What Are Sleep Disorders?
Medically reviewed by Valerie Cacho, MD
Sleep disorders, or conditions that cause difficulty getting healthy sleep, are relatively common. About 50 million Americans have some type of chronic sleep disorder, with insomnia and sleep apnea being the most common. Other conditions can also lead to disruptions in your sleep-wake cycle, including mental health conditions like depression or anxiety, medications, and chronic conditions or diseases affecting your physical health.
The symptoms of sleep disorders vary by type. Everyone is susceptible to difficulty getting good rest from time to time, but for some, the issue can become chronic and persistent. Treatments for sleep disorders depend on the severity and duration of the symptoms. Fortunately, there are therapies available for sleep disorders.
Design by Health
Types
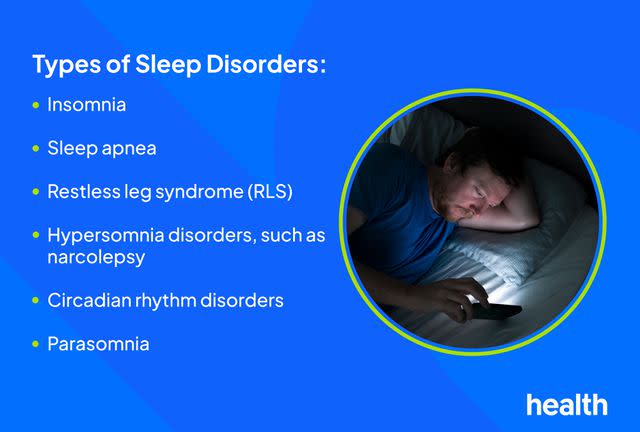
Researchers have identified over 80 types of sleep disorders. The most common types include:
Insomnia: This is the most common sleep disorder. It is characterized by difficulty falling or staying asleep.
Sleep apnea: This causes bouts of shallow or interrupted breathing while you sleep, often leading to snoring.
Restless legs syndrome (RLS): RLS causes tingling or prickling in your legs, often alongside a heavy urge to move them.
Hypersomnia: Hypersomnia is when you have trouble staying awake during the day. It includes conditions such as narcolepsy and Kleine-Levin syndrome.
Circadian rhythm disorders: Your circadian rhythm is your natural sleep-wake cycle. Problems with this cycle make it difficult to go to sleep or wake up at the times you need.
Parasomnia: This refers to unusual behaviors while falling asleep, sleeping, or waking up, such as walking, eating, or talking in your sleep.
Sleep Disorder Symptoms
The symptoms of sleep disorders depend on the specific type you have. Because they affect the quality and quantity of rest you’re getting—and because your body needs sleep—they also affect you during your waking hours.
Nighttime Symptoms
Each type of sleep disorder presents differently and has a unique set of signs. Common signs include:
Regular difficulty falling asleep (taking more than 30 minutes to do so)
Regularly waking up at night or too early without being able to fall back asleep
Snoring, gasping, or choking in your sleep or brief pauses in breathing
Creeping, tingling sensations in your legs that go away when you move them, often when trying to fall asleep
Jerking or moving your arms or legs in your sleep often
Very vivid dreams or dreamy sensations when drifting off to sleep
Sleepwalking or sleep-eating
Sleep paralysis, which is an inability to move just after waking up
Daytime Symptoms
Lack of sleep can significantly impact how you feel during the day, and some sleep disorders have specific effects throughout the day. The symptoms can include:
Excessive daytime sleepiness
Brain fog, causing symptoms such as difficulty concentrating, remembering, or staying focused
Irritability and crankiness
Suddenly falling asleep
Frequent napping
Sudden episodes of muscle weakness when angry, afraid, or laughing (cataplexy)
Feeling a lack of energy or motivation
Increased accidents, such as slips or falls
Causes
Your brain and body have a natural, 24-hour cycle of wake and sleep activity called the circadian rhythm. It’s what makes you tired when it’s time for bed or helps perk you up throughout your waking hours. Sleep disorders occur when this cycle is disrupted.
