How Is Type 1 Diabetes Treated?
RichLegg / Getty Images
Medically reviewed by Danielle Weiss, MD
Type 1 diabetes is a chronic (long-lasting) autoimmune condition in which the pancreas makes little or no insulin. The pancreas contains beta cells that produce insulin, a hormone that helps the body convert glucose (a type of sugar) into energy. When a person has type 1 diabetes, the body’s immune system destroys beta cells. This causes beta cells to stop creating insulin.
Without insulin, glucose in the blood builds up and the levels become too high. When left untreated, high blood sugar levels can damage the kidneys, eyes, heart, and nerves. It can also lead to complications such as diabetic ketoacidosis.
There isn’t a cure for type 1 diabetes, but the condition can be managed with medical treatments and lifestyle changes. The main goals of type 1 diabetes treatment are to achieve normal or near-normal blood sugar levels and prevent or limit diabetes-related complications.
Day-to-day monitoring of your blood sugar levels will be mostly managed by you. However, guidance and support will come from your primary care provider and other members of your healthcare team like an endocrinologist (doctors who treat conditions related to your hormones). Routine check-ups and lab tests will be used to monitor and necessary adjustments to your treatment plan.
Insulin
In type 1 diabetes, insulin-producing beta cells are destroyed by the immune system. As a result, the pancreas produces little to no insulin. If you were diagnosed with type 1 diabetes, taking insulin will be an essential part of your treatment plan.
Insulin helps regulate (or, normalize) your blood sugar levels. The insulin you’ll take to treat your type 1 diabetes is a man-made version of the hormone produced by a healthy pancreas.
There are different ways to take insulin. The most common methods to takin insulin include using a needle and syringe, an insulin pen, or a small portable device called an insulin pump. Less common methods include inhalers, injection ports, and jet injectors. Insulin is not available in pill form.
When using insulin to manage your glucose levels, there are three terms to keep in mind. These terms are:
Onset: How long it takes for the insulin to start lowering your blood sugar.
Peak time: The amount of time it takes for insulin to reach its maximum strength.
Duration: How long the insulin continues to work once it’s in your body.
There are many types of insulin available. In general, insulin is classified by how long it takes to work and how long it remains active. Insulin is categorized as:
Rapid-acting: Onset about 15 minutes after injection, peaks in about one hour, and has a duration of two to four hours. Rapid medications include: Admelog, Humalog, Lyumjev (insulin lispro); Fiasp and NovoLog (insulin aspart); Apidra (insulin glulisine)
Regular or short-acting: Onset about 30 minutes after injection, peaks in about two to three hours, and has a duration of three to six hours. Humulin R (insulin regular) is a type of short-acting medication.
Intermediate-acting: Onset about two to four hours after injection, peaks in about four to 12 hours, and has a duration of 12 to 18 hours. Medications include: Humulin N (insulin NPH); and, Humalog Mix (insulin lispro protamine)
Long-acting: Onset two hours after injection, does not peak, and evenly lowers glucose levels over a period of up to 24 hours. Medications include: Basaglar, Lantus, Semglee (insulin glargine); and, Levemir (insulin detemir)
Ultra-long acting: Onset six hours after injection, does not peak, and evenly lowers glucose levels over for 36 hours or longer. Medications include: Tresiba (insulin degludec); and, Toujeo (insulin glargine 300 units/mL)
Related:How Much Insulin Do You Need?
Glucose Monitoring
Glucose monitoring allows you to understand how your body processes sugar and responds to insulin. It’s a quick way to know what’s working in your type 1 diabetes treatment and management plan.
Thanks to improvements in technology, glucose monitoring devices take the guesswork out of managing your type 1 diabetes. Glucose monitoring can be done in two ways: a blood glucose monitor and a continuous glucose monitor:
A blood glucose monitor (BGM) uses fingersticks to get small samples of blood. These small devices analyze the blood samples to measure glucose levels.
