Vasectomy to Prevent Pregnancy
Facts to Help You Decide
Medically reviewed by Jamin Brahmbhatt, MD
A vasectomy is a surgical form of birth control that cuts off the supply of sperm to your semen. It is done by severing and sealing two long tubes that transport sperm from the testicles, called the vas deferens. Most vasectomies are performed as an in-office procedure under local anesthesia.
Vasectomies are generally safe and effective with a relatively short recovery time (usually around a week). Although vasectomies are considered a permanent form of contraception, they can be reversed in many cases should a person change their mind.
This article explains what is involved in a vasectomy, including the different procedures and how they are performed. It also describes what to expect during and after recovery as well as your options for vasectomy reversal.
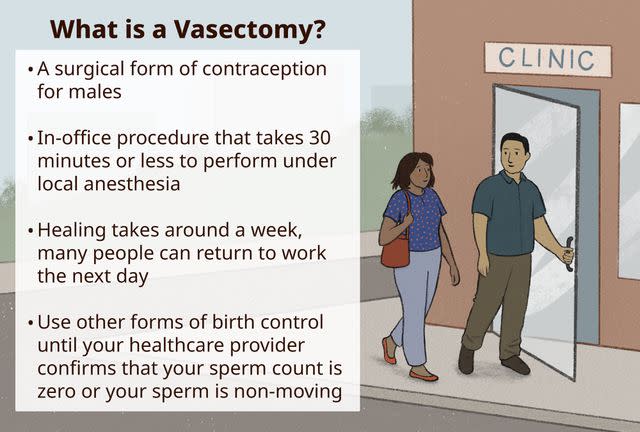
Illustration by Paige McLaughlin for Verywell Health
A Note on Gender and Sex Terminology
Verywell Health acknowledges that sex and gender are related concepts, but they are not the same.
Sex refers to biology: chromosomal makeup, hormones, and anatomy. People are most often assigned male or female at birth based on their external anatomy; some people do not fit into that sex binary and are intersex.
Gender describes a person's internal sense of self as a woman, man, nonbinary person, or another gender, and the associated social and cultural ideas about roles, behaviors, expressions, and characteristics.
Research studies sometimes don't use the terminology in this way. For example, terms that describe gender (“woman,” “man”) may be used when terms for sex (“female,” “male”) are more appropriate.
To reflect our sources accurately, this article uses terms like "female," "male," "woman," and "man" as the sources use them.
Deciding to Have a Vasectomy
The most obvious reason for a vasectomy is to prevent an unplanned pregnancy. While effective, the decision to have a vasectomy is a highly personal one that shouldn't be rushed.
As the only permanent form of male birth control, a vasectomy may be the ideal solution if you are sure you don't want to produce more children.
While many vasectomies can be reversed, there's no guarantee that yours will be. So, this is one of the main factors you'll need to consider before pursuing a vasectomy.
Here are a few facts that may help you make an informed choice:
Effectiveness: People who undergo a vasectomy have between a 0.2% and 1.5% chance of conceiving a pregnancy with a partner. By contrast, the real-world failure rate of external (male) condoms is around 87%, even with consistent use.
Revision rates: Vasectomies are effective but not perfect. Even so, less than 1% of people who undergo the procedure require repeat surgery, according to the American Urological Association (AUA).
Alternatives: Tubal ligation, a permanent form of contraception for females, is equally effective in avoiding unplanned pregnancy. However, it is a more complicated surgery and one that is less likely to be reversed. There is also a significant risk of ectopic pregnancy (a nonviable pregnancy implanted outside the uterus).
How Much Does a Vasectomy Cost?
The cost of a vasectomy can vary based on where you live and the type of procedure used. On average, expect to pay around $1,000 if you are paying out of pocket, including tests and follow-up visits.
Vasectomies may be covered in part or in full by your health insurance plan, including Medicaid and Medicare Advantage. (Vasectomies are not a benefit of Medicare Part A or B.) Contact your insurance provider for details.
Possible Risks of a Vasectomy
A vasectomy is a commonly performed procedure that is considered safe and effective. With that said, there are risks associated with vasectomies that you need to be aware of.
According to the AUA, the rate of complications hovers between 1% and 2%, the most common of which include:
Post-operative infection (usually mild and limited to the incision site)
Hematoma (the pooling of blood under the skin)
Chronic scrotal pain (pain in the scrotum lasting three months or more)
Less commonly, an abnormal cyst (spermatocele) can develop in a coiled tube called the epididymis, where sperm from the testicle is collected and stored. A fluid-filled sac (hydrocele) can also develop around a testicle, causing the scrotum to swell. Both of these can occur many days after the surgery and tend to resolve gradually on their own.
