Running Back From Hell

Normally, James Buzzell avoids crowds.
Being surrounded by strangers makes the former turret gunner anxious: Where did they come from? What are they up to? How the hell do I get out of here? He does not like being in situations where he can’t control the variables, because he knows if you don’t pay attention to 100 percent of the variables 100 percent of the time, people die. But there he was, at the starting line of the Rock ’n’ Roll Mardi Gras Half Marathon in New Orleans with more than 5,000 other people, not worried about something awful happening. In fact, he was laughing. Joking around with the guys he was going to run with, guys on his team. If you’d asked him then, he would’ve been hard-pressed to find words for the sense of peace he felt.
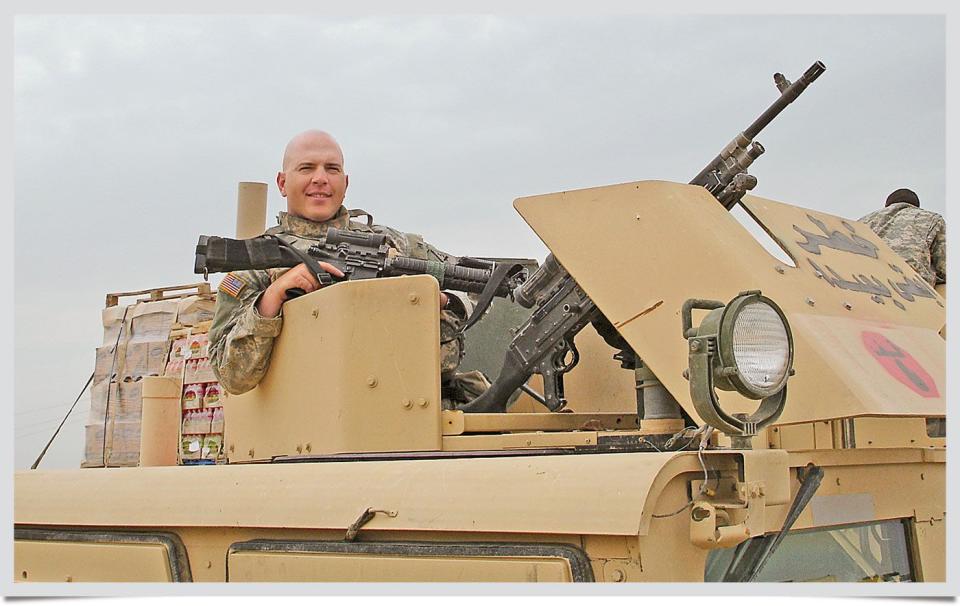

During most of his eight years in the Army’s Airborne Infantry, Buzzell, now 36, had plenty of stiffness and pain thanks to blunt-force trauma from a couple IED blasts in Iraq. But he ran 10-plus miles and did PT with guys in his squad at Fort Polk, Louisiana, every day, and when his shoulder or his ankle or his knee or his neck started really hurting, he took it easy, took some aspirin, and soaked in some Epsom salts. No big deal. Until his 1st sergeant saw his right hand involuntarily ball up into a claw, which it did sometimes because of nerve damage in his shoulder.
The Army restricted his exercise, and he started to gain weight. As he lost muscle, stuff started hurting more, and doctors prescribed meds for the pain. Inactivity combined with a 35-pound weight gain left him depressed and anxious, and they gave him meds for that, too. Ask his wife-that’s when the irritation and the impatience and the distrust and the anger snowballed and cost him nearly every friend he’d ever had. Doctors tried to reconstruct an ankle they could hardly believe he could walk on, let alone run on. In May 2012, he was diagnosed with PTSD, and two months later, he was medically discharged from the Army, from his career, from his life.
He slipped down a hole. Unable to work or tolerate restaurants or movie theaters, Buzzell rarely left his house in Columbia, South Carolina. His brain coursing with survivor’s guilt and memories of things he did and friends he lost, he drank a pint of vodka almost every day before bed. Doctors kept telling him to relax and prescribed him more meds, but drugs weren’t what he wanted. He just needed a better way to deal.
So when a physical therapist suggested he regain fitness after his surgery, he bought a pair of running shoes. And he couldn’t believe what he felt in those first runs in the woods. Peace. It just shoved all the anger and despair to the side and took him over. In time, he noticed that within the first mile, his anxiety fades. His rage evaporates. And he knows it sounds crazy, but the chronic pain in his shoulder and his ankle and his knee and his neck goes away, too. The sense of calm can linger for days, if things with his wife and baby are okay, and while the pain often comes roaring back the minute he stops, sometimes it takes a couple hours. He told his doctor that if he could run 16 hours a day and sleep for eight, he would.
