How the world’s first malaria vaccine program benefits children
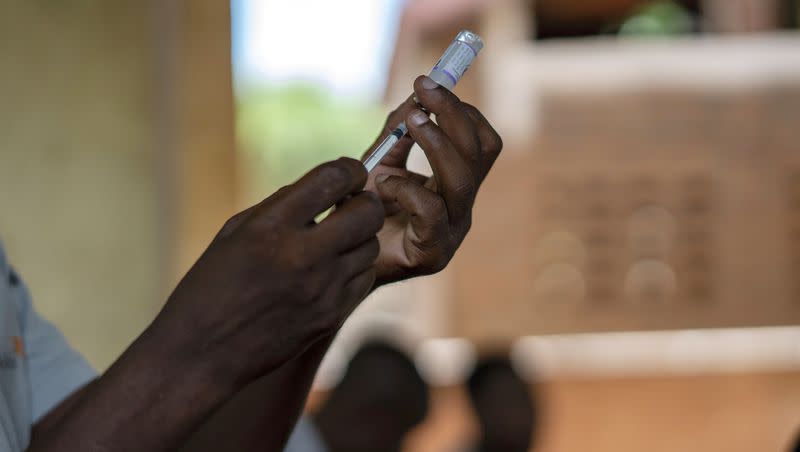
On Monday, Cameroon, a country in Central Africa, launched its plan to routinely give children a new malaria vaccine.
The campaign is a milestone in the decadeslong effort to stop the disease happening in Africa, where 95% of the world’s malaria deaths occur, according to NBC News.
What is malaria and why does it have a large death rate?
Malaria is a life-threatening disease spread by certain mosquitoes, typically found in tropical countries. Symptoms include fever, chills, headaches, fatigue, confusion, seizures and difficulty breathing, depending on the severity of the case. The disease is preventable and curable, per the World Health Organization.
Due to scarce resources and socioeconomic instability in areas where malaria is concentrated, individuals and governments find it hard to prevent and treat the disease, creating larger death rates, according to the Centers for Disease Control and Prevention.
Children under the age of 5, because of their lack of immunity to the virus, account for 78% of all malaria deaths in the African Region, per WHO.
Related
How does the vaccine benefit children?
The malaria vaccine reduces 13% of all kinds of deaths among children, not just from contracting malaria, according to NPR.
This is “not only a huge step forward for malaria control but also a major advancement in child health,” said Mary Hamel, the WHO’s senior technical officer on malaria, to NPR.
How does the vaccine work?
Cameroon has begun using Mosquirix, the first of two recently approved malaria vaccines. The vaccine, sold by GlaxoSmithKline, is about 39% effective and requires four doses, according to NPR.
“While 39% efficacy seems low for a vaccine, when we consider the sheer burden of malaria, this means potentially a huge reduction in cases and deaths among children,” said Aaron Samuels, CDC’s Kenya malaria program director, to the CDC.
What are the challenges?
The fact that four doses are needed causes some difficulty in coordinating, and each dose costs about $9.80, per NPR.
Another challenge is that GlaxoSmithKline can only produce about 15 million doses of Mosquirix a year.
A second malaria vaccine developed by Oxford University and approved by WHO last October offers hope for a more practical solution. The vaccine would be cheaper, require only three doses and India’s Serum Institute said it can make up to 200 million doses a year, according to NBC News.
While there is still ways to go, Mohammed Abdulaziz, head of disease control and prevention at Africa CDC, is encouraged.
“For a long time, we have been waiting for a day like this. It brings more than just hope. It brings a reduction in the mortality and morbidity associated with malaria,” he said in a press conference with NPR.
Cameroon hopes to vaccinate about 250,000 children this year and next year. There are plans in place to also introduce the vaccine in 20 additional countries and immunize more than 6 million children by 2025, per NBC News.

