What Is Wet Age-Related Macular Degeneration (Wet AMD)?
Medically reviewed by Johnstone M. Kim, MD
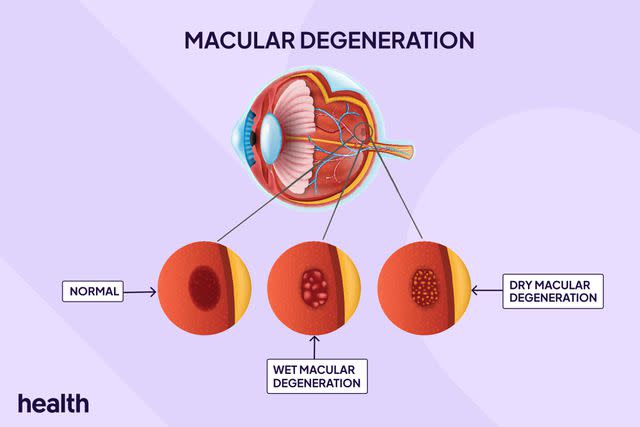
Wet age-related macular degeneration (AMD), or advanced neovascular AMD, is an eye condition affecting central vision. It is an advanced form of age-related macular degeneration (AMD), which is also commonly referred to as simply macular degeneration or MD.
Wet AMD occurs when abnormal blood vessels develop beneath the macula—the part of the retina that helps you see objects straight ahead. These abnormal vessels leak fluid or blood, damaging the macula and leading to blurred or distorted vision.
Without treatment, wet AMD can progress rapidly and lead to blindness. Medications and laser therapy can effectively slow disease progression and preserve vision. Nearly 20 million adults in the U.S. live with age-related macular generation (AMD), with wet AMD accounting for between 10 to 15% of all cases.
Design by Health
Types of Age-Related Macular Degeneration
Age-related macular degeneration is a leading cause of permanent vision loss in older adults worldwide. About 1 in 8 people over age 60 have AMD, and the risk increases with age. There are two main types of age-related macular degeneration (AMD): dry and wet.
Dry AMD
Dry AMD is the most common type of age-related macular degeneration, accounting for 85 to 90% of all cases. The macula thins over time with dry AMD, and clumps of drusen (yellow-colored deposits of lipids and protein) grow under the retina. People with dry AMD may have hazy vision, blurry central vision spots, or trouble seeing in low lighting.
Wet AMD
Wet AMD is a more advanced form of AMD that develops when abnormal blood vessels in the macula leak fluid or blood, which damages and scars the macula. Between 10 and 15% of people with dry AMD will develop wet AMD, which progresses rapidly and can lead to severe vision loss or blindness.
Wet AMD Symptoms
Wet AMD affects your central vision—the straight-ahead part of your vision that allows you to see details and colors clearly. You need central vision to drive, read, and recognize faces. Symptoms of wet AMD can develop suddenly, often causing noticeable vision changes that worsen within days or weeks.
Wet AMD symptoms can affect one or both eyes and may include:
Blurry or blind spots: A blurry or dark ‘spot’ in your central vision that may appear red, black, or gray and can grow in size over time.
Distorted vision: Straight lines may appear wavy or crooked, and objects may appear to change shape, size, or color or disappear when looking at them.
Reduced color vision: Colors may seem faded or less vibrant.
Difficulty adjusting to low light: It may take longer for your eyes to adjust to dim lighting, and many people with wet AMD have trouble seeing in low-light conditions.
Increased sensitivity to light: Some people with wet AMD experience discomfort when exposed to bright light.
Causes
Wet AMD develops when abnormal blood vessels grow under the macula, the small area in the middle of the retina. These blood vessels leak blood and other fluids, which can build up and damage the macula, leading to blind spots and blurry, distorted vision.
Wet AMD occurs in people with dry AMD, and experts suggest these abnormal, leaky vessels grow in response to the damage and functional problems that dry AMD causes.
Risk Factors
A combination of genetic and environmental factors likely play a role in developing age-related macular degeneration, but the exact cause is unknown. Wet AMD occurs in about 10 to 15% of people with dry AMD. Certain factors can increase your risk of developing the condition.
Risk factors for wet AMD include:
Age: Wet AMD is most common in adults ages 60 and older, and the risk increases with age.
Sex: People assigned female at birth are more likely to develop wet AMD.
Family history: Genetic factors play a role in the development of AMD, and having a family history of the condition increases your risk.
Ethnicity: Wet AMD is most common in people with Caucasian ancestry, especially those with light iris/eye color (e.g., blue).
Diet: Consuming a diet high in processed and fried foods, red meat, and high-fat dairy can increase your risk of wet AMD.
Smoking: Smoking damages the blood vessels, which may promote the growth of abnormal blood vessels in the eye.
Alcohol: Drinking alcohol causes inflammation, which can damage body tissues, including the retina.
Underlying conditions: Obesity and high blood pressure (hypertension) can increase your risk of wet AMD.
Diagnosis
Healthcare providers specializing in eye and vision care, such as ophthalmologists and optometrists, can diagnose wet AMD. During your appointment, your eye doctor will ask about your symptoms, including when and how quickly they progressed. They will also ask about your family history, whether you have any medical conditions or are taking medications, and your risk factors (e.g., whether you smoke).
Your eye doctor will perform a comprehensive eye examination, including a visual acuity (eye chart) test and an Amsler grid exam. The Amsler grid, which resembles graph paper, has straight lines and one black dot in the grid’s center. Your provider will ask you to look directly at the dot. If the grid lines appear wavy or missing, it is a sign of AMD.