But it was connecting with other runners that finally pulled him out of that hole. Don’t take it the wrong way, he says, but there’s an intimacy he has with his buddies from Iraq, a camaraderie that makes a lot of his PTSD symptoms go away. He found a similar reprieve when he joined Team Red, White & Blue, an organization that helps soldiers transition into civilian life, in part by connecting them to their communities through athletic groups and races. Now he’s part of a team again, and the soldiers and civilians he runs with don’t judge him. But they don’t let him wallow, either. They’ll tell him to shut up, stop feeling sorry for himself. And he listens, because he trusts them. And because he trusts them, he can stand at the starting line of a big race in a major city and instead of feeling like someone might die, he feels happy.
Since 2001, nearly 2.5 million U.S. military personnel have deployed to Iraq and Afghanistan. One in six of these men and women return home with post-traumatic stress disorder, which denies them peace, erodes their relationships, and erases joy from their lives. Countless more come back with post-traumatic stress, a term that applies to those who test below a diagnostic threshold but who have enough symptoms of PTSD that their lives are degraded or impaired.
Yet, while PTSD is the most common mental-health diagnosis among veterans of the wars in Iraq and Afghanistan, fewer than half of those affected seek help-many are halted by the stigma of being “broken.” Those who do get help can find relief: Several cognitive behavioral therapy treatments can essentially “cure” PTSD. But of those vets who seek treatment, 20 to 40 percent drop out. They do so for lots of reasons: difficulty accessing care, discomfort with mental-health professionals who don’t understand a soldier’s job, disillusionment.
Our veterans need an alternative. And one is starting to emerge.
For years, studies have found that exercise improves mood and is beneficial to those with depression, anxiety, and chronic pain. Now, based on this body of evidence, a few experts are researching how exercise might help those with PTSD. At the same time, soldiers are discovering on their own that physical activity eases their symptoms. And groups like Team Red, White & Blue are increasingly bringing those veterans together to instill a vital sense of mission to their recovery.
There’s long been a gap in exercise research as it relates to PTSD, but at two research facilities in Texas, an effort is under way to tap all the supporting evidence, to measure what guys like James Buzzell feel, and to answer a potent, provocative question: Can running help soldiers heal?
Mark Powers, Ph.D., believes the answer may well be yes. He’s a research associate professor at the Institute for Mental Health Research at the University of Texas at Austin, but up until July, he was codirector of the Anxiety Research and Treatment Program at Southern Methodist University in Dallas. There, he led a 12-week pilot study.
Powers, 42, with spiked black hair and the thick arms and stocky frame of a bodybuilder, wanted to examine the effect of exercise on PTSD symptoms. Specifically, he wanted to know if patients who ran moderately hard on a treadmill for 30 minutes prior to therapy reported a greater reduction in symptoms compared with those who underwent therapy alone.
The therapy employed in Powers’s study was prolonged exposure therapy, or PE. In it, a person repeatedly recalls his memory of a traumatic event for about 45 minutes, while he’s being recorded. The therapist then asks questions that help him process the memory-to fill in gaps and provide context around the images in his head. So, for example, an Army medic who blames himself for not saving his wounded buddy learns to incorporate details like their remote location, the extent of his friend’s injuries, and the prognosis for such injuries. Fleshing out his memory makes it clearer, and as he develops a better understanding of what actually happened, his guilt and sense of responsibility subside. He’ll spend time in highly stressful environments-say, the trauma ward of a hospital-and listen to the recording daily between therapy sessions.
Recovery comes from not only clarifying the memory, but being able to talk about it without falling apart. A memory can be so visceral that talking about it can prompt an uncontrollable fight-or-flight response. So the medic’s heart might race, his hands might get sweaty. He might get sick to his stomach, or cry. He knows he’s in an office in the suburbs, but his body responds to the memory like he’s in the firefight. That response is terrifying, overwhelming, maddening. It’s so intense that it can feel like he’s going crazy-or about to die. So his therapist asks him one crucial question: Has anything bad happened to you as you’ve been talking?
“Remembering a trauma is not threatening-the trauma was, but remembering it is not,” says Powers. “But we’re programmed such that, when something really bad happens, the brain says, Don’t unlearn this too easily. So it takes a lot more effort to unlearn something than to learn it-you can be in combat once and have the experience override everything else. We do the exposure, then draw attention to the fact that they’re safe-and that’s what we want them to remember.”
