How to Get the Right Team for Your Cancer Care, From Someone Who Did It
"Hearst Magazines and Yahoo may earn commission or revenue on some items through these links."
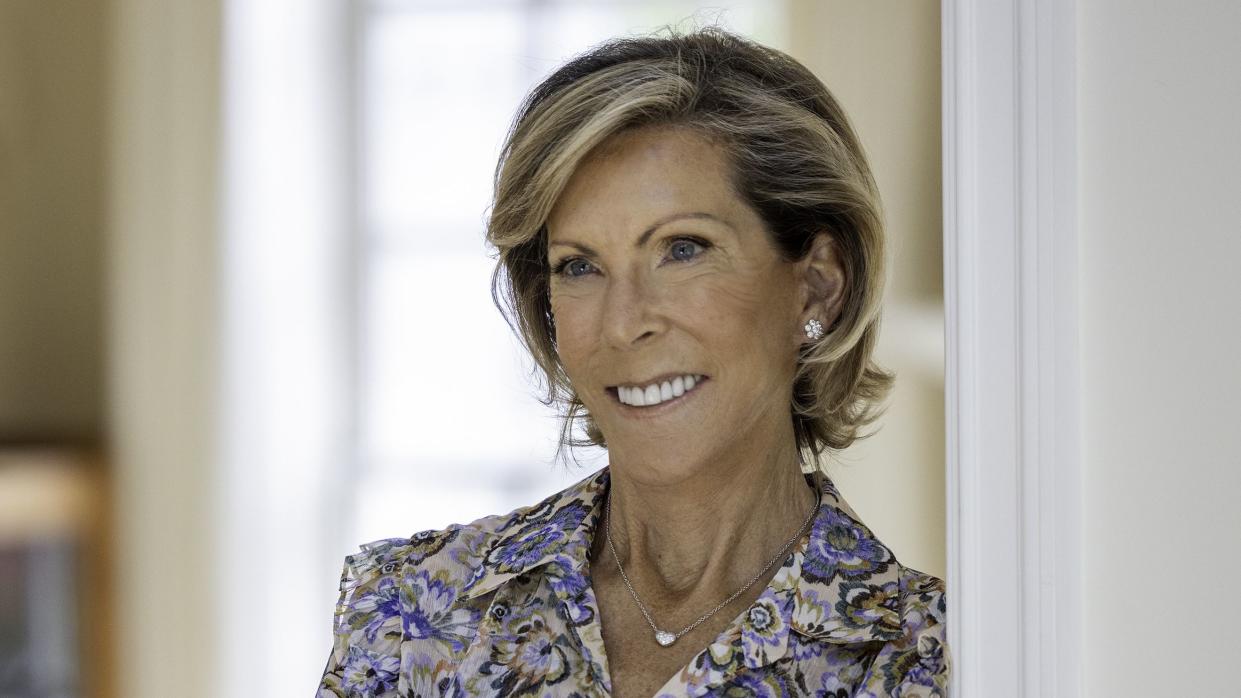
If today you were given a scant three years (or less) to live, what would you do? When I was given a fatal cancer diagnosis more than twenty-five years ago, I was told that’s how long I had.
The road to my cure what not an easy one to walk. I felt encumbered by a system that didn’t have my death sentence in mind. It sparked a level of incalculable drive, forcing me to shift from fear to fearless if I was going to survive.
No matter how fearful we are of our diagnosis, we can find a way to beat the system, to turn the volume down on our fear—to fear less. My new book, Fatal to Fearless, is organized around twelve steps to do just that. Here is my best advice for one of them, on building a team that will support you in every way.
This is how to build a team with the expertise, compassion, and resilience to see you through your full cancer journey, and beyond.
Fatal to Fearless: 12 Steps to Beating Cancer in a Broken Medical System
amazon.com
$30.00
Understand the different types of medical centers
There are different types of medical centers, each with its own benefits and drawbacks. Understanding which centers are best to treat your specific cancer is critical.
NCI-designated centers
The National Cancer Institute recognizes medical centers for their rigorous standards and state-of-the-art cancer research. There are more than seventy of these NCI-designated cancer centers, located in thirty-six states and the District of Columbia. They are funded by the NCI to deliver cutting-edge treatments. There are three different kinds:
comprehensive cancer centers, which have to meet the highest standards and initiate clinical trials;
clinical cancer centers, which conduct clinical research and provide care; and
basic laboratory cancer centers, which do not provide patient treatment and instead focus solely on laboratory research.
All NCI-designated centers renew their status every five years with the National Institutes of Health (NIH). Examples of top- ranked centers include Dana-Farber in Boston, Memorial Sloan Kettering in New York, Mayo Clinic Cancer Center in Rochester, Minnesota, and MD Anderson in Houston, Texas. You can find an NCI-designated cancer center in your region by searching “Find a Cancer Center” on the National Cancer Institute’s site.
Academic medical centers (AMCs)
AMCs contain multiple, distinct layers and are the primary sites for graduate medical education and cutting-edge research (many AMCs are affiliated with a medical school). They are also called teaching hospitals because they work with residents and interns from various medical schools. With physicians, nurses, researchers, and teachers all working in unison at an AMC, patients have better access to the latest medical breakthroughs, resources, and clinical trials at these centers. And many AMCs are conducting bench-to-bedside medicine, meaning they have entire teams of PhD scientists that work in the labs with new ideas and approaches. Those ideas are brought to the clinical community to eventually use at the bedside with patients.
