Do I Have a Cold or COVID?
Understanding Their Similarities and Differences
Medically reviewed by Geetika Gupta, MD
COVID-19 and the common cold share similar symptoms. How then can you tell if you have COVID-19 or the common cold? Understanding key differences in how these illnesses are caused, spread, prevented, and treated can help you seek the appropriate medical care.
The common cold, also known as upper respiratory tract infection (URI), is a viral infection of the upper airway (nose, nasal cavity, pharynx, and larynx) but can also affect the lower respiratory tract (trachea, bronchi, and lungs). Colds are the most common cause of illness in people.
By comparison, the virus that causes COVID-19 is called SARS-CoV-2, which belongs to the family of coronaviruses. COVID-19 is a highly contagious disease that begins in the upper airways and can quickly progress to infections in the lower respiratory tract, causing severe illness.
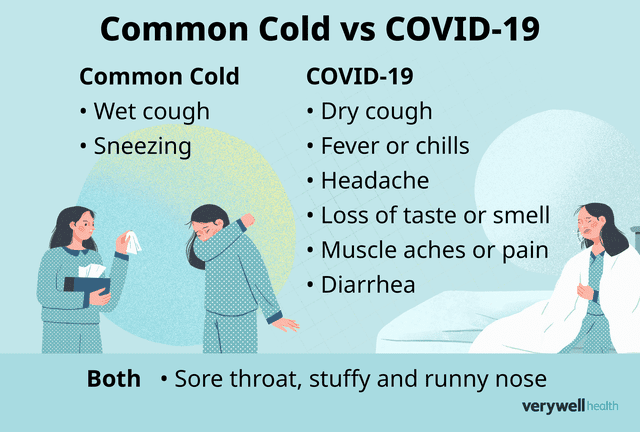
Illustration by Julie Bang for Verywell Health
By January 2023, over 100 million cases of COVID-19 had been recorded in the United States since the start of the pandemic in 2020. The common cold, however, is estimated to account for approximately 1 billion new cases annually in the United States.
This article will explain the similarities between the common cold and COVID-19 and include information on the diagnosis and treatment of each illness.
Common Cold vs. COVID-19
The common cold and COVID-19 share symptoms. However, the symptoms of COVID-19 are generally more serious and can progress to severe disease, even death. The severity of COVID-19 symptoms also increases if you have underlying health conditions, are unvaccinated, or are 65 or older.
That said, it's important to note that while some people infected with COVID-19 are asymptomatic (showing no symptoms), they can still be contagious. Common symptoms of the common cold and COVID-19 include:
Symptoms | Common Cold | COVID-19 |
Fever or chills | Rare | Common |
Uncommon | Common | |
Tightness or pressure on chest (respiratory distress) | Sometimes | Common |
Coughing | Common (usually wet) | Common (usually dry) |
Stuffy and runny nose | Common | Common |
Common | Rare | |
Sore throat | Common | Common |
Loss of taste or smell | Uncommon, although production of mucus can block nasal passages and lead to temporary loss of taste or smell | Common |
Diarrhea | Rare | Sometimes |
Muscle aches and pain | Uncommon | Common |
Related: Regaining Smell After COVID-19: What Can You Do?
Similarities
The common cold and COVID-19 are caused by respiratory viruses (although different ones). The common cold is most often caused by rhinoviruses, while SARS-CoV-2 causes COVID-19. Some coronaviruses other than SARS-CoV2 can cause the common cold.
These viruses spread in similar ways, such as through respiratory droplets when someone talks, coughs, or sneezes. People can also contract these illnesses by touching surfaces contaminated with either SARS-CoV-2 or rhinoviruses and then touching their eyes, nose, or mouth.
Differences
A key difference between the common cold and COVID-19 is the incubation period (time of exposure to an infection and the appearance of the first symptoms).
For the common cold, the incubation period is relatively short, usually one to three days. For COVID-19, the incubation period can range anywhere from two to 14 days.
If you develop symptoms of COVID-19, the Centers for Disease Control and Prevention (CDC) recommends you should do the following:
Stay home and away from others until your symptoms improve for 24 hours (without the use of fever-reducing drugs)
After your symptoms improve for 24 hours, you can resume normal activities, but you should continue to take added precautions for the next five days. This includes avoiding close contact with others and wearing a well-fitting mask.
What Does "Close Contact" Mean?
According to the CDC, "close contact" refers to someone who was less than 6 feet away from an infected person for 15 minutes. This can include 15 minutes at a given time or over a 24-hour period. Studies have shown that wearing medical graded masks (N95 or KN95) is at least 95% effective at protecting people from contracting COVID-19.
Related: Does Health Insurance Cover At-Home COVID Tests?
Diagnosis
Colds are usually diagnosed by their symptoms alone as there is no lab test for cold viruses. But since there is an overlap in symptoms with colds and COVID-19, taking a COVID-19 test can help determine what is causing your illness. As well, your healthcare provider may test you for influenza.
COVID-19 tests can detect SARS-CoV-2, or antibodies that your body makes after getting COVID-19 or getting vaccinated.
Tests for SARS-CoV-2 tell you if you have an infection at the time of the test. This type of test is called a viral test because it looks for viral infection. Examples of viral tests include antigen (pieces of viral protein) and nucleic acid amplification tests (NAATs). Both are approved by the Food and Drug Administration (FDA) and may be covered by your insurance.
When you get a COVID-19 test, you can select a rapid antigen test or laboratory PCR (polymerase chain reaction) test. A healthcare professional will take a sample of cells from your nose, mouth, or throat.