Essentially, Powers wants that Army medic to leave the session remembering that when he talked about ammunition cooking off from the burning Humvee, and the trees exploding from the force of 40mm grenades, and his buddy extinguishing the flames that had melted the skin from his face, none of it was actually happening. He didn’t need to react, he didn’t need to run. The quicker he makes the connection that he feels safe when he talks about his trauma, the more muted his physiological reaction becomes, and the faster he’ll recover.
And that’s where running comes in. Powers believes running might speed up that connection by boosting levels of a brain protein called brain-derived neurotrophic factor, or BDNF.
The protein helps the brain adapt to stressors and repair itself, and it’s low in most people with depression and anxiety-and particularly in those with PTSD. It’s also involved with learning and memory: Essentially, more BDNF is associated with a larger hippocampus. And when you have to learn and remember stuff, bigger is better. That’s because the hippocampus is a part of the brain responsible for contextual memory. According to Powers, brain scans have shown that like BDNF levels, hippocampal volume is low in people with PTSD. Which may explain why their contextual memory is off and every big bang is a bomb. Their brains aren’t differentiating between being at a cookout on the Fourth of July with fireworks going off and being in a convoy in Iraq that hit an IED.
“There’s evidence [primarily from animal studies] that when you exercise, BDNF goes up and hippocampal volume goes up, too,” says Powers. By cranking up BDNF, running could help someone with PTSD extinguish his fear and re-establish a sense of safety around feared cues.
Powers’s colleague at SMU was Jasper Smits, Ph.D., coauthor of Exercise for Mood and Anxiety. Formerly the codirector of SMU’s Anxiety Research and Treatment Program, Smits is now a professor at UT Austin along with Powers. “There are drugs that optimize learning, called cognitive enhancers, that act on receptors involved in extinction learning,” says Smits. “We think exercise is similar to those enhancers. Previous studies [in patients with panic disorder] have shown that exercise raises BDNF, and thereby gets a person’s brain systems ready to consolidate that safety learning. Patients walk away from the therapy session thinking, Oh, I’m okay. I’m safe.”
Before and after the 12-week study, Powers’s team took blood samples from nine participants (all civilians) to measure BDNF levels, and evaluators blinded to which group the person was in-therapy-only or exercise-plus-therapy-recorded participants’ PTSD symptoms.
The results were surprising.
The group that ran showed an increase in BDNF, while levels of those in the therapy-only group stayed flat. Everyone got better with treatment, but compared with the nonexercisers, the runners had a steeper decline in symptoms.
“We’re trying to remain skeptical, but it’s exciting given that we had so few people and still saw an impact,” says Powers. “It’s often difficult to find any difference with that small a number. We’ll write this up and apply for a grant to look at it with more people.”
It’s unlikely James Buzzell knew anything about BDNF or safety learning when he started running. All he knew was that it made him feel better and filled a hole in his life. That’s not surprising, according to both Powers and Smits. “There’s a lot of evidence showing that exercise can improve mood,” says Smits, “but a lot of that initial work wasn’t done with people with PTSD.” It was done on those with depression.
“Depression co-occurs strongly with PTSD, and even if you don’t have full-blown depression, PTSD brings with it mood disruption,” says Michael Otto, Ph.D., a professor of psychology at Boston University and Smits’s Exercise for Mood and Anxiety coauthor. “And exercise brings about a mood change almost immediately-within five to 10 minutes after exercising, people notice, ‘Wow, I really do feel better.’
“The boost comes after 30 to 40 minutes of moderate exercise,” Otto continues. “In fact, pushing hard can delay the boost because the exertion initially feels bad. So when you’re exercising for mood, you’re targeting a moderate level of exercise. The other good news is that the gains come so fast.”
Meaning that, unlike exercising for weight loss or a PR, the payoff is instant: You feel better now. What’s behind the boost? Perhaps changes in BDNF levels or in brain chemicals linked to mood and anxiety. Or perhaps it comes from doing something enjoyable, productive, and rewarding-finishing your first 5K, maybe.
Indeed, the power behind renewing a sense of accomplishment, pride, and esteem cannot be understated-especially for soldiers who have left the military. For some, leaving their team, the discipline, the sense of purpose and meaning and service to the greater good, is profoundly disorienting and can exacerbate symptoms of post-traumatic stress.
Exercise could replace some of what these soldiers lose. A running group could become a new team. A training program could provide structure. A race could instill purpose. Accomplishments could be 5Ks, then marathons, then 50-milers. And when a soldier dedicates himself to running for kids or cancer or wounded vets, he fulfills his mission of serving the greater good. “For the returning veteran, a number of things are important,” says Otto. “One is the mood boost. Second is this return to achievement-veterans leave structured, important lives for a much vaguer life, and sports training gives you structure. And then there’s this social integration-you get to join a team. It’s a one-two-three punch of getting the mood boost, training support, and social integration.”