Community hospitals
Community hospitals are your local hospitals. They won’t have the same focus on bench-to- bedside medicine, but they do have their perks and plusses— they are closer geographically, easier to get in and out of, and tend to be friendlier and less intimidating. They may also have contracts with other academic centers. Ask what that partnership truly entails. It may provide access to academic clinicians or clinical trials but it also could be a bit more marketing than true integration.
Select your lead and hospital
Decide who leads, who executes. As I mentioned earlier, you really want to have a lead doctor with deep knowledge and hands-on experience in your particular cancer, combined with a strong local hospital that you’re comfortable with for ongoing execution. If possible, you want that lead doctor to come from an NCI-designated center or equivalent AMC in cancer. Your local execution can be well served by a community hospital. Here are a few tips to help you choose your team:
Base your decision on the oncologist or hospital
You may make your hospital selection based on an oncologist you really clicked with. Or you may have decided on a specific center because it is close to home or specializes in your type of cancer, and now you are selecting the oncologist at that center. Either way should be perfectly fine. Just keep asking which clinician sees the most patients like you.
Base your decision on expertise in your cancer and specialties offered
With over a hundred types of cancer, not every center can excel in each one. Where a patient goes for prostate cancer treatment, for example, can be completely different from a center selected for pancreatic cancer. Sometimes you will see that an AMC has centers of excellence dedicated to specific cancers. Patients with rare tumor types will have to research even harder to identify which hospitals see the most patients and have the most experience (Cancer.net has a landing page dedicated for “Finding Information and Support Resources for Rare Cancers” and includes a list of sites, including links to finding doctors who specialize in a rare cancer).
Become familiar with the resources available to you
Start with making sure which elements of your treatment can be done there. Do they have a strong surgical team, cutting-edge radiation programs, access to new drugs in clinical trials? Can they support you with a navigator or case manager to help you through the logistics of your care? Do they offer psychosocial support or alternative, complimentary programs like meditation, yoga, acupuncture? If you need help with adapting your diet and exercise regimen to your treatment, do they provide relevant support services? Remember to always ask, and never apologize for asking.
Build out your personal team
Friends, family members, and other caregivers can play distinct and crucial roles in providing support for your cancer journey. While the specific roles may vary based on individual circumstances and relationships, here are general considerations when thinking about roles and how to build and work with your support team:

Roles of family members
Caregiving support: Family members often take on a primary caregiving role, providing day-to-day support, managing medications, assisting with personal care tasks, and coordinating overall care. They may accompany you to medical appointments and help navigate the healthcare system. It’s important to communicate openly with your caregiver(s) and show gratitude.
Emotional support: Family members can offer unconditional love, understanding, and emotional support. They can provide comfort, reassurance, and a shoulder to lean on during challenging moments. But family members also come with emotional history and sometimes it might feel safer to talk with a friend.
Decision-making and advocacy: Family members can be helpful in discussing treatment options, making important medical decisions, and advocating for your best interests with your medical team or your insurance.
Long-term support: Family members can assist in managing finances, coordinating insurance claims, or even exploring supportive care options. They can also help create a supportive environment at home by modifying the living space, ensuring accessibility, and organizing necessary equipment.

Roles of friends
Emotional support: Friends can offer a listening ear, empathy, and emotional encouragement. They can provide a sense of normalcy, a source of distraction, and companionship during difficult times.
Practical support: Friends, like family, can help with practical tasks such as running errands, cooking meals, providing transportation to appointments, or assisting with childcare.
Distraction and recreation: Friends can help you relax and enjoy outings or social gatherings that can provide much- needed distraction from the daily challenges of living with cancer.
Advocacy and communication: A close friend can also act as your advocate, helping to communicate your needs, concerns, and preferences to healthcare professionals. They can attend appointments with you, take notes, ask questions, and ensure that your voice is heard and understood.
Integrate your care
Integrate your doctors
The healthcare system doesn’t make it easy for specialists to talk to each other. They tend to work independently, even when they’re in the same hospital. But that doesn’t mean you can’t encourage their integration. You may need to copy each specialist and be clear about your every step. You want to know, for example, when you are shifting from the surgeon or the transplant clinician back to the medical oncologist or the hematological oncologist.
Integrate the centers
This typically means that you’re linking the specialist at an AMC with your local doctors, but it can also mean linking two AMCs. If you don’t do this integration, mistakes can be made. You also need to know when you shift between the lead AMC and local hospital.
Integrate your personal support team
Have open and honest conversations with your potential caregiv- ers about your diagnosis, your treatment plan, and how they can support you. Discuss your expectations and their availability. Keep your team informed about your treatment progress and coordi- nate schedules when necessary. It’s important to establish clear communication channels to keep everyone informed about your needs, your progress, and any changes in your treatment.
Keep all important information easily distributable and in one place
Keep all important information in one place that you can easily distribute to your personal support team. Examples include:
the hospital location, the wing, the parking
the lead doctor’s name, location, and phone numbers
emergency phone numbers
copies of insurance cards
legal information like your medical directive and/or a living will and trust
Put every detail in your phone. You can take photos of the most im- portant documents and save those on your phone, too. You will also want to provide these documents to your personal leads.
Provide a schedule based on information from the medical team— biopsy dates, surgery dates, radiation, check-in appointments. Then go to the treatments knowing in advance what you can expect. Will your treatment be delivered orally or intravenously? If it’s oral, that’s easy, but if it’s an infusion, you’ll want to know more details. How long does it take? How often will it be performed? Know in advance what you’re in for so you can best plan and prepare.
You Might Also Like

