Types of Arthritis and Rheumatic Diseases
Medically reviewed by Anita C. Chandrasekaran, MD, MPH
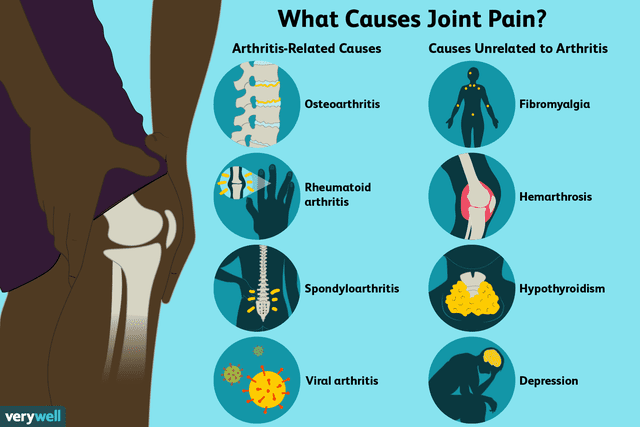
Rheumatic diseases are those characterized by inflammation and impaired function of one or more connecting or supporting structures of the body. There are more than 100 different types of rheumatic diseases, including arthritis and its various types, which are conditions that specifically produce joint inflammation. Pain, stiffness, and swelling are common symptoms associated with rheumatic diseases, but there can also be systemic effects with certain conditions.
In the United States, the most common rheumatic diseases are (in order of prevalence) osteoarthritis, gout, and rheumatoid arthritis. It is estimated that 52.5 million people in the U.S. have arthritis or one of the rheumatic diseases, according to the Centers for Disease Control and Prevention (CDC).
Common Types
Although you may be most familiar with osteoarthritis, there are many different types of arthritis and other rheumatic diseases that can affect the body.
Ankylosing Spondylitis
Ankylosing spondylitis is a type of arthritis primarily characterized by chronic inflammation of the joints and ligaments of the spine. Pain and stiffness start in the spine and can progress to the neck and hips as the disease progresses. Over time, the bones in the spine can fuse, causing loss of mobility and, in advanced cases, spinal deformity.
The exact cause of ankylosing spondylitis is unknown, but it's believed to have a genetic component. The disease primarily affects men, with the typical onset between the ages of 17 and 35. It can occur in anyone, though, at any age.
Ankylosing spondylitis is a progressive disease. Treatment can help manage pain and slow the progression.
Related: What Is Ankylosing Spondylitis?
Bursitis
Bursitis is a condition caused by inflammation of a bursa. Bursae are small, fluid-filled sacs that act as cushions to reduce friction between bone and other moving parts, such as muscles and tendons.
Symptoms of bursitis include pain, stiffness, swelling, and warmth around the affected joint. Pain is often worse during and after activity. Most commonly, bursitis affects the shoulders, elbows, knees, and hips.
The most common cause of bursitis is repetitive joint overuse. Other causes are prolonged pressure to the bursa or injury.
Most cases of bursitis resolve within a few months with minimal treatment. Over-the-counter (OTC) pain relievers, ice, and rest can help relieve pain while a bursa heals. If the pain is persistent despite conservative treatment, steroid injections may be used. The symptoms can be caused by other medical conditions, so it's important to see your healthcare provider to get an appropriate diagnosis and guidance for treatment.
Related: An Overview of Bursitis
Enteropathic Arthritis
Enteropathic arthritis is an inflammatory condition linked to inflammatory bowel diseases (Crohn's disease and ulcerative colitis).
Enteropathic arthritis symptoms and severity varies from person to person. It can cause pain and stiffness in the joints, especially the knees, hips, ankles, and lower back. It may also cause body aches. It's a chronic condition, and you can get flares that come and go.
Some of the treatments often used to treat arthritis can make inflammatory bowel diseases worse, so treatment planning requires careful consideration. TNF inhibitors have successfully been used to treat this disease.
Related: An Overview of Enteropathic Arthritis
Gout
Gout—a form of arthritis—is characterized by the sudden onset of intense pain, tenderness, warmth, redness, and swelling due to inflammation of an affected joint. It most commonly affects the big toe, but can also affect other joints in the foot, elbows, wrists, and fingers.
Excess uric acid in the body and deposition of uric acid crystals in the affected joint and tissues cause the symptoms. With gout, you'll have acute flares that last several days followed by periods with no symptoms. Without treatment, flares get progressively worse.
Men are more likely to develop gout, as are those with kidney problems or who are obese. Certain medications, like diuretics, also raise your risk of the disease. And diseases that increase cell turnover, such as psoriasis, also increase the risk because uric acid is a normal byproduct of cell turnover.