Indeed, the potential impact of exercise on those with PTSD is wide-ranging. “It works for so many different things,” says Smits. “It works for physical health problems. For depression, the effect is robust, and for anxiety, there are more and more studies. With a few exceptions, it’s amazing the effects we’re seeing. Exercise might be a good alternative for people who say, ‘I don’t like medications,’ or, ‘I don’t like psychotherapy.’ And then for some people-what we’re studying-exercise can be used as a complement to things. Physicians already prescribe exercise, so now they could also prescribe it for mental-health problems.”
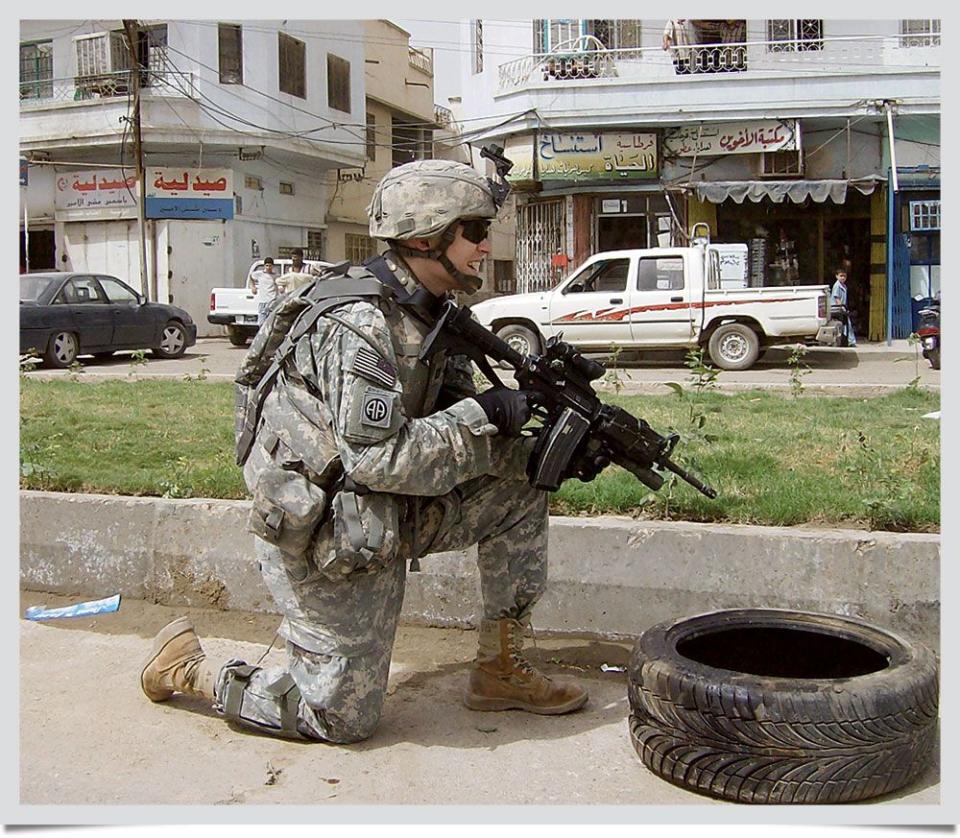

Joe Miller, 32, started having flashbacks and nightmares after his first deployment to Iraq. The grief and anger began during his second tour, when he was forced to abandon a mortally wounded but conscious Iraqi man after a suicide bombing. When Miller stopped sleeping during his third deployment, during the surge, the infantry platoon leader started to run. He ran as much as he could, to entice sleep, stave off depression, lead his guys, do his job.
Miller left the Army in the summer of 2008, and had his first panic attack during a run that fall. He dropped to the ground, winded and vomiting. It felt like he was going to die. But I’m not sick. Soon after, he started counseling for PTSD and made some connections: When his heart rate jacked above a certain point, the attack would come. The worst violence he’d experienced in Iraq came in urban areas in winter, so if it was cold out and there were a lot of cars around and his heart rate soared, the attack would come.
He ran sporadically for a while until two years later, when he signed up for his first trail race. Actually back-to-back races, a 10K followed by a 25K. It was overkill, of course, and he suffered mightily, but it reminded him of something: the sublime blend of strength and weakness, of moving like a broken man through the woods yet feeling utterly at peace-it had been like that at Army Ranger School. He returned increasingly to the trails, because the simplicity of putting one foot very carefully in front of the other could diffuse the anger and frustration he found hard to control.
