before spreading to most areas of the brain, while FTD is more specific. “With FTD, the first neurons you lose are related to ‘personality and behaviour’ or ‘language’,” says Dr Niccoli.
When the Hollywood actor Bruce Willis, 67, was diagnosed with FTD, the Alzheimer’s Society website saw a 12,000 per cent spike in traffic.
Support for families living with FTD
“Helping a family understand the disease and what is driving the difficult, distressing and embarrassing behaviours can ease the stress and impact of FTD,” says Professor Rowe. “Just hearing: ‘We know what this is, we will help you get to grips with it and put you in the driving seat,’ can bring relief.”
Families might need help with devising strategies to cope with certain behaviours, understand triggers, reduce stress, develop diversion techniques and perhaps find new ways to communicate , through gestures, drawings or electronic devices.
“Practical help like respite, and financial advice around benefits and early pensions can also make a big difference,” Prof Rowe explains.
“The person with FTD often feels very well and happy; our job is to keep that sense of quality of life, while also helping the family manage the challenges” Support for families can come from memory clinics, from Alzheimer society local branches, and from the FTD support group amongst others.
“At first, you’re shocked and upset. It’s ‘progressive’, ‘incurable’, your life will never be the same”
The first clear sign that something was very wrong with Urvashi Desai’s husband Bhupendra was when he turned to her and told her that their three sons weren’t his. “I didn’t know what he meant. He loved his boys, he loved me, we had a wonderful marriage. I asked: ‘Whose sons are they then?’ He said: ‘I’ve no idea, but I’ve checked their passports and they’re not mine’.”
Bhupendra was in his early 50s at the time – he is 69 now. His behaviour became increasingly odd. “He wouldn’t know what a packet of crisps is,” says Urvashi, 60. “If I asked him to pass me a lemon, he wouldn’t know where to look. He was clearly struggling and writing everything down to try and hold on to reality – bus numbers, bills.
Though he had several jobs – as a support worker, in retail, in a hotel – he left them all.
“He used to be vibrant and alive, but he was becoming withdrawn and paranoid, shut in a room with a notebook and obsessed with his Rubik’s Cube,” says Urvashi. “His world became narrower, like a funnel.
“Gradually, all the balloons that were aspects of his life – work, friends, interests – went ping, ping, ping, until there was nothing left except for family,” she says.
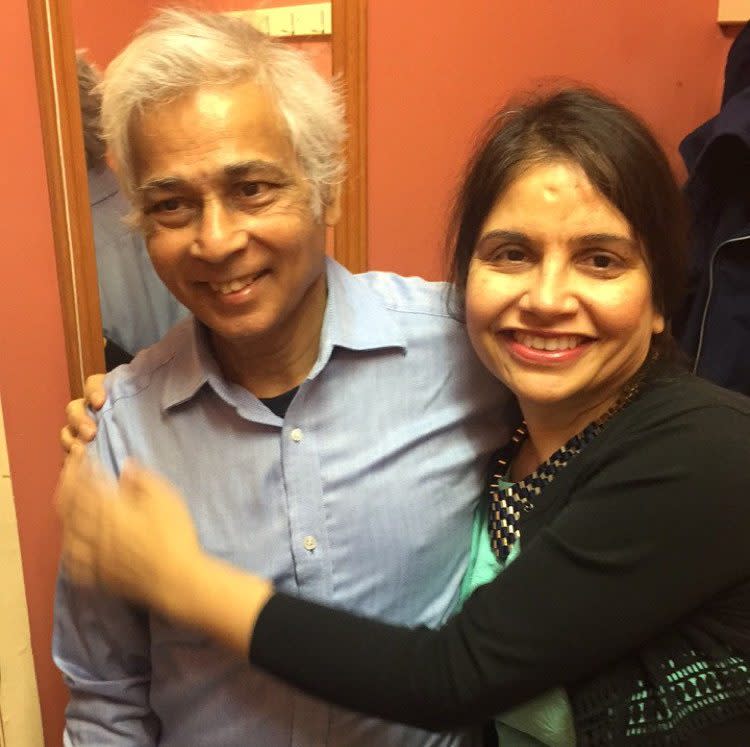
When Bhupendra was 56, Urvashi managed to get a proper, detailed consultation and assessment, which included brain scans. Frontotemporal dementia (FTD) was the devastating diagnosis.
For Urvashi, a former City HR director, building a new life has taken time. She has downsized her career to become an executive coach, and in the last two years, enlisted the help of a carer four times a week. “At first, you’re shocked and upset. It’s ‘progressive’, ‘incurable’, your life will never be the same,” she says.
“I did go on a mission, looking for a cure but I moved on from that very quickly. Counselling helped me. Now I live by one burning question: ‘How can I enrich my husband’s life?’
“He likes coffee shops and walking, so we do that a lot,” she continues. “We’ll visit museums and galleries and parks about five times a week.
“Sometimes he might behave in a challenging way and people might stare. Perhaps they’re inspired by me, or maybe they’re judging me – either way, I don’t care.”
Though Bhupendra hasn’t spoken for the last two years, Urvashi can see when he’s happy and lets this be her guide. “He’s still the pilot of my plane,” she says. “He loves music – which he never did before – so we listen to a lot of music and I sing to him. Love, energy and kindness are powerful instruments that everyone can use. It’s about transforming this into something that’s worth living – because if he is happy, I’m happy.”
If you or someone you know has dementia and would like to take part in research, register your interest in dementia research here.
Recommended
Dementia prevention: How to reduce your risk