Gout is diagnosed by lab testing coupled with a physical exam. The gold standard for diagnosis of gout is a joint aspiration/arthrocentesis, demonstrating intercellular urate crystals within the affected joint. Imaging tests can also be used to check for joint damage.
Reducing uric acid in the blood is key to managing gout. This is accomplished through diet and/or uric acid-reducing medications. Anti-inflammatory medicines, rest, and ice can help relieve pain during gout attacks.
Related: Gout
Juvenile Idiopathic Arthritis
Juvenile idiopathic arthritis (JIA) is a type of arthritis that affects children 16 years old and under. There are seven recognized subtypes of juvenile idiopathic arthritis.
Signs of juvenile idiopathic arthritis include typical arthritis symptoms of joint pain, stiffness, and swelling. But some forms of JIA also cause fever, skin rash, a swollen spleen or lymph nodes, eye inflammation, weight loss, and anemia.
Unfortunately, there isn't a simple test that can be used to diagnose JIA. Diagnosis can be made more difficult because young children can have trouble verbalizing exactly what they're feeling, and aches and pains can be caused by many other issues. Healthcare providers diagnose JIA by reviewing your child's medical history and symptoms, along with results from various lab tests.
Observing your child can help with diagnosis, especially with young children. Do they have trouble running or walking up stairs? Do they seem stiff or reluctant to move first thing in the morning? How long have you noticed these issues? This is all information to relay to the healthcare provider.
Juvenile idiopathic arthritis is managed through pain-relieving drugs, anti-inflammatory and/or anti-rheumatic medications, and often physical therapy.
Related: An Overview of Juvenile Idiopathic Arthritis
Osteoarthritis
Osteoarthritis is a degenerative joint disease that is considered the most common type of arthritis. It is caused by the breakdown of cartilage in one or more joints.
Also called "wear-and-tear" arthritis, osteoarthritis causes pain, stiffness, limited range of motion, joint inflammation, creaking or grinding of the joints, and joint instability.
People of any age can develop osteoarthritis, but it's most common after age 65. Repetitive joint motion, prior injury to the affected joint, and being overweight also put you at risk for developing this disease.
Osteoarthritis is a progressive disease, but early diagnosis and treatment help slow joint damage and relieve pain. In addition to pain-relieving drugs and anti-inflammatories, lifestyle considerations like gentle exercise and weight loss can be extremely helpful.
Related: An Overview of Osteoarthritis
Osteoporosis
You may not think of osteoporosis as a rheumatic disease, but it is. Osteoporosis is characterized by progressive bone thinning (i.e., decreased bone density) and, consequently, a high fracture risk. It's called a "silent disease" because it shows little to no symptoms until a fracture occurs.
Osteoporosis is more common in women than men, especially those with a small build and those who are white or Asian. It can occur at any age but most often develops after age 50.
You can reduce your risk of developing osteoporosis by helping your body build strong bones. Adequate calcium and vitamin D intake, and regular weight-bearing exercise are crucial to build and maintain bone health.
There are treatments that can help prevent further bone loss as well as newer medicines that promote new bone formation.
Related: An Overview of Osteoporosis
Polymyalgia Rheumatica
Polymyalgia rheumatica is a rheumatic condition characterized by musculoskeletal pain and stiffness in the neck, shoulders, and hips lasting at least two weeks. Polymyalgia rheumatica may also cause flu-like symptoms like fever, fatigue, and weight loss.
There is no test for polymyalgia rheumatica, so diagnosis is made by reviewing symptoms and ruling out other diseases. It's most common in women over 50, with peak incidence between age 70 to 80.
Polymyalgia rheumatica is treated with low-dose corticosteroids. Sometimes steroid-sparing agents, such as methotrexate, or biologics like Kevzara (sarilumab), are used to help manage refractory disease. Symptoms typically improve within a few days of beginning treatment. Typically treatment lasts a year, but it could take up to 5 years.
Related: An Overview of Polymyalgia Rheumatica
Pseudogout
Pseudogout is a condition that develops when calcium pyrophosphate crystals accumulate in a joint and the tissues that surround the affected joint. It's often mistaken for gout because the symptoms are nearly identical (sudden pain, swelling, and stiffness of the joints). One difference is that pseudogout most often affects the knee instead of the big toe.
Pseudogout affects both men and women about equally, and your risk of developing it increases with age. Pseudogout can be diagnosed by drawing joint fluid and looking for calcium pyrophosphate crystals.