Running also tuned him in to his body. It made him sensitive to paces that would spawn a panic attack (5K and 10K) and those that mostly didn’t (half marathon and longer). It helped him manage those attacks and push back the point at which they flared (in December, he ran his second ever sub-20-minute 5K). Running drove away-a bit-the fear of the future that haunts those with PTSD, and it gave him a measure of hope. Most of all, it gave him back the best parts of himself. In its boundless cruelty, PTSD smothers self-esteem with shame. But running ultramarathons mimicked what Miller had been good at in the military-he had loved the methodical preparation and planning for a mission. Running 50-milers requires the same complex understanding of what might go wrong and how to deal with fallout. He’d thrived on the adrenaline of being in the Army, and his whole life he’d always chosen the harder path-the infantry, the Rangers. Very few people have the balls or the brains to run 50 miles, and even when he has bad races, he takes solace in knowing he is again part of an elite group. When his mood darkens, he can look at his legs and know he’s got the strength to rise to a challenge very few could accept. He is still a badass.
It’s so windy in San Antonio that traffic lights are blown nearly horizontal and birds coasting on the currents look like they’re about to capsize. But walls of rock protect the maze of trails tucked beneath scraggly branches of live oak and cedar trees. Alan Peterson, Ph.D., runs easily over the loose stone and polished bumps of limestone. He is trim, with green eyes, short graying hair, and deep lines around his mouth. He isn’t feeling great; he’s had a sore throat for days, and he’s got family matters on his mind. The federal government sequester is set to go into effect in five days, and he’s worried that a forced restructuring of the military will perpetuate the stigma around PTSD-with the proposed elimination of 80,000 active-duty soldiers from the Army, “they’ll be looking for anyone with a hangnail, any blemish,” he says, as a reason for discharge. He’s running with all that on his mind because it’s what he does, what he needs. It’s his therapy.
Peterson, 56, is a retired Air Force colonel who spent most of his military career as a clinical health psychologist. After 9/11, he deployed twice to the Middle East-the second time at Balad Air Base in Iraq during the Battle for Fallujah. November 2004 remains the most deadly month for U.S. troops in Iraq since 9/11, and at the time, the U.S. Air Force field hospital in Balad was likely the busiest trauma center in the world, with patients coming in 24/7-amputees, burn victims, serious head injuries. It was there that he started using prolonged exposure therapy to treat soldiers who had witnessed too much devastation-piles of severed limbs, eviscerated remains, maimed Iraqi kids-and had developed PTSD. His wasn’t the standard practice in theater at the time. Back then the perception was that talking about traumatic events made things worse; just give the guy a little counseling, “three hots and a cot,” and get him back on duty.
But Peterson’s methods worked. After a few sessions, he was able to get guys into remission, back to their units, and back into the fight. Balad was also where he started to run. Peterson signed up for the virtual Balad to Baghdad run-mostly to get the T-shirt-tracking his miles on a treadmill. After that, he did a shadow run of the Army Ten-Miler with a colleague, one of the few times he was able to be outside without 35 pounds of body armor. It was his longest run ever.
In 2006, after 21 years of active duty, Peterson retired to become a professor and chief of the Division of Behavioral Medicine at the University of Texas Health Science Center at San Antonio. That same colleague he ran with in Iraq started bugging him about running a marathon. Peterson, citing bad knees and little faith, said no: It’s not healthy to run those distances. But the guy kept after him, and eventually, Peterson relented. That November he ran his first marathon-and within four months, ran four more.
“At first, I liked running because it got me into a routine and gave me a chance to think,” he says. “Eventually, I realized this is my therapy, my time to make sense out of life.” Running helped him process the trauma of more than 150 mortar and rocket attacks and exposure to seriously injured troops during his deployment. He could take his stress and frustration and anger, and just dump it out over the miles. When he finished, he felt better, more resilient. He favored trails over roads for both scenery and surface, and in April 2007, he ran his first 50K on the dirt. He’s since run more than 50 marathons and ultras, including four 100-milers.
In 2008, after Congress reviewed reports detailing skyrocketing rates of PTSD in troops returning from Iraq and Afghanistan, the Department of Defense granted Peterson $35 million to establish a research consortium on PTSD-the first of its kind to study PTSD in active-duty military. It was on a run that he convinced himself he could effectively manage 14 research projects and more than 200 people, including some of the top researchers in the world. It was also where he came up with the consortium’s name: STRONG STAR (South Texas Research Organizational Network Guiding Studies on Trauma and Resilience).
