Understanding Migraine-Related Brain Lesions on Your MRI
Medically reviewed by Nicholas R. Metrus, MD
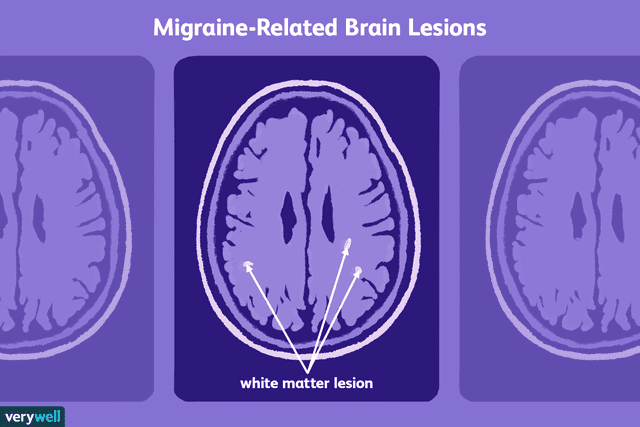
Research indicates that migraines are associated with lesions in the brain called white matter hyperintensities (WMH), as seen on a magnetic resonance imaging (MRI) scan. A lesion occurs because of some sort of damage to the part of the brain where it's located.
Experts don't know whether or not these migraine-related brain lesions may have a long-term effect on your health. However, migraine is linked to an increased risk of stroke and dementia, and WMH lesions are seen in people who develop those conditions.
Scientific studies looking into the potential effect of these lesions on your migraine and overall health are important not only for the future of migraine therapy but also to provide further insight into the brain mechanism behind migraines.
This article will discuss the research into brain lesions in migraine, the characteristics of people with migraine who develop them, and their possible significance.
Migraines and the Brain
Multiple studies have found that people with migraines have an increased risk of brain lesions.
White matter hyperintensities are lesions that appear bright white on certain sequences of MRI scans. These abnormalities can also be seen in older people and people with stroke and dementia. In people with migraine, they're typically found in the frontal lobe, limbic system, and parietal lobe of the brain.
A 2023 meta-analysis of 30 studies found that 44% of people with migraine had white matter hyperintensities, which was significantly higher than healthy people without migraine.
Experts have been trying to piece together the precise cause of these brain lesions, deciphering whether they're caused by the effects of migraine itself or by some other factor specific to people with migraine.
Related: A Guide to the Anatomy of the Brain
What the Research Shows
While it's clear that migraine is a risk factor for developing subclinical brain lesions, the causes, nature, and long-term outcomes are still uncertain, and the research is somewhat inconsistent.
Various studies have looked at the characteristics of people with migraine who have WMH. The 2023 meta-analysis of 30 studies concluded that these lesions were more common in people who have migraine with aura compared to those who have migraine without aura.
Increased age and the presence of hypertension (high blood pressure), diabetes mellitus, and right-to-left shunt (a heart condition in which some of your blood isn't oxygenated in the lungs) were associated with WMH in people with migraine in the 2023 study.
This study also did not find an association between the characteristics of the subjects' migraine pain and aura with the presence of WMH.
As far as other causes for brain lesions, a 2015 study examined the relationship of other cardiovascular risk factors (factors that increase your chance of having a stroke or heart attack), like smoking, body mass index, and high cholesterol, to the presence of white matter hyperintensities in people with migraine.
The results indicated that these cardiovascular risk factors weren't associated with WMH in people with migraine, and other studies have shown similar results. The authors suggest that the effects of migraine itself may be the direct cause of the brain lesions.
The Significance of Brain Lesions
The significance of WMH for people with migraine is not fully known.
A number of studies have examined older people who do not have migraines but have white matter hyperintensities, and these lesions are associated with an increased risk of stroke, dementia, and thinking problems. Since migraine is associated with stroke, it's possible that lesions in people with migraine could be an indication of a higher risk of stroke.
WMH lesions are also seen in people with multiple sclerosis, a condition in which the immune system attacks the protective myelin coating of nerve cells. People with MS have a higher incidence of migraine. The underlying cause of WMH is likely different in these two conditions, but it is an area of research.
If migraines and their associated brain lesions are found to have long-term neurological effects, this may alter the way neurologists treat episodic migraines. For example, healthcare providers may consider migraine preventive medication for episodic migraines in certain people who are at high risk for developing brain lesions or who already have them.
Related: Medications to Prevent Episodic Migraines
Summary
If you have migraine and an MRI shows brain lesions, discuss the implications with your healthcare provider. Stay on top of your migraine health by regularly following up with a healthcare provider, taking your medication as prescribed, and monitoring your triggers. Further research may show what these lesions may mean for the long-term health of people with migraine.
Read the original article on Verywell Health.

