Steps to Getting an MS Diagnosis
Medically reviewed by Nicholas R. Metrus, MD
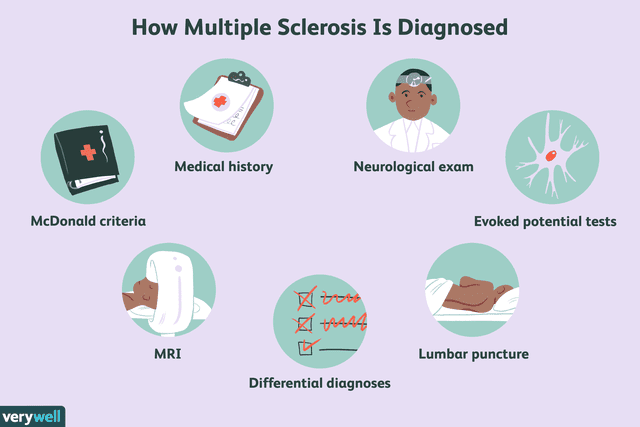
Diagnosing multiple sclerosis (MS) can be challenging because no blood or imaging test by itself can confirm that a person has the disease. Moreover, MS symptoms vary significantly among individuals and mimic symptoms of many other health conditions.
The good news is that after extensive revisions of the McDonald criteria (a formal set of MS diagnostic guidelines) and the emergence of sophisticated magnetic resonance imaging (MRI) techniques, multiple sclerosis can now be diagnosed more timely and accurately.
This article reviews the steps of getting an MS diagnosis, from seeing a neurologist to undergoing various tests like an MRI of the brain. It also discusses the typical age for an MS diagnosis and the risks of going undiagnosed.
Verywell / Emily Roberts
How to Get MS Diagnosed
A neurologist is a medical doctor specializing in brain, spinal cord, and nerve diseases, and they are responsible for diagnosing MS.
Neurologists perform a detailed medical history when evaluating someone for possible MS. They also ask about symptoms and collect data from various blood and imaging tests (and sometimes procedures) to determine if that person fulfills the McDonald criteria.
Information from this detailed evaluation also helps rule out alternative diagnoses.
Get a Neurologist Referral
If you are experiencing possible MS symptoms, seeing a neurologist is essential.
A primary care provider can often assist you with a neurology referral, or you can make the appointment on your own, depending on your insurance type.
The National MS Society—a prominent MS education and awareness organization—offers an easy-to-navigate tool for finding neurologists near you.
When choosing a neurologist, consider factors like traveling distance from your home or work, their approach to treatment (if diagnosed), and whether they are up-to-date on the latest MS research.
Learn More: How to Find a Neurologist for Multiple Sclerosis
Medical History
MS is a complex disease, so thoroughly investigating a person's medical history is essential.
During such an evaluation, a neurologist will inquire about the following:
Past and present symptoms, including time of onset and duration
History of any prior illness or current health conditions (e.g., viral infections, diabetes, or thyroid disease)
Family history of MS or other autoimmune diseases
Potential history of MS environmental exposures (e.g., obesity as a child/adolescent, smoking, or vitamin D deficiency)
Related: What Causes Multiple Sclerosis?
Record and Track Symptoms
The symptoms of MS are highly variable, often intermittent, and can be nonspecific, meaning similar to those found in other conditions. As such, before or between appointments with a neurologist, try writing down how you feel, whether in a notebook or on your phone or computer.
Recording symptoms can help you and your neurologist track potential patterns and triggers and, in the future, if diagnosed, determine whether MS treatments are working.
Common symptoms of MS include:
Sensory disturbances, like numbness and tingling of the face, trunk, arms, or legs.
Cognitive impairment (learning and memory problems)
Differential Diagnosis for MS
Although not an exhaustive list, health conditions that resemble MS include:
Neuromyelitis optica and acute disseminated encephalomyelitis (both neurological diseases)
Infectious diseases like Lyme disease and human immunodeficiency virus (HIV)
Other autoimmune diseases, namely lupus, Sjogren's syndrome, and sarcoidosis
Structural problems in the spine, such as a herniated disk
MS Diagnostic Criteria
The McDonald criteria are guidelines neurologists use to diagnose MS. With multiple revisions over the years, these guidelines have improved the accuracy and promptness of MS diagnosis.
According to the criteria, the essential step to diagnosing MS is uncovering evidence of damage in at least two parts of the central nervous system (consisting of the brain, spinal cord, and the eyes' optic nerves) occurring at different points over time.
Evidence for this premise, called dissemination in space and time, is primarily obtained from a person's medical history, neurological exam, and MRI of the brain and sometimes spinal cord.
What Is an MRI?
An MRI is a noninvasive imaging technology that produces three-dimensional (3D) images of the body's soft tissues using magnetic fields and radio waves. It's the most sensitive test for detecting MS-related damage in the central nervous system.
On the MRI, neurologists look for lesions (areas of damage or scarring), signifying that a person's immune system has malfunctioned and attacked the fatty (myelin) sheath surrounding nerve cells.