Many factors can influence this cycle, and sometimes the exact causes of sleep disorders are unknown. They can be symptoms of other health conditions, such as heart disease, lung disease, nerve pain (neuropathy), and obesity, among others. Also, sleep disorders may occur due to stress, traumatic events, medication side effects, mental health conditions (such as depression and anxiety) or genetic factors.
Risk Factors
Certain populations are more at risk of developing sleep disorders. Risk factors for this issue include:
Caffeine, alcohol, and/or substance use
Being assigned female at birth (for insomnia)
Being assigned male at birth (for sleep apnea)
Having an irregular sleep schedule due to work, school, or personal commitments
Working late or overnight shifts
Older age, as your ability to get restful sleep naturally declines as you get older
Using electronics often, especially close to bedtime
Having obesity
Insufficient exercise
Family history of a sleep disorder
Smoking
How Are Sleep Disorders Diagnosed?
If you’re presenting with sleep disorder symptoms, it's important to determine the underlying cause. Many conditions can affect your sleep, so your healthcare provider (likely a sleep specialist) may evaluate you for signs of post-traumatic stress disorder (PTSD), alcohol use disorder, depression, anxiety disorder, and chronic obstructive pulmonary disease (COPD).
Healthcare providers diagnose sleep disorders by evaluating your symptoms, medical history, and overall health. In addition, they may perform one or more of the following diagnostic tests:
Sleep diary: Your healthcare provider may ask you to keep track of how much sleep you’re getting, how easily you’re falling asleep, when you’re getting it, and how you’re feeling to assist with diagnosis.
Questionnaires: This involves using standardized scales, such as the Epworth Sleepiness Scale (ESS) or the Fatigue Severity Scale (FSS), you rate your symptoms to measure your level of sleepiness and drowsiness.
Sleep studies: Polysomnography (an inpatient sleep study) and home sleep apnea tests can be used to track breathing and brain activity while sleeping. You may also wear devices to measure your heart rate, physical activity, blood pressure, and other important clinical indicators.
Laboratory testing: To detect diseases that may be causing your sleep concerns, your healthcare provider may orders tests to evaluate your arterial blood gases, thyroid function, levels of iron in the blood, as well as cerebrospinal fluid (CSF).
Actigraphy: This is a device you wear on your wrist while you sleep. It tracks your circadian cycles and brain activity to assist in diagnosing certain sleep disorders.
Multiple sleep latency testing (MSLT): MSLT, or a nap study, tracks your body’s level of sleepiness to diagnose narcolepsy or hypersomnia. Devices are used to measure the extent of your daytime sleepiness while you take multiple 20-minute naps in an eight to 10-hour period.
Treatments
The specific approach to treating a sleep disorder depends on the type you have as well as the severity of your symptoms. Therapies range from taking medications to therapies focused on improving the quality of the sleep you’re getting.
Cognitive Behavioral Therapy
Cognitive behavioral therapy for insomnia (CBT-I) is a set of talk-based therapies that try to promote relaxation and change your behaviors surrounding sleep. CBT-I is performed under the direction psychologists, mental health counselors, or therapists. Strategies include:
Relaxation therapy: Focusing on meditation and other techniques to help you get to sleep
Sleep restriction therapy: Limits awake time spent in bed to make you drowsier at bedtime
Stimulus control therapy: Not reading or using of devices or watching TV in bed
Sleep hygiene therapy: You focus on improving sleeping habits through lifestyle changes
Breathing Devices
You can treat sleep apnea by wearing breathing devices, such as the continuous positive airway pressure (CPAP) device. A CPAP increases pressure in your upper air passages, ensuring your breathing remains consistent and you stop snoring.
In addition, wearing oral appliances (such as mandibular advancement device, or MAD) can change the position of your jaw or tongue to prevent symptoms. A MAD helps position your jaw and tongue in a way that helps you breathe while you sleep.