Although it can't be cured, pseudogout can be controlled with NSAIDs and low-dose colchicine. If you are unable to take these medications, low-dose steroids may be recommended.
Related: An Overview of Pseudogout
Psoriatic Arthritis
Psoriatic arthritis is a rheumatic disease associated with psoriasis and chronic joint symptoms, which can develop separately. In most cases, psoriasis develops first and arthritis develops over time. And sometimes arthritis develops first, then psoriasis develops.
Psoriatic arthritis is an autoimmune disease, so it occurs when the body's immune system turns on itself. This causes inflammation, pain, stiffness, and skin lesions.
Treating psoriatic arthritis typically involves NSAIDs, anti-rheumatic drugs, and biologic drugs such as TNF blockers. Psoriatic arthritis can't be cured but can be controlled.
Related: Rheumatoid Arthritis and Diabetes: What Is the Relationship?
Rheumatoid Arthritis (RA)
Rheumatoid arthritis is a chronic, autoimmune, inflammatory type of arthritis with joint complications and potential systemic effects. Fever, weight loss, fatigue, and lost-lasting morning stiffness are symptoms of RA, in addition to joint pain and swelling.
While the exact cause isn't known, some of a person's risk is inherited. You have up to a five-fold greater risk of developing the disease if there is a history of it in your family.
Diagnosis is made through a combination of physical exams, lab, and imaging tests.
Rheumatoid arthritis is a progressive disease that isn't curable but is manageable. There are many treatment options available to help control the disease including corticosteroids, NSAIDs, and biologic-response modifiers.
Related: Rheumatoid Arthritis
Sjögren's Syndrome
Sjögren's syndrome is an autoimmune, inflammatory disease characterized by dry mouth and dry eyes that can occur as a primary or secondary condition. Other symptoms can include difficulty chewing and swallowing, sore throat and tongue, digestive problems, enlarged lymph nodes, and swollen joints.
The vast majority of people with Sjögren's syndrome are female. Genetic factors, viral infections, and hormonal factors may play a role in its development. There is an increased risk of lymphoproliferative disorders, particularly lymphoma, with Sjogren's.
Treatment for Sjögren's is different for everyone. Depending on your symptoms, there are treatment options to help relieve dry mouth, dry eyes, and painful joints.
Related: An Overview of Sjögren's Syndrome
Lupus
Lupus (systemic lupus erythematosus) is an autoimmune, inflammatory disease that can affect the joints, skin, kidneys, lungs, heart, nervous system, and other organs of the body. Symptoms vary widely between individuals, but can include muscle and joint pain, fatigue, and fever.
The exact cause is unclear, but environmental factors, genetic, and reaction to certain drugs may play a role. Because of the wide range of symptoms, and the fact that there is no single diagnostic test for lupus, diagnosis is difficult.
Lupus can't be cured but can often be managed. Treatment varies depending on your symptoms and their severity. You and your healthcare provider must work closely to develop the right treatment plan for you.
Related: An Overview of Lupus
Tendonitis
Tendonitis is a condition caused by inflammation of one or more tendons in the body. Symptoms include pain and tenderness of the joint, stiffness, cracking of the joint, and a lump on the tendon.
Tendonitis is most often caused by repetitive overuse of the tendon. It can also be caused by an injury or due to other inflammatory disorders (e.g., rheumatoid arthritis).
Rest and restricted movement of the affected joint is the best treatment for tendonitis. In some cases, physical therapy may also be needed. Corticosteroids may be prescribed for chronic tendonitis.
Related: An Overview of Tendonitis
Rare Types
There are a few rarer types of arthritis and rheumatic diseases that can develop as well. Given how often they occur, they may be considered only after more common types of rheumatic disease have been ruled out.
Mixed Connective Tissue Disease
Mixed connective tissue disease (MCTD) is an autoimmune disease that features overlapping symptoms of at least two connective tissue disorders: systemic lupus erythematosus, systemic sclerosis, polymyositis, dermatomyositis, rheumatoid arthritis, and sometimes Sjogren's syndrome. In addition to joint pain, symptoms include muscle pain or weakness, low-grade fever, fatigue, and Raynaud's syndrome.
The cause of MCTD isn't known, but there may be a genetic component. It's much more prevalent in women than in men, especially young women.
This disease is very difficult to diagnose because its symptoms overlap with other diseases, and the symptoms don't occur all at the same time. The distinguishing point with MCTD is the high concentrations of anti-U1 RNP (ribonucleoprotein) in the blood.
Treatment involves managing symptoms with anti-inflammatory medications, pain relievers, and other drugs as needed. Treatment is dependent on the severity of the symptoms.