Rapid antigen tests are usually performed in minutes, while laboratory tests can take up to several days to complete depending on testing demands. Same-day laboratory tests are also available in certain locations but may require a fee.
At-home rapid antigen tests are also widely available. If you have a positive home antigen test, contact a healthcare provider for advice on treatment.
In mid-2020, the FDA approved at-home PCR test kits. People can collect samples of cells (usually a nasal swab) at home and then send the sample to a lab for testing.
Rapid vs. Laboratory Tests
While rapid antigen tests yield fast results (in minutes), they're usually less accurate and less sensitive in detecting viral antigens, especially in individuals who are asymptomatic. In comparison, laboratory PCR tests yield slower results (in days) but are significantly more accurate and sensitive, as they detect the presence of the ribonucleic acid (RNA) of SARS-CoV-2.
Related: When and What Day to Test for COVID-19
Treatment
The best way to protect yourself from COVID-19 is to get vaccinated before you are infected. If you're symptomatic for COVID-19 and don't require medical attention, stay isolated and take the following steps to manage your symptoms. These steps are also effective in relieving common cold symptoms.
They include:
Take over-the-counter (OTC) medications, such as acetaminophen (Tylenol) or ibuprofen (Advil or Motrin) to reduce fever and body aches.
Drink plenty of fluids (water, herbal tea, clear soup) to stay hydrated.
Get plenty of rest to fight off the infection and speed up the recovery process.
If your COVID-19 symptoms become worse (shortness of breath or chest pain), seek medical attention immediately. All treatments for mild to moderate cases of COVID-19 should be prescribed by a healthcare provider. They may prescribe FDA-approved treatments such as:
Veklury (remdesivir): This drug has been shown to prevent SARS-CoV-2 from reproducing in the cells. It is available for people who have mild to moderate cases and are at high risk of developing a severe case, and for people who need hospitalization. Studies have also shown that it shortens the recovery time of people infected with COVID-19 by about five days.
Paxlovid (ritonavir-boosted nirmatrelvir): This antiviral drug is given as a pill. It may be used to treat people who have a mild to moderate case and are at higher risk of developing severe COVID-19.
Several anti-SARS-CoV-2 monoclonal antibodies (mAbs) received Emergency Use Authorization (EUA) from the FDA, but only one (Actemra) is still authorized for use in the United States. The drugs were found to be less effective against the predominant Omicron COVID variants, which led to the FDA revoking their EUAs.
COVID-19 Safety Reminder
If you have COVID-19, don't attempt to take any medications or substances that aren't FDA approved or authorized. Taking products that are not approved could harm your body or cause death. Remember, a healthcare provider will decide the best course of treatment for you.
When It's an Emergency
COVID-19 can progress to severe disease, especially among individuals who aren't vaccinated. Seek emergency medical care immediately if you or someone you know show these signs and symptoms:
Difficulty breathing
Pain, tightness, or pressure in the chest
Confusion and disorientation
Pale or bluish skin (due to lack of oxygen in the blood)
Related: What Should You Do if You Test Positive After a Booster Shot?
Summary
The common cold and COVID-19 are both caused by respiratory viruses. Colds affect the upper airway (nose, nasal cavity, pharynx, and larynx) and can affect the lower respiratory tract (trachea, bronchi, and lungs). COVID-19 also affects the upper and lower respiratory systems but can cause severe disease in the lungs, and sometimes death.
COVID-19 tests tell you if you have an infection in real time by looking for viral infection. If you test positive for COVID-19, treatments are available mild-to-moderate cases, as well as for severe disease requiring hospitalization. However, getting vaccinated is the best protection.
For the common cold, which typically produces mild symptoms, treatment includes staying hydrated, getting enough sleep, and taking OTC medications as needed.
The information in this article is current as of the date listed, which means newer information may be available when you read this. For the most recent updates on COVID-19, visit our coronavirus news page.
Frequently Asked Questions
How can I be sure I don't have COVID-19?
The best way to prevent illness is to avoid being exposed to the virus. The CDC recommends taking measures to help prevent the spread of respiratory diseases.
These include being fully vaccinated and boosted, wearing a medical-grade mask (N95 or KN95), washing your hands for at least 20 seconds, social distancing (at least 6 feet or more), and avoiding large crowds.
How long does a cold last?
Common cold symptoms, which generally affect the upper respiratory system, typically peak at one to three days and last seven to 10 days. However, they can linger for as long as three weeks in some cases.
Cold symptoms are generally mild, but if your symptoms remain the same or become worse over time, consider seeking medical attention from a healthcare professional.
How long does COVID-19 last?
How long COVID-19 stays in the body varies from person to person. Generally, people are no longer contagious about 10 days after the onset of symptoms. However, a 2020 study from the Lancet Microbe found that people can shed the virus for as long as 83 days, underscoring the importance of frequent testing, quarantining, and isolation practices.
How many people have died from COVID-19?
As of January 2023, over 1,100,000 COVID-19 deaths have been reported in the United States. By comparison, over 6.8 million individuals had died from COVID-19 worldwide by January 2023.
Where can I find a COVID-19 vaccine?
According to the CDC, everyone 6 months of age and older are now eligible to get a COVID-19 vaccination. You can get a vaccine at many locations such as a clinic, pharmacy, pop-up vaccine site, and even a dentist's office. For a list of participating vaccine sites in your town or city, visit vaccines.gov.
Read the original article on Verywell Health.