Medications
Medications for sleep disorders work either to promote sleepiness when it’s time for bed, or to take in the morning to prevent daytime drowsiness. Depending on your sleep disorder and its severity, your healthcare providers may prescribe any of the following:
Benzodiazepines, such as Restoril (temazepam)
Non-benzodiazepine hypnotics like Ambien (zolpidem) and Sonata (zaleplon)
Melatonin receptor agonists, such as Rozerem (ramelteon)
Orexin receptor antagonists like Dayvigo (lemborexant)
Histamine-3 (H3) receptor antagonists like Wakix (pitolisant)
Certain supplements, such as melatonin, may help though evidence is mixed
Prevention
Not all sleep disorders can be prevented, but healthy sleep practices can be helpful in managing your sleep and reducing symptoms of any sleep disorders you have. These strategies include:
Aiming for 7 to 9 hours of sleep a night, if you’re an adult
If you're struggling to fall asleep, get up, walk around for a little while, and try again
Managing stress, meditating, stretching, or other means of relaxing
Establishing set times to go to bed and wake up
Avoiding substance, nicotine, or alcohol use
Creating a comfortable, cozy low-lit bedroom environment
Boosting physical activity levels
Creating relaxing rituals before bed
Keeping your bed a screen- and work-free zone
Avoiding strenuous activity or heavy meals for at least four hours before going to bed
Related Conditions
Chronic sleep disorders can have a significant impact on your health and immune function, raising your risk for several conditions, including:
Asthma: Chronic insomnia can lead to or worsen asthma symptoms like wheezing and difficulty breathing, which also disrupt sleep.
Heart conditions: Heart failure, arrhythmia (irregular heartbeat), high blood pressure, and coronary heart disease often accompany chronic insomnia due to unhealthy habits caused by poor sleep, such as lack of physical activity, poor diet, and others.
Mental health conditions: Chronic sleep disorders can impact your mood, leading to depression, suicidal thoughts and anxiety. Conversely, conditions such as depression and anxiety can also disrupt sleep.
Pregnancy complications: Insomnia and sleep apnea raise the risk of increased pain during delivery, low birthweight, pre-term birth, preeclampsia (high blood pressure) and other complications. In a 2016 study, fewer than six hours of sleep a night increased the chances of caesarean section by 4.5 times.
Cognitive effects: Chronic insomnia can have a lasting impact on your ability to concentrate, remember, or perform other mental tasks.
Weakened immunity: Chronic lack of sleep also weakens your immune function, causing inflammation; this raises your risk of infection and disease.
Metabolic diseases: Sleep disorders impact hormones that regulate your metabolism, affecting hunger and how you break down food; this raises the risk of diabetes and metabolic syndrome, among other conditions.
Living With Sleep Disorders
While everyone can have sleep difficulties from time to time, chronic and difficult to treat cases can significantly impact your quality of life and overall health. Insufficient sleep leads to increased accidents and worsens your overall health. Studies found getting an average of less than seven or more than nine hours of sleep a night increases the risk of all-cause mortality (overall risk of death) by 33%.
Life with a sleep disorder very much depends on the type of disorder you have. With dedicated treatment of any underlying causes, therapies, lifestyle changes, and other approaches, many are able to manage their condition. As research continues, novel treatments and newer medications will continue to emerge.
Frequently Asked Questions
Is it normal to sleep 12 hours a day and still be tired?
Sleeping 12 hours a day and still feeling tired often or daily isn’t normal and calls for medical attention. Regularly or always sleeping well over the recommended 7 to 9 hours of sleep a night (for adults), may be a sign of hypersomnia, a sleep disorder, along with excessive drowsiness or napping sleepiness during your waking hours.
Can anxiety cause a sleep disorder?
Sleeping problems and mental health conditions are closely linked. Along with depression, anxiety disorder is among the mental health conditions that causes disturbed sleep as a symptom. Most commonly, anxiety causes insomnia: difficulty falling or staying asleep, restlessness at night, and waking up feeling tired.
Are nightmares a type of sleep disorder?
The occasional frightening or disturbing dream isn’t a sign of a sleep disorder, but frequent nightmares could be. Parasomnia—also called nightmare disorder—occurs when vivid nightmares regularly interrupt your sleep. This can significantly impact your mental, physical, and emotional health, as well as relationships at home and work.
For more Health.com news, make sure to sign up for our newsletter!
Read the original article on Health.com.