Related: An Overview of Mixed Connective Tissue Disease (MCTD)
Polymyositis
Polymyositis is characterized by inflammation and degeneration of the muscles. It typically begins with muscle groups closest to the trunk but can affect other muscles over time. Muscles progressively get weaker to the point of affecting daily life.
Polymyositis develops gradually. It's most common in women between the ages of 40 and 60, but anyone may develop it at any age. It often occurs alongside other rheumatic diseases and certain cancers. While there's no known cause, genetics seem to factor in.
High-dose corticosteroids and/or immunosuppressants are considered first-line treatments. With early and aggressive treatment, it's possible to achieve remission.
Related: An Overview of Polymyositis
Reactive Arthritis
Reactive arthritis is a type of arthritis that occurs as a reaction to an infection somewhere in the body. Besides joint pain and stiffness, reactive arthritis also causes eye inflammation and inflammation of the urinary tract.
Reactive arthritis is often triggered by an infection in the bladder, urethra (men), or vagina (women). It can also be triggered by an infection in the digestive tract caused by bacteria-contaminated food.
Most people fully recover from reactive arthritis within a year of developing it. Treatment can help manage symptoms until that time.
Related: An Overview of Reactive Arthritis
Septic Arthritis (Infectious Arthritis)
Septic arthritis, also called infectious arthritis, is an infection that develops in a joint. It is caused by a pathogen (bacterium, virus, or fungus) that enters the body through any open wound and travels through the body to a joint.
Typically only one joint is affected, but septic arthritis can affect several joints at once. The symptoms include pain (often severe and that comes on quickly), stiffness, and swelling of the affected joint. Infectious arthritis may also cause fever, chills, fatigue or weakness, and nausea.
Takeaway
Septic arthritis is a medical emergency. It can cause severe damage to the joint in question. It can also lead to septic shock, which can be fatal if left untreated. If you or your loved one have symptoms, see a healthcare provider immediately.
Anyone can develop septic arthritis, but it's most common in the very young and the elderly, and those with a compromised immune system. Diagnosis of septic arthritis is made through blood tests and synovial fluid analysis, to check for signs of infection.
Treatment of septic arthritis can involve antibiotics, surgical irrigation or debridement. Prompt treatment can reduce the amount of long-term damage caused to the joint.
Scleroderma
Scleroderma is an autoimmune disease characterized by the abnormal growth of connective tissue that supports the skin and internal organs. There are two main types of scleroderma: localized and systemic.
Localized scleroderma causes affected areas of the skin to become hard and tight. Systemic scleroderma affects the skin, as well as organs and blood vessels.
There is no cure for scleroderma, but treatment can help control symptoms.
Related: An Overview of Scleroderma
Vasculitis
Vasculitis is a condition associated with inflammation of the blood vessels. It develops when your immune system mistakenly attacks the blood vessels, causing inflammation that restricts normal blood flow. Symptoms include pain, fever, loss of appetite, and various other signs depending on what areas of the body are affected.
Immunosuppressants and anti-inflammatories are often prescribed to treat vasculitis. Early treatment is key to help limit tissue and organ damage, as well as control symptoms.
Related: An Overview of Vasculitis
Takeaway
Fibromyalgia, characterized by widespread or generalized muscular pain, tender points, fatigue, digestive problems, sleep disturbances, and other assorted symptoms, used to be considered an arthritis-related or rheumatic syndrome. It is not considered an arthritis-related syndrome or a rheumatic disorder anymore. It is now considered a central nervous system disorder characterized by a hypersensitive sensory processing system.
Challenges With Diagnosis
If you suspect you have arthritis or another rheumatic disease based on early symptoms, consult your healthcare provider. Know, though, that diagnosis can be complicated and may take time; some rheumatic diseases have overlapping symptoms and may mimic one another. Your diagnosis is based on your medical history, a physical examination, laboratory tests, imaging studies, and in some rare cases, a tissue biopsy.
A rheumatologist is a specialist in the diagnosis and treatment of arthritis and rheumatic diseases. While you may begin the diagnostic process with your primary care provider, you may need a rheumatologist to distinguish between the different conditions and set you on the right treatment path.
A Word From Verywell
These types of arthritis and rheumatic diseases are the most well-known, but the list is not exhaustive. There are more and some are quite rare. An early, accurate diagnosis is imperative to managing rheumatic diseases, and treatment options for rheumatic diseases depend on which specific disease or condition you have.
Related: Psoriatic Arthritis vs. Sacroiliitis: What Are the Differences?
Read the original article on Verywell Health.