Advances in surgical techniques have greatly minimized many of these risks reducing the size of incisions and occasionally leaving the vas deferens unblocked (which may reduce the risk of long-term pain).
Related: Vasectomy Side Effects You Should Know
Types of Vasectomy
A vasectomy is performed by a specialist known as a urologist, typically in an office or clinic. There are two main types:
Conventional incisional vasectomy: A scalpel vasectomy involves making one or two incisions around 1 inch long on the scrotum ("ball sac") using a scalpel. The incision may require stitches.
No‐scalpel vasectomy: Also known as a "keyhole vasectomy," this involves puncturing the skin of the scrotum with a forceps‐like tool, creating one or two 1/4-inch holes. Stitches are usually not needed.
Because the no-scalpel method creates a smaller wound, the risk of infection, pain, and hematoma is lower than with a conventional vasectomy. Both methods are equally effective in preventing pregnancy.
Step-by-Step Process of Vasectomy
Irrespective of whether a scalpel or no-scalpel procedure is used, the general aims of the procedure are the same, with a few variations.
Prior to undergoing a vasectomy, you may be asked to stop taking blood thinners like heparin, Coumadin (warfarin), and Plavix (clopidogrel) as well as nonsteroidal anti-inflammatory drugs (NSAIDs) like aspirin, Advil (ibuprofen), and Aleve (naproxen) several days beforehand to prevent excessive bleeding.
Related: Vasectomy: How to Prepare
Here is what you can expect when undergoing a vasectomy:
You will be asked to undress and lie on a procedure table.
You'll be given an injection of local anesthetic in your scrotum or lower groin to prevent pain. Some urologists use a special jet injector that delivers anesthesia through the skin without a needle.
Once you are numb, the urologist will either make one incision (cut) in the middle of the scrotum or two incisions on either side of the scrotum. With the no-scalpel method, the skin is punctured rather than cut.
The vas deferens are gently lifted through the openings in the skin and cut.
The cut ends are then either tied, clamped, or with electricity. (Some urologists perform an open-end vasectomy in which the cut ends are left unsealed, allowing sperm to drain into the testicles, where they are broken down and reabsorbed by the body.)
The vas deferens are then returned to the scrotum.
If needed, the opening in the skin is closed with stitches or surgical glue. With the no-scalpel method, the puncture wound may be left to close on its own.
Vasectomies usually take 10 to 30 minutes to complete. After a short rest, you can put on your clothes and return home.
Related: Vasectomy: What to Expect on the Day of Surgery
Where Do Sperm Go After a Vasectomy?
Under normal circumstances, sperm cells are "warehoused" in the epididymis until they are ejected from the penis during ejaculation. The epididymis is "upstream" from the vas deferens. If ejaculation doesn't occur, the sperm cells will die in the epididymis within two to four weeks and be naturally absorbed in tissues. After a vasectomy, the same will occur.
If the vas deferens are not adequately closed during the procedure (or an open-ended vasectomy is used), the sperm cells will drain directly into the scrotum, where they are broken down and absorbed. There may be a slightly increased risk of pregnancy, but the overall failure rate remains extremely low (between 0.04% and 0.08% after six months).
After Vasectomy: Self-Care and Healing
Some level is pain or swelling can be expected after a vasectomy, although these are generally mild and tend to resolve within a few days.
To help promote healing and make your recovery more comfortable:
Rest for 24 hours, and stay off your feet for as much as possible the next couple of days.
Wait at least 24 hours before showering to give your wounds time to heal. Avoid soaking in a bathtub for three to four days. Pat the skin dry but thoroughly after cleaning.
For the first few days, wear an athletic support/jock strap or snug cotton briefs to support the testicles.
Avoid heavy lifting, exercise, or strenuous activity for seven to 10 days.
You can ease swelling and pain by applying an ice pack to the scrotum for 10 to 20 minutes several times a day. Place a cloth between the ice pack and your skin to prevent frostbite.
If needed, take Tylenol (acetaminophen) to help relieve pain. Avoid NSAIDs like aspirin which can promote bleeding.
If strips of tape have been placed on the incision, leave them on for a week or until they fall off.
Many people can return to work the day after a vasectomy. But if your job involves physical labor or lifting, you may need to wait two to three days.
Should You Expect Pain From a Vasectomy?
You can expect to have some pain or discomfort following a vasectomy, with most cases being relatively mild and resolving within seven days.
With that said, some studies suggest that pain may persist for up to four weeks in 30% of people. Some experts recommend wearing an athletic supporter for up to two weeks and applying an ice pack intermittently for the first 24 to 48 hours to reduce pain.