As he falls into the rhythm of the run, Peterson is clearing his throat less and opening up more. He runs past a small herd of deer tucked out of the wind beneath the cedars and explains STRONG STAR’S goal. It’s simple: intervene early to get service members with PTSD into remission so they can do their jobs and live happy, productive lives. With one study in particular, Peterson believes running may help soldiers recover from traumatic stress exposure and build resiliency, just like it did for him. If he’s right, the implications could be huge. For those with post-traumatic stress, their recovery just might be a training plan away.
At 342 square miles and supporting a population of about 350,000, Fort Hood near Killeen, Texas, is one of the largest military installations in the world. Since 9/11, more soldiers from this post have been deployed, wounded, and killed than from any other in the Department of Defense. For post-traumatic stress, “it’s ground zero,” says Peterson.
Rough Rider Village in Fort Hood is a short drive from the vast field where troops do morning PT. Its sand-colored trailers once housed service members; this past fall, it became the site of a STRONG STAR study that will examine whether running enhances treatment for post-traumatic stress. Five times over eight weeks, soldiers in both the therapy-only and the exercise-plus-therapy arm of the study will enter unit #3560, cross a kitchen area, and enter an office. While a white-noise machine hums outside the door and an audio recorder captures it all, they will recall the agony of what they saw, heard, smelled, and felt. They will leave with the assignment to listen to the recording every day. But what sets the STRONG STAR study apart from the Dallas study is that five days a week, the exercise group will run the streets and paths and treadmills of Fort Hood with the horror playing over their headphones.
Peterson designed the study with Stacey Young-McCaughan, R.N., Ph.D., 57, an Army nurse for 29 years who retired a colonel in 2008. She has green eyes, short gray hair, and an inquisitive manner, having spent much of her career as a cancer nurse and exercise researcher. She’s lead researcher of the exercise study.
Most people who experience a traumatic event-a car accident, say, or an IED explosion-do not experience lasting effects. For a while, they may flinch at the sight of an oncoming car or jump at a loud noise. That response is normal; it’s the body’s way of protecting you, of saying, Hey, pay attention here. The world is a little unsafe right now.
Eventually, the more you drive and the more you’re exposed to the racket of day-to-day life, that heightened sense of awareness naturally diminishes. New memories-of mundane, crash-free trips on the highway, for example-get laid down over the traumatic one. Your brain recognizes that maintaining anxiety or fear is no longer useful because sustaining such emotions is no longer a matter of life and death. Physiologically, your body quiets down, clearing out the stress hormones keeping you on high alert. With time, you respond to traffic and fireworks the same way you did before the crash or the explosion.
But sometimes, a traumatic event and its emotional and physical aftermath are so devastating that they override the body’s ability to recover and move on. For a soldier, it might be a single event like an ambush that killed his best friend, but it’s often an accumulation of horrors: weeks, months-sometimes years-of navigating a world full of mortars, rockets, bombs, and very bad guys. While he’s downrange, his body adapts to the idea that the world is an extremely dangerous place, and the only way to survive is to stay on guard and avoid places where bad things happen. So his body churns out stress hormones that keep him relentlessly on edge. And when he comes home, it’s difficult to turn those adaptations, those survival skills, off. He stays on edge, and the skills that kept him and his buddies alive in Iraq or Afghanistan are suddenly very much out of place. Patrolling his home’s perimeter, avoiding crowds or stairwells or parked cars, jumping at the dog barking-those skills become problems. He can’t turn the alert down.
But the most terrifying, overwhelming, maddening thing of all is that if he’s suddenly in a crowd or has to drive in a congested city center or talk about certain things, his body unleashes a barrage of fight-or-flight sensations so powerful it can feel like he’s about to die. It makes no sense to him to feel mortal danger when he enters the grocery store or drives his kid to school or tries to answer a question about a patrol last February, but those sensations-and his lack of control over them-are so awful, he quits doing whatever the hell triggers them. Quits going out, driving, or talking much. And when that happens, the disorder has taken him captive. Because the only way to overcome profound distress is to confront it. Over and over and over again, until his brain and body accept that when he drives on the highway, talks about the patrol, or walks among parked cars, nothing bad happens. In a cruel twist, the disorder seeks to keep him safe-by diminishing his life and depriving him of joy.
And that is PTSD.
“The military’s job is not to do research; that’s what civilian institutions do,” says Peterson. “But they don’t know how to work with the military. A lot of our consortium members are retired military or prior service, so we’re hoping to bridge the gap between civilian experts and the troops that need care.”
