What Is Tinea Capitis?

Boy_Anupong / Getty Images
Medically reviewed by William Truswell, MD
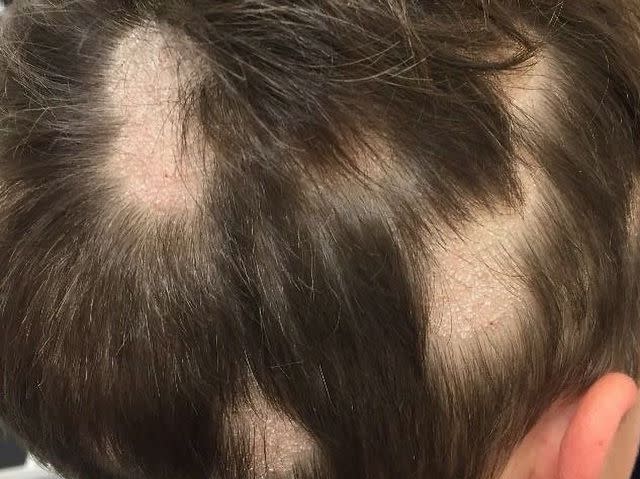
Tinea capitis (also more commonly known as ringworm of the scalp) is a common fungal infection that affects your scalp and hair follicles. Despite its name, this infection is not caused by a worm but by various types of fungi known as dermatophytes. This infectious is highly contagious and causes symptoms like an itchy scalp, hair loss, and redness.
Fortunately, there are effective treatments available to help reduce symptoms. The gold standard treatment for tinea capitis is antifungal medications, but some home remedies can also help support your scalp health.
Types of Tinea Capitis
Fungi called dermatophytes cause tinea capitis. More specifically, the Microsporum and Trichophyton species of fungi are the primary culprits of this infection. These fungi can invade the protective outer layer of your hair follicles and sometimes attack the hair shaft itself. If you develop these fungi, you may experience one of the two types of tinea capitis:
Inflammatory tinea capitis: Causes significant inflammation on your scalp, which may cause redness, swelling, pus-filled bumps, tenderness, and pain on your scalp or hair loss in severe cases
Non-inflammatory tinea capitis: Doesn't cause significant inflammation or hair loss, but scaly patches and swelling may occur
Symptoms
Most people who develop tinea capitis are young children between the ages of 3 and 14. But, anyone can catch this infection. If you experience tinea capitis, you may have one or more of the following symptoms:
Frequent head-scratching
Circular or oval patches
Redness and inflammation
Scaly or dry skin on your scalp that resembles dandruff
Brittle or weak hair
In more severe cases of inflammatory tinea capitis, hair loss, swollen lymph nodes, and pus-filled sores or abscesses may occur.
It's important to note that symptoms of this fungal infection can vary from person to person, so it's possible that you may not experience all of these symptoms. However, if you suspect you have a scalp ringworm, it's essential to see your provider for proper diagnosis and treatment.
DermNet NZ
Causes
While the name "ringworm" may imply a parasitic worm, the culprit behind this condition is not a worm at all but rather a group of fungi known as dermatophytes. These fungi thrive on keratin, a protein found in your hair, nails, and the outermost layer of your skin.
Tinea capitis is highly contagious and the following factors can increase your risk of developing symptoms:
Making direct contact with someone who has the infection, such as through touching their hair or sharing hats and hairbrushes
Living in a hot and humid climate where these fungi can thrive and spread more easily
Not washing your hair often enough, especially after sweating or a rigorous workout
Having cuts or scrapes on your scalp, making it easy for fungi to penetrate the skin
Diagnosis
If you think you may have caught this fungal infection, it's important to see your healthcare provider for proper testing. During your appointment, your provider will ask you about your medical history and current symptoms. They may also use several tests to confirm a diagnosis. These tests include:
Physical exam to visually examine the scalp
Wood's lamp exam which uses ultraviolet (UV) light to check for fungi on your scalp
Skin scraping, which collects a small sample of your scalp skin or hair to test for fungi
Fungal culture test to identify the type of fungi affecting your skin and hair
In rare or more complicated cases, your provider may recommend a skin biopsy—a procedure that removes a small piece of skin from your scalp to confirm a tinea capitis diagnosis and rule out other skin conditions. Your primary care provider will likely work with a dermatologist (a doctor who specializes in skin, nail, and hair conditions) during testing and treatment to provide you with accurate information and recommendations to help reduce symptoms.