Related: Recovering From Your Vasectomy
Vasectomy Recovery Time
The recovery time for a vasectomy is generally between seven and 10 days. Even so, there may be lingering pain or discomfort for days and sometimes weeks after. It is rare for the pain to persist for more than three weeks.
Sexual intercourse can usually be resumed within a week, pending your urologist's approval. It's important to remember pregnancy is still possible as long as your sperm count is above zero. Until that time, another method of contraceptive is needed, such as condoms or the birth control pill.
Your sperm count—also known as a post-vasectomy semen analysis, or PVSA—will be checked eight to 16 weeks after the surgery. According to updated guidance from the AUA, a vasectomy is successful if the PVSA confirms that you either have no sperm (azoospermia) or low levels of non-moving (non-motile) sperm. In the past, two successive counts were needed.
Sex After Vasectomy
A vasectomy neither affects your libido (sex drive) nor your ability to get an erection, have an orgasm, or ejaculate ("cum"). The only thing it changes is your ability to conceive a pregnancy.
A vasectomy does not protect against sexually transmitted infections (STIs). If you have more than one sexual partner, practice safer sex by using condoms consistently.
Related: Confirming Sterility After a Vasectomy
Vasectomy Not Healing Right
It is not uncommon after a vasectomy to have significant bruising and clear fluid drainage from the surgical wound. These are normal. But there are times when a vasectomy may not be healing as it should.
Generally speaking, the wound should be well on its way to healing after a week or so. This means that your symptoms are starting to ease. Although the pain may persist, it shouldn't be getting significantly worse.
Arguably, the biggest concern following a vasectomy is the risk of infection. While uncommon, it can occur if wound care instructions are not followed, or the wound is placed under stress due to excessive physical activity.
It is important to call your healthcare provider immediately if you develop the following signs of infection after undergoing a vasectomy:
Fever over 100.4 F
Chills
Increasing pain, redness, heat, and swelling
A yellowish, greenish, or pus-like discharge, often foul-smelling
Antibiotics will be prescribed to help clear the infection.
Related: 7 Ways to Prevent Surgical Infections
What Happens During Vasectomy Reversal
A vasovasostomy is a surgery used to reverse a vasectomy. It is an increasingly common and successful procedure that can be used even in people who had undergone a vasectomy decades earlier.
Studies suggest that between 2% and 6% of people in the United States change their minds after having a vasectomy. There are many reasons for this, including a new relationship, a change in financial situation, or wanting to alleviate chronic scrotal pain (known as post-vasectomy pain syndrome).
A vasovasostomy is a highly technical form of microsurgery that aims to reattach the ends of one or both vas deferens. A more complicated procedure called a vasoepididymostomy may be used if there the vas deferens are blocked.
How Successful Is Vasectomy Reversal?
Age doesn't disqualify you from a vasovasostomy, but it can affect success rates. If you had a vasectomy within the past three years, for instance, you have a 76% chance of conceiving after the procedure. After 15 years, the success rate drops to around 30%.
A vasovasostomy is typically an outpatient procedure performed in a hospital under general anesthesia. It is generally performed as followed:
After general anesthesia is administered, you are placed on your back on the surgical table.
An incision about 1/2 inch long is made on the upper side of the scrotum.
The cut ends of the vas deferens are lifted to the surface, and the ends are trimmed.
Fluid is taken from the end closest to the testicle and examined to see if there are any viable sperm.
If no sperm are found, the surgeon may perform a vasoepididymostomy in which the vas deferens is attached to the epididymis.
After returning the vas deferens to the scrotum, the incision is stitched or closed with surgical glue.
A vasovasostomy takes between three to four hours to complete.
A follow-up visit is scheduled two weeks later to assess healing. At six weeks, the first semen analysis is performed. Depending on when you had the vasectomy and other factors, it can take one month to one year for the sperm count to return to viable levels.
Related: Is Male Birth Control on the Horizon?
Summary
A vasectomy is a surgical form of contraception in males. It involves cutting the vas deferens which transports sperm to your semen. The in-office procedure takes 30 minutes or less to perform under local anesthesia. Healing takes around a week, and many people can return to work the next day.
While a vasectomy is highly effective, you need to use other forms of birth control until your healthcare provider confirms that your sperm count is zero or your sperm is non-moving. Side effects include pain, swelling, and bleeding.
Vasectomy reversal surgery is available if you later change your mind and want to have kids. Success rates are relatively high if you had a recent vasectomy and gradually decline thereafter.
Read Next: Other Types of Permanent Birth Control
Read the original article on Verywell Health.