The eye examination also involves dilating your pupils using eye drops so they can closely examine your retina to look for signs of wet AMD and determine whether there is optic nerve damage.
If your eye doctor suspects you have wet AMD, they may perform additional diagnostic tests, including:
Fluorescein angiography: This test involves injecting a fluorescent dye into your arm that travels to the blood vessels in your eye. Your eye doctor then takes pictures of your eye at timed intervals for 15 minutes to see if there are any leaks from abnormal blood vessels in the retina.
Indocyanine green angiography (ICG): Similar to fluoresceine angiography, this test involves using a green dye to help visualize blood flow in your choroid, a thin layer of blood vessels in between your retina and sclera (white of the eye)
Optical coherence tomography (OCT): This is an imaging test that uses light waves to create detailed cross-sectional images of your retina, allowing your eye doctor to see the layers of your retina and detect any abnormalities.
Treatments for Wet AMD
Treatment for wet AMD aims to control the growth of abnormal blood vessels under the macula and prevent further damage to the retina to maintain your vision and prevent further vision loss.
Anti-VEGF Injections
Anti-vascular endothelial growth factor (VEGF) injections are the first-line treatment for wet AMD. These injections contain medications that block the activity of vascular endothelial growth factor (VEGF), a protein in the body that promotes the growth of new blood vessels.
Before administering the injection, your eye doctor will first numb your eye to reduce your discomfort and clean your eye to prevent infections. Anti-VEGF injections are administered directly into your eye using a thin needle. Most people need regular anti-VEGF injections, typically once a month at the start of treatment, though you may need fewer injections over time.
Ninety percent of people who receive anti-VEGF treatment retain their vision, and about one-third see improvements to their vision. Your healthcare provider may inject one of the following anti-VEGF medications:
Avastin (bevacizumab)
Eylea (aflibercept)
Lucentis (ranibizumab)
Beovu (brolucizumab)
Vabysmo (faricimab)
Photodynamic Therapy (PDT)
Photodynamic therapy (PDT) is a less common treatment for wet AMD that some healthcare providers use in combination with anti-VEGF injections. PDT involves injecting a light-sensitive medication (verteporfin) into your arm that travels through your body’s blood vessels, including in your eyes.
Verteporfin activates when exposed to a specific laser light, which your healthcare provider shines on a small area on the back of your eye. This closes off the leaking blood vessels to prevent further damage to the retina.
Nutritional Supplements
Certain nutritional supplements may slow the progression of wet AMD and help protect your vision. Studies exploring the benefits of vitamins and minerals for preventing AMD have shown promising results regarding the daily use of nutritional supplements, including:
Related: Should You Take Copper and Zinc Supplements Together? Here's What To Know
Prevention
There is no guaranteed way to prevent wet AMD; some risk factors, such as age and family history, are not within your control. However, certain lifestyle habits may help lower your risk of developing wet AMD, including:
Avoid smoking: Smoking is a major risk factor for developing AMD; not smoking is one of the best ways to protect your eye health and vision.
Eat for eye health: An eye-healthy diet rich in fruits, vegetables, and omega-3 fatty acids can benefit your eye health. Colorful fruits and vegetables, such as kale, berries, broccoli, papaya, Swiss chard, and spinach, are especially beneficial for eye health.
Get regular eye exams: Regular comprehensive eye exams with your eye doctor can help detect changes to your eye health and vision early and ensure you get prompt treatment to detect eye conditions early and protect your vision.
Related Conditions
Several conditions share risk factors with wet AMD, and some may contribute to its development. Common wet AMD-related conditions include:
Dry AMD: The most common form of age-related macular degeneration, dry AMD progresses to wet AMD in about 10 to 15% of people with the condition.
Cataracts: Cataracts are cloudy areas in the eye's lens, causing blurry vision. Cataracts and wet AMD are both age-related eye conditions common in older adults.
Glaucoma: Glaucoma is a group of eye diseases that damage the optic nerve and cause progressive vision loss. Glaucoma and wet AMD share some risk factors (e.g., age, family history), and some people can develop both.
Living With Wet AMD
Getting a wet AMD diagnosis can be overwhelming and worrisome, but with early diagnosis and treatment, most people with wet AMD can prevent further vision loss and maintain their quality of life. Some people may experience progressive vision decline despite treatment, which can impact daily activities. Fortunately, resources are available to help you manage the condition.
Low-vision aids and assistive technology, such as magnifiers and voice-activated devices, can help with daily tasks like reading, writing, and using electronic devices. Joining support groups and connecting with others with wet AMD and other vision conditions can provide emotional support, understanding, and guidance on coping with vision loss. Your eye doctor may refer you to a low-vision therapist who can help you adapt to your daily routines and maintain independence with vision loss.
Frequently Asked Questions
Is it better to have wet or dry AMD?
Neither dry nor wet AMD is “better” to have, as both can lead to vision loss. While dry AMD typically progresses more slowly than wet AMD, there are no treatments for dry AMD until it progresses to late-stage or wet AMD.
What is the average age of getting a diagnosis of wet AMD?
The average age of diagnosis for age-related macular degeneration is approximately 75 years old. The risk of wet AMD increases with age and is most common in people 60 and older.
How quickly does macular degeneration cause blindness?
Dry age-related macular degeneration can cause gradual vision loss over several years and may never progress to total blindness. Wet AMD can cause sudden, rapid vision loss over days or weeks, requiring prompt treatment to prevent blindness.
For more Health.com news, make sure to sign up for our newsletter!
Read the original article on Health.com.

