Strokes, delirium and dizziness: Here's what we know about how the coronavirus can affect the brain
When news of a respiratory illness spreading through China first broke, Dr. S. Andrew Josephson — chair of neurology at the University of California, San Francisco — didn’t anticipate that his department would be involved. “When I first heard about it ... I said, ‘This isn’t going to involve my day job,’” Josephson, who is also the editor in chief of JAMA Neurology, tells Yahoo Life.
But within a few weeks of COVID-19 arriving in the United States, patients began showing neurological symptoms, and Josephson realized he was wrong. “It turns out, I care for these patients every day,” he says.
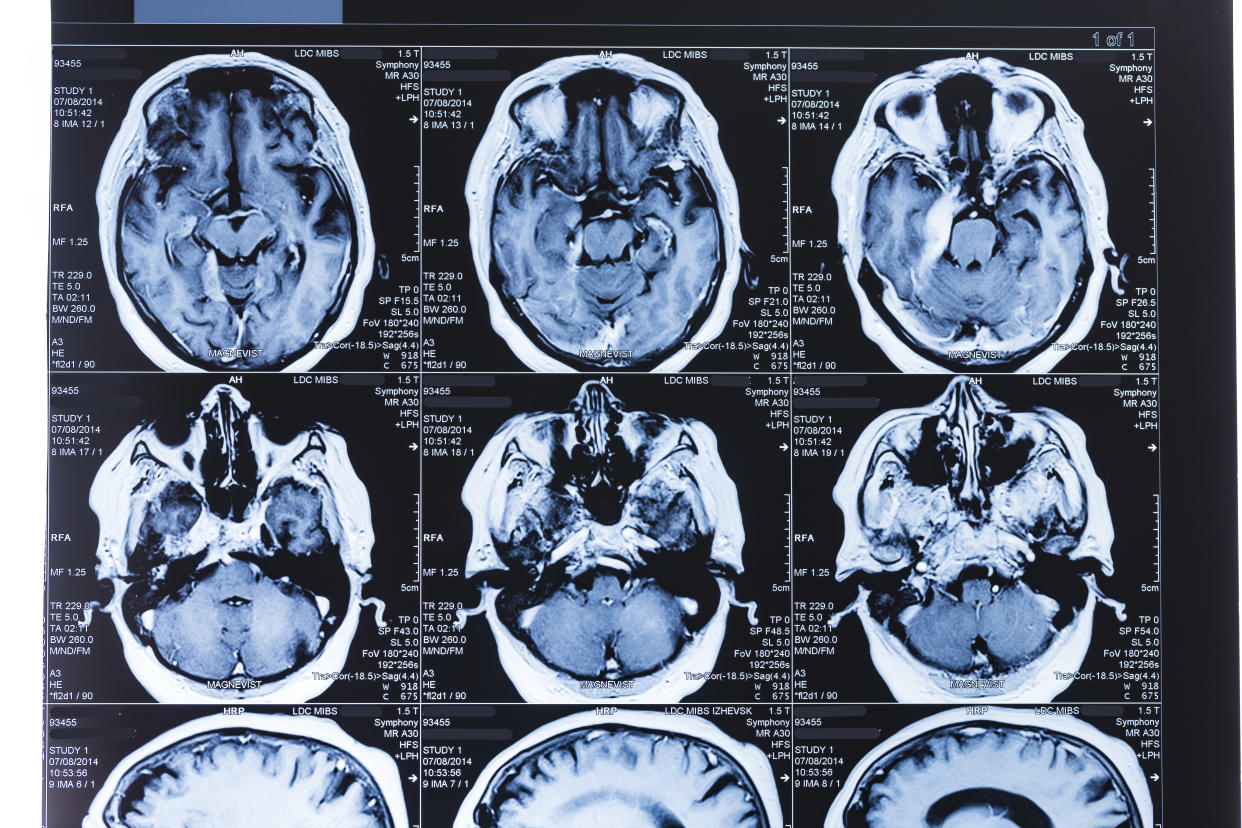
Josephson is one of many studying how the coronavirus affects the brain and why it has been found to cause a variety of neurological symptoms, from stroke to memory loss. He authored an editorial on one of the earliest studies published by JAMA Neurology, in April, in which researchers from Wuhan, China, identified neurological symptoms in many patients with COVID-19.
This week he has his eyes on a new study from the U.K., published by the Lancet, which presents over 120 case reports of individuals with neurological manifestations. While the most common symptom found was stroke (reported in 57 individuals), the study also found 39 instances of patients experiencing an “altered mental status” — defined as “an acute alteration in personality, behavior, cognition or consciousness.”