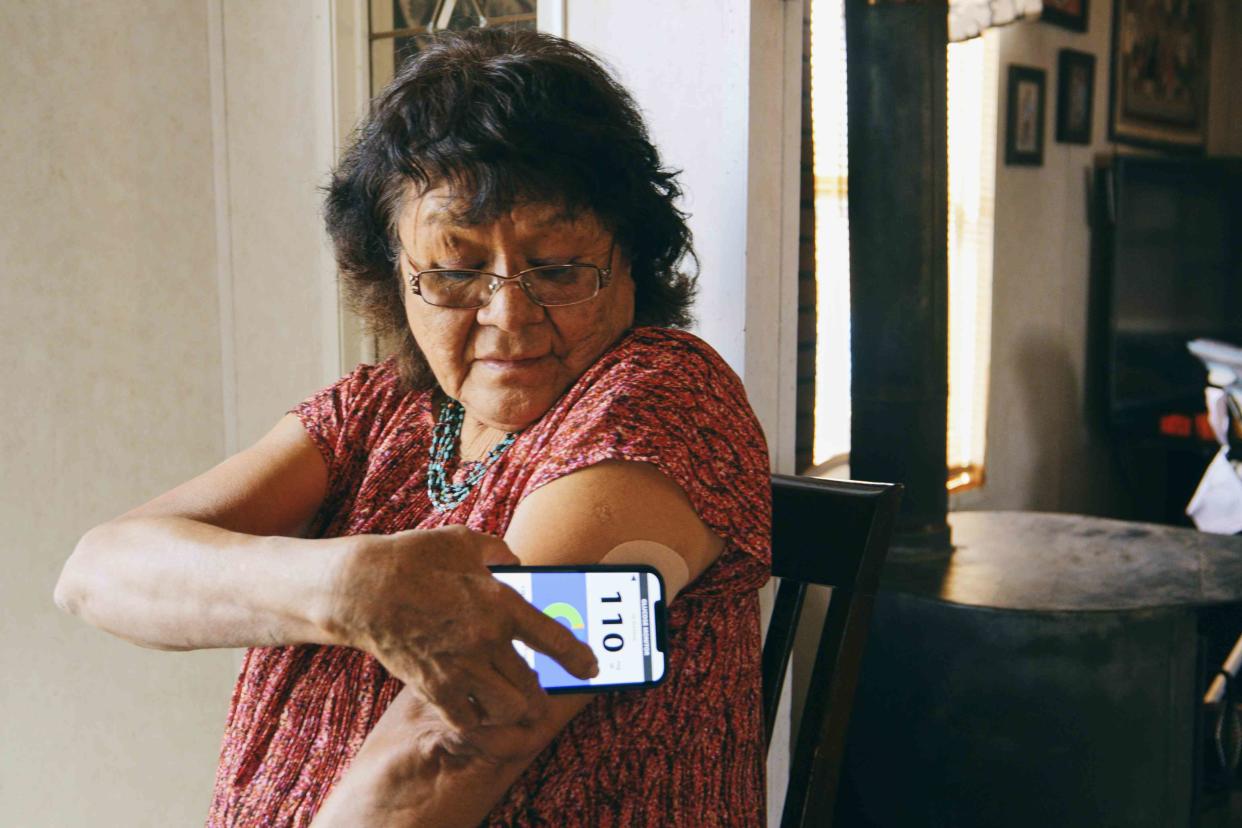
A continuous glucose monitor (CGM) uses a small sensor to measure glucose levels in the fluid under the skin. The sensor (with an attached transmitter) is held in place on the skin with a sticky patch. The continuous glucose monitor wirelessly transmits the glucose reading to a recording device or smartphone. In some cases, a CGM may be part of an insulin pump.
Lifestyle
Treating type 1 diabetes requires a well-rounded approach to avoid a sudden drop or spike in blood sugar. Managing blood sugar may involve changes in exercise routines, dietary patterns, and stress. Your healthcare provider may suggest the following lifestyle changes:
Don't smoke: Consuming nicotine increases your blood sugar levels, which means you need to use more insulin to keep your levels balanced.
Eat a well-balanced diet: Make sure your meals include fruits, vegetables, whole grains, lean meats, and proteins. Learn which foods raise or lower your blood sugar level. Include heart-healthy fats found in olive oil, avocados, nuts, and seeds.
Limit foods high in saturated and trans fats, added sugars, and salt: Eating these foods can affect your blood sugar levels and make it more difficult to keep your levels balanced.
Get regular exercise or physical activity: Talk to your healthcare provider before starting an exercise routine. People living with type 1 diabetes need to take special steps before, during, and after physical activity.
Take care of your emotional health: Practice ways to reduce stress such as listening to relaxing music or meditation. Seek support from trusted family members or loved ones.
Living With and Managing Type 1 Diabetes
Type 1 diabetes is a life-long health condition. Although there is no cure, controlling your blood sugar levels can help prevent or delay complications.
When you first start taking insulin, it may take some time to find the right dose. This is a normal part of managing type 1 diabetes, so try not to be discouraged. Your healthcare provider will teach you how to give yourself insulin injections.
Your healthcare provider will also help you find a dose that works best for you. Your insulin dosage may need to be adjusted from time to time based on factors like:
Exercise and activity level
Food intake
When you are traveling
If you are sick
Keeping your blood sugar within a normal range can help reduce your risk of long-term complications. But sometimes, complications can happen along the way even when sticking to your treatment plan. Stay in contact with your healthcare team and update them on any changes in your symptoms.
A Quick Review
Although there is no cure for type 1 diabetes, many people with the condition live full and healthy lives. Treatments are available to manage insulin and glucose levels and prevent complications.
Your treatment plan may require trial and error, lifestyle adjustments, and glucose monitoring. Keep your healthcare team updated on changes in your symptoms or any challenges you may experience with treatment.
For more Health news, make sure to sign up for our newsletter!
Read the original article on Health.