Tinea Capitis Treatment
The most common treatment for tinea capitis is an antifungal medication, which usually comes in the form of an oral pill. Generally, you will need to take these medications for four to eight weeks. It's also essential to finish your dose completely and follow your medication plan as directed. Stopping medication (even if you're feeling better) can cause symptoms to come back.
Your healthcare provider may treat ringworm of the scalp with one of these antifungal medications:
Grifulvin V (griseofulvin)
Terbinex (terbinafine)
Onmel (itraconazole)
Diflucan (fluconazole)
In addition to medication, there are steps you can take at home to manage the infection and improve your scalp health. These home remedies include:
Using a medicated shampoo that contains ingredients like ketoconazole or selenium sulfide to slow the spread of the infection
Washing your hair with lukewarm water
Gently cleansing your hair and scalp without trying to scratch or further irritate your symptoms
Immediately putting your towel in the washer with hot water to reduce the risk of fungi spreading
Cleaning your hairbrushes and combs with a mixture of 1 part bleach and 10 parts water to disinfect the objects properly
Avoiding sharing items such as towels, pillowcases, hats, helmets, or hairbrushes with others
How to Prevent Ringworm of the Scalp
Preventing tinea capitis involves adopting good hygiene practices and taking precautions to minimize your risk of fungal infections. Here are some steps to help prevent this condition you can take to prevent this infection:
Wash your hair and scalp regularly with a mild shampoo
Avoid excessive scratching of the scalp, as it can lead to breaks in the skin, making it easier for fungi to enter
Limit sharing combs, hairbrushes, hats, scarves, towels, pillowcases, or other personal items with others
Minimize close contact with people with tinea capitis or other contagious infections until they have received treatment and are no longer contagious
Additionally, if you or someone in your household develops symptoms of tinea capitis, seek medical attention promptly. Early treatment can help prevent the spread of the infection to others.
Related Conditions
It's worth noting that having tinea capitis can also increase your risk of developing other conditions, including:
Tinea corporis: Ringworm of the body which can cause red, scaly, and itchy patches on the skin
Tinea pedis: More commonly known as athlete's foot, which can cause itchiness, scaling, and blistering between the toes and on the soles of your feet
Tinea cruris: Also known as jock itch, which causes a red and itchy ratch on the groin and inner thighs
A Quick Review
Tinea capitis is a common and contagious fungal infection that causes symptoms like an itchy scalp, hair loss, and redness. While this infection mostly affects children, anyone can develop symptoms through direct exposure to someone with tinea capitis or sharing contaminated items like hats or hairbrushes. If you develop this infection, your treatment plan will usually involve taking antifungal medications and practicing hygienic home remedies to help relieve symptoms.
Frequently Asked Questions
Will ringworm on the scalp go away on its own?
Ringworm on the scalp typically does not go away on its own and usually requires treatment with oral antifungal medications prescribed by a healthcare provider. Without proper treatment, the infection may persist and can lead to more severe symptoms and complications.
What kills ringworm on scalp naturally?
Natural remedies alone are often not sufficient to eliminate ringworm on the scalp. If you cannot take antifungal medications, ask your healthcare provider for any alternative therapies or supplements they recommend to aid in your healing.
Should you wash your hair if you have ringworm?
Yes, it is important to maintain good scalp hygiene when you have tinea capitis. Keeping your scalp clean and using a medicated shampoo can help keep the affected area clean and prevent further irritation. However, be gentle while cleansing the scalp to avoid scratching or bleeding, which can worsen your symptoms.
For more Health.com news, make sure to sign up for our newsletter!
Read the original article on Health.com.