Like Powers and Smits, Peterson and Young-McCaughan see a gaping hole in the research on the effect of exercise on those with PTSD, and believe that, based on research done in other areas, exercise could help. Unlike the civilian study in Dallas, the STRONG STAR study in Fort Hood will enroll soldiers with post-traumatic stress as opposed to full-blown PTSD. Since exercise is not yet a proven treatment for PTSD-studies like Powers’s have not yet reached the large, controlled trial stage-and because the Department of Defense has tasked STRONG STAR with expediting treatment, PTSD patients are directed to studies using therapy methods proven to effectively treat the disorder in civilians. Briefly, to be diagnosed with PTSD, you must exhibit for at least a month a certain type and number of symptoms that seriously disrupt daily life. But testing below a symptomatic threshold does not mean one’s suffering is any less real.
“Almost everyone who deploys to a combat zone is exposed to combat-related trauma-mortar attacks, rocket attacks, small-arms fire, exposure to human remains and severely injured individuals,” says Peterson. “About 40 to 50 percent of that group will have post-traumatic stress symptoms that impact their functioning, [even if] not to the point where it meets the clinical criteria for PTSD.”
Young-McCaughan adds, “People with PTS wall themselves off, thinking, Why do I need to go to Walmart? I’ll just order everything online. They know their spouse is unhappy because they don’t like to go out anymore, and they know they feel isolated, but they kind of deal with it. And people get surprised because, all of a sudden, they can’t go to a family wedding or to a playoff game. They’re surprised when it comes back to hit them in a really negative way. So, yeah, you could control the symptoms to some extent, and you could isolate yourself, but you could have your life back, too, and do all the things you used to enjoy doing.”
It’s a potentially huge population that lives this way. And an underserved one, says Peterson, because if you don’t have full-blown PTSD, there aren’t programs for you. “There’s also the stigma piece; people are often embarrassed to be labeled with PTSD,” he says. “I think PTS is more acceptable because almost everybody has it, and if there’s a program like running that can help with it, we think [soldiers] will be more receptive.”
As with Powers’s Dallas study, Peterson and Young-McCaughan are looking at a distinct effect exercise may have on those with post-traumatic stress: its effect on anxiety and stress resiliency-specifically, changes in levels of the stress hormone cortisol. They both (along with Powers and Smits) think running can help soldiers get used to those terrifying, overwhelming, maddening fight-or-flight sensations by mimicking them. Fear of benign bodily sensations is called anxiety sensitivity, or anxiety over anxiety, and it’s common in people who suffer PTSD. If a soldier is running, he’s going to feel some of the same physical sensations that occur whenever he steps inside a crowded stairwell, drives in traffic, or recalls the day his convoy was attacked. If he can start associating those sensations with a morning workout instead of an ambush, he’ll avoid them less and get over them faster.
Think about it: Exercise, especially running, mimics the sensations you feel when you’re afraid. It jacks up your heart rate, riles up your gut, makes you breathe hard and sweat a lot. It’s a major stressor. People with PTSD may avoid those feelings because they associate them, either consciously or unconsciously, with a traumatic memory. The dominant memory of a hammering heart and sick stomach is an IED explosion.
But if you run, you expect your heart to beat faster and your palms to sweat and your stomach to maybe feel like a bowl full of junk. And the more often you run, the more you expose yourself to those physical sensations, the thicker the layer of new memories becomes-the dominant memory associated with those sensations is no longer the fire-fight. It’s the interval workout you did that morning. That trauma memory is still there. It doesn’t go away, but it’s no longer the most salient, and it no longer triggers a response.
“With fight-or-flight reactions,” Peterson says, “there’s a significant physiological reaction, and vigorous exercise like running comes closest to what that reaction is like. The goal is not to get overwhelmed by the physiology and quit, but to channel the surge of adrenaline into running, cognitively process the traumatic events, and lay down new memories.”
Running might also fortify the soldiers against future stressors. Studies have shown that fit people generally respond better than unfit people to stress-they don’t have as intense a reaction; i.e., their heart rates don’t spike as high, and they return to a physiological baseline quicker. “Stress, in particular post-traumatic stress, can cause a big release of hormones that people react to differently,” says Young-McCaughan. “For some, these stress hormones don’t ever dissipate; they’re always on high alert. Other people have been on high alert so long, their bodies are just so exhausted, they can’t mount a stress response.
“Exercise helps retrain the body to respond to a stressor,” she says. “You’re asking the muscles, heart, and lungs to work hard, and when you stop, you want the body to recover back to normal functioning. To be like, ‘Oh, I recognize that stress. I know how to handle that.’ I think running helps metabolize stress hormones, and we could use it to help retrain the body-to relearn how to recognize stress, respond, and recover.”