Josephson says this phenomenon, which predates COVID-19, is referred to by many names, such as ICU delirium, hospital delirium or — the official term used in the neurology world — encephalopathy. To help clarify what that means and what we know about COVID-19 and the brain thus far, Yahoo Life spoke about it all with Josephson. Here’s what he had to say.
Yahoo Life: How long have experts known that this coronavirus can cause neurological symptoms?
Josephson: When coronavirus first came out, we were all taught this is a respiratory illness and the bad things that come of it are the lungs. ... And I think starting with that Wuhan report, we began to realize that there were a lot of people who had neurologic and psychiatric manifestations from this disease. Some of them are relatively nonspecific things like confusion, dizziness, headache.
And what about specific things?
The specific things we’ve heard about are things like stroke, encephalopathy ... we’ve heard about people who obviously lose their sense of smell. And so this preponderance of evidence suggests that neurological psychiatric problems are relatively common, at least in these two studies, and at least in people who are ill enough to be in the hospital.
Is it clear what’s causing so many strokes in COVID-19 patients?
The striking incidents of stroke probably has to do with blood clots forming in the body and with the heart being affected — both of which can lead to stroke.
On the psychiatric front, we’ve heard from COVID-19 survivors who have had harrowing experiences in the ICU, sharing stories of hallucinations, pulling out their own breathing tubes and fearing that the nurses were trying to kill them. Can you help explain exactly what ICU delirium is — if that’s the right term?
There are a million different names for it: delirium, ICU delirium, encephalopathy, confusion, altered, mental status. We’re all talking about the same thing, which is people who are ill in the hospital, not thinking straight. Right now we’re trying to figure out how much of that is due to a problem with the brain and how much is due to the fact that when somebody who’s elderly, or someone who’s really sick, ends up in the hospital, the incidence of confusion is very, very high. Some of it likely has to do with underlying disease, but some of that has to do with the confusing environment that’s going on in the hospital and the person’s underlying susceptibility to that. We do know it happens more in older people because presumably some of those people have underlying beginnings of problems of aging in the brain and therefore they’re not as resilient. A younger person, when they go into the hospital, that doesn’t typically occur very often.
It also seems like the high rate of delirium with this virus may be influenced by the fact that many of the things that help normalize this environment have been taken away, is that correct?
Exactly. One of the things we do to treat delirium or prevent delirium is that we know the hospital is a very unusual environment, especially the ICU. So we do things to people to help patients by bringing in their family, making it look more realistic, not having bells and alarms go off every five seconds. Well, someone who’s sick, especially in a pandemic when visitors are not allowed, all of these risk factors for delirium are exacerbated, and that’s a real problem.
Is it clear how the coronavirus is causing these reactions?
That’s the big question that is yet to be figured out ... how much of this is nonspecific. In other words, if you take an old person who’s really sick with any virus, let’s say influenza, when they go into the hospital a lot of them become confused, a lot of them get dizziness, a lot of them get headaches. So how much is just that it’s a sick person in the hospital — because we know the brain doesn’t like that for a variety of reasons — and how much of it is specific to coronavirus?
So it may be that these neurological and psychiatric reactions aren’t as connected to the virus as they seem?
[We’re trying to figure out] how much of this is due to actual invasion of the virus of the nervous system — meaning how much of it is that the virus is in the brain and the spinal fluid — and that has been a much more difficult thing to prove. There are some case reports that suggest in these patients, that virus may be directly in the nervous system. But a lot of these case reports have not been able to show that, suggesting that many of these effects may just be due to a systemic illness rather than to coronaviruses hiding in the brain and attacking it directly. But we don’t know the answer to that definitively. How many of these are actual viruses in the brain or virus in the nervous system? My guess is that it’s going to be a minority, but it’s not going to be unheard-of.
Video: How coronavirus affects the brain after being treated with a ventilator
For the latest coronavirus news and updates, follow along at https://news.yahoo.com/coronavirus. According to experts, people over 60 and those who are immunocompromised continue to be the most at risk. If you have questions, please reference the CDC’s and WHO’s resource guides.
How to maintain your physical and mental health during the pandemic
Taking care of a loved one with COVID-19? Here’s how to stay healthy
Q&A with Dr. Kavita Patel: How to keep your family safe and maintain your mental health
Read more from Yahoo Life
Sleep deprivation from nightly fireworks 'can be viewed as torture,' doctor says
What's the difference between a 2nd wave and 2nd peak of COVID-19?
Pregnant women with coronavirus: New study finds majority were ‘asymptomatic’
Want daily lifestyle and wellness news delivered to your inbox? Sign up here for Yahoo Life’s newsletter