The damage—known as demyelination—is what causes the varying symptoms of MS (e.g., blurry vision, numbness, and muscle weakness, among many others).
MS lesions do not always cause symptoms. This is why, according to the revised 2017 McDonald criteria, the presence of any lesions, whether a person has symptoms or not, supports the principle of dissemination in space or time.
Also, in the revised criteria, under some circumstances, oligoclonal bands in a person's cerebrospinal fluid (CSF) can be used instead of dissemination in time to establish an MS diagnosis.
An example of this scenario would be if someone has MRI lesions in two or more brain regions but has only experienced one MS relapse (episode of new or worsening neurological symptoms).
What Are Oligoclonal Bands?
Oligoclonal bands are antibodies (proteins) released into the CSF during an MS attack. They indicate inflammation within the central nervous system and are present in more than 95% of people with MS.
Tests Used Besides MRI
Besides an MRI, other tests may help establish an MS diagnosis or rule out mimicking conditions.
Lumbar Puncture
As mentioned above, specific inflammatory proteins within a CSF sample may be used to confirm an MS diagnosis in some settings. The CSF is the fluid that bathes and protects your brain and spinal cord.
A CSF sample is obtained through a lumbar puncture (called a spinal tap), generally performed in the neurologist's office.
During the procedure, a person will lay on their side or sit on the edge of a bed, bent forward. The neurologist will then clean the lower back and inject a numbing medicine.
A needle will then be inserted between the vertebrae of their lower back to reach the spinal column, where a small amount of CSF will be removed using a syringe and eventually analyzed in a laboratory.
Evoked Potentials
Evoked potential tests measure how fast nerve signals reach the brain and how large or small a nerve response is when stimulated.
These tests are sensitive in detecting MS lesions because nerve signaling is slowed and less efficient when myelin is damaged.
Two types of evoked potentials sometimes used to help detect MS are:
Visual evoked potential (VEP) measures the speed of nerve signals between the eye and the brain.
Somatosensory evoked potential (SSEP) measures the speed of nerve signals between the skin (physical touch) and the brain.
Blood Tests
Blood tests can help assess a person's health and rule out differential diagnoses.
Examples of such tests include:
A complete blood count (CBC) to evaluate for anemia and infection
Vitamin B12 level to check for a deficiency
Blood tests for markers of inflammation, like C-reactive protein (CRP) or erythrocyte sedimentation rate (ESR or sed rate)
Thyroid-stimulating hormone (TSH) to assess thyroid function
Antinuclear antibodies (ANA) to check for autoimmune diseases, like lupus
Learn More: The Role of Blood Tests in Diagnosis MS
Typical Age of MS Diagnosis
Although MS can develop at any age, it's generally detected in young adulthood, between the ages of 20 and 40. Around 5% of cases are diagnosed at 50 or older (called late-onset MS),and 3% to 10% of MS cases occur before the age of 16.
Interestingly, for relapsing-remitting MS (RRMS), the median age of onset is 30 years. For primary progressive MS (PPMS), the median age of onset is 40 years.
RRMS Vs. PPMS
RRMS is the most common MS type, characterized by attacks (relapses) of new or worsening neurological symptoms followed by periods of symptom recovery (remission).
PPMS is the least common MS type, characterized by an accumulation of disability over time in the absence of relapses.
Learn More: Types of Multiple Sclerosis Overview
Risks of Undiagnosed MS
Unfortunately, due to the variable, subtle, and often intermittent symptoms of MS, a person may go undiagnosed for years. The risk of delaying an MS diagnosis is that it prevents the early initiation of a disease-modifying treatment (DMT).
Early Initiation of MS DMT
DMTs positively impact the long-term outlook of MS by decreasing the number and severity of MS relapses and slowing down the natural progression of the disease.
Moreover, in addition to a delayed diagnosis, an MS misdiagnosis is also relatively common. In one study, nearly 1 in 5 people were diagnosed with MS when they did not fulfill the current McDonald criteria. In such cases, alternative diagnoses were more likely.
Misdiagnosing someone with MS creates stress and carries a high physical and emotional burden. A person may take MS-related medications that bring on side effects and alter their lifestyle unnecessarily based on the diagnosis.
A misdiagnosis also means that the actual condition remains untreated, which can contribute to a worsening of the disease.
Related: Why Is Multiple Sclerosis Misdiagnosis So Common?
Summary
The diagnosis of MS is complex because there is no single test to confirm a person has the disease. Instead, neurologists use a formal set of guidelines called the McDonald Criteria to make the diagnosis.
The key principle of the McDonald criteria is that it provides evidence of damage to the central nervous system (CNS) at different times and to different parts—referred to as "dissemination in time and space."
To determine if a person fulfills the McDonald criteria, neurologists gather data from a person's medical history, neurological examination and magnetic resonance imaging (MRI) imaging of their brain and sometimes spinal cord.
Results from other tests, like a spinal tap and blood tests, are also used to establish MS and rule out differential diagnoses.
Read the original article on Verywell Health.