To that end, before and after the eight-week study, she’ll collect saliva samples to measure levels of the stress hormone cortisol; soldiers will submit those samples from multiple points in time during a day in which they recall their trauma. The point is to see if, by study’s end, their bodies react less intensely and recover more quickly from the stress of talking about it. Those results will be considered along with a blind evaluation of the prevalence of PTSD symptoms.
But what’s unique about Peterson and Young-McCaughan’s study, and what could have implications for soldiers who want limited to zero time in structured therapy, is that running while listening to the trauma tape, or simply thinking about the experience, gives all that stress that comes with the memory a place to go. Our bodies are hardwired to respond to fight or flight, but if we’re just sitting around with no way to release that energy, that’s when stress starts attacking the body’s weakest links, and you end up with chronic health problems. If you could channel it into running, says Peterson, all that adrenaline has something to do besides contaminating your systems and beating up your organs. Running can exhaust all that stress. By the end of the run, a soldier might be able to think clearer, and go a little further in making sense of what happened.
But why running? Certainly other sports could have a similar effect. But running is cheap and easy to do and has few side effects. It’s familiar-an integral part of every soldier’s job. And there’s a rhythm to it that helps him focus on the scenes in his head.
And when a soldier turns to running for relief, stigma does not follow.


Research takes years. Studies like those at Southern Methodist University and STRONG STAR must first show that exercise enhances treatment. Then larger studies or randomized clinical trials will follow. Science is a long process of replicating results. But if something as simple as running can help defuse the horrors of PTSD, perhaps we don’t need to wait that long.
Peterson believes soldiers with full-blown PTSD will need therapy to fully recover but that exercise may help them get there faster. And for those warriors with “just” post-traumatic stress, those who live in a purgatory of getting by but barely, he has a plan. For them, he envisions a treatment program that exists outside hospital walls, outside a therapist’s office. He envisions a program that takes place outside-on the trails.
It will be a running program and it will have a name that taps the nature of the men and women it serves-something with the word “rogue”-and it will be hard, with goals that might seem impossible for a while. The soldier will get advice on training and instructions on navigating the pain, both psychological and physical. Then he’ll go out, and on terrain that might resemble a place where unspeakable things happened and brothers died, he’ll run. He’ll think about those things that happened and start to assemble the pictures in his head, and when some of those images send a bolt of adrenaline through his body, he might run faster. It will be awful, dredging up the guilt and the shame and the grief and the horror, and he’ll drive as much of it as he can into the ground. He will call Peterson after those first few runs, and they’ll talk for a few minutes to process, fill gaps, create context. He’ll keep running and remembering, day after day after day, and as he does, grainy images will get clearer. A story will emerge from the pictures, a detailed story with a beginning, middle, and end. And when he’s paged through it enough, his torment will subside. The grief and the pain will make room for joy. Triggers will lose power, and the sound of his heart beating will simply be the sound of a soldier running.
If the STRONG STAR study shows that running helps soldiers, Peterson will implement this plan. His team must first prove that it helps. But across the country, turret gunners, platoon leaders, and Special Forces guys are ahead of the experts, of the research, of the papers and the press releases.
They already know running helps.
Story Update · June 2, 2016
Shortly after this story ran, James Buzzell and his wife bought a small farm in Massachusetts, which Buzzell manages full-time with a little help from his “boss”-4-year-old daughter, Isabelle. Most days, he feels great. “I am perfectly content, living a happy, fulfilled life with my daughter as my alarm clock,” he wrote in an email to Runner’s World. He still runs, and plans to complete a 5K series this summer. Buzzell now equates running to meditation. “I can go to ‘that place’ whenever I want now because I have been there so many times through running.” Joe Miller is also doing well. He has a 5-month-old son, and is working on his Ph.D. dissertation about mental and physical resilience among soldiers in the War of 1812. He also teaches. “Making students understand PTSD, and the fact that soldiers miss combat, has been really valuable to me,” he wrote in an email. Despite a setback from a stress fracture, he too still runs, and was targeting a 50K over Memorial Day Weekend. “I have been visualizing carrying my son over the finish line, as my chief training motivation during an ugly and less than healthy training period,” he wrote. One study mentioned in the story has since wrapped up: Mark Powers, who is now at the University of Texas at Austin, and his team found that people who ran prior to therapy for PTSD had fewer symptoms at the study’s conclusion than those who did not. The STRONG STAR study is ongoing; researchers are roughly halfway to their goal of examining 120 Fort Hood service members. “People seeking treatment for PTSD often don’t like the choices they’re given,” writer Christine Fennessy says. “If something as simple as running might offer some relief, it’s worth researchers’ time and effort to better understand why and how. Veterans deserve good options.” –Nick Weldon
('You Might Also Like',)

