Rheumatoid Arthritis: From Beginning Symptoms to Treatment
Medically reviewed by Stella Bard, MD
Rheumatoid arthritis (RA) is one of the most common autoimmune arthritis types. It occurs when the immune system malfunctions and attacks healthy tissues—mainly the synovial linings of joints. RA is also a type of inflammatory arthritis.
Inflammation is a central characteristic of RA, leading to pain and swelling that affects the joints and other body tissues. Inflammation is how the body responds to defend itself from foreign invaders like bacteria and germs. In people with RA, the body's inflammatory response is overactive.
Left unchecked, RA inflammation can lead to severe joint damage, disability, and disease complications. There is no cure for RA, but the disease is treatable and manageable.
This article will cover rheumatoid arthritis symptoms, causes, treatment, and more.
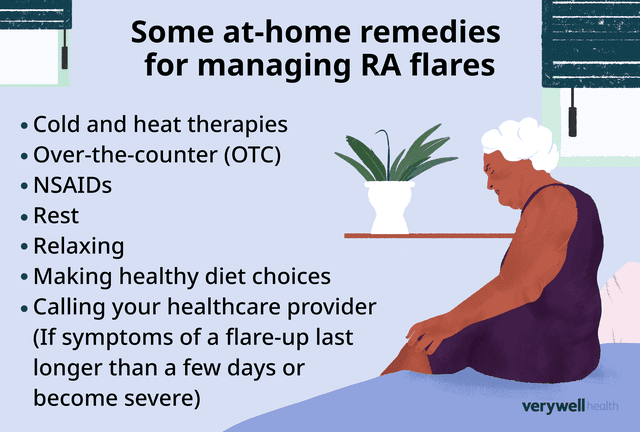
Illustration by Michela Buttignol for Verywell Health
Early Rheumatoid Arthritis (RA) Symptoms
Morning stiffness of the joints is one of the earliest signs of RA. This symptom may last an hour or longer. It occurs after long periods of inactivity and affects one or more joints. This type of stiffness improves with movement and as the joints warm up. Pain with movement and joint tenderness are additional early symptoms of RA.
Symptoms of RA will come on slowly and worsen over weeks and months. The number of joints involved in early RA varies, but RA is a polyarticular condition, which means five or more joints will be affected.
For many people, RA will start in the small joints of the hands and feet. Inflammation and swelling of these joints lasting six or more weeks might indicate inflammatory arthritis.
Inflammatory Arthritis
The term "inflammatory arthritis" refers to any arthritis type in which the body's immune system mistakenly attacks healthy tissues, causing inflammation that affects multiple joints and other body tissues. In addition to RA, psoriatic arthritis, Still's disease (systemic juvenile idiopathic arthritis), and lupus (systemic lupus erythematosus, SLE) are all types of inflammatory arthritis.
RA is a type of symmetric arthritis that affects the same joints on both sides of the body. For example, if the fingers of one hand are inflamed, the fingers of the other hand often will be as well. If one wrist is affected, the other wrist is also likely to be affected by RA.
Symmetric involvement of the small joints of the hands is expected in RA. As RA progresses, it is possible to experience inflammation in larger joints, including the knees and hips.
Related: Polyarthritis, Inflammatory Arthritis, and Rheumatoid Arthritis
How It Feels
Symptoms of RA will be systemic (whole-body) and symmetric. They may include:
Malaise (a general unwell feeling)
Fever
Pain and stiffness in more than one joint
Morning joint stiffness
Tenderness and swelling of affected joints.
Numbness and tingling
Decreased joint range of motion (full movement potential of a joint)
Weight loss and loss of appetite
Related: Early RA Symptoms and Signs
The pain associated with RA varies from person to person. Inflammation associated with the condition leads to pain, tenderness, and warmth in and around the affected joints.
RA pain has been described as deep and achy, as well as dull and persistent. It has also been described as sharp and shooting, especially with movement. Joint stiffness is typical, especially in the morning upon waking and after long periods of inactivity.
Some people with RA describe periods of excruciating pain, severe fatigue, and little or no energy. Pain can affect mobility, especially if the hips, knees, ankles, or feet are severely inflamed.
RA can also have cognitive and emotional effects. Cognitive features of RA include memory loss, brain fog, confusion, and trouble with thinking or reasoning. Emotional effects of RA include mood swings, depression, sadness, despair, and anxiety.
Disease Progression
RA is a progressive condition that will worsen over time. What that progression looks like will vary from person to person and depends on multiple factors.
Such factors include:
How advanced the disease was at the time of diagnosis
Age of the person at the time of diagnosis
Current disease activity
Presence of antibodies in the blood: Two types of antibodies are present and elevated in people with RA—rheumatoid factor (RF) and anti-citrullinated protein antibody (ACPA or anti-CCP). RF and ACPA are detectable in most people with RA and are known to cause increased disease activity.
RA progression is gradual and can take years or even decades. This progression is classified into stages.
These stages are:
Stage 1 or early-stage RA: In this initial stage, the immune system is activated, and inflammatory cells (i.e., macrophages, T cells, and B cells) invade the synovial tissues of the joints. The small joints of the hands and feet are often the first affected joints. Additional symptoms like joint pain and stiffness, fatigue, and fever, will be subtle in stage 1.
Stage 2 or moderate RA: RA will gradually worsen, and in this stage, the joints may start to experience damage from synovial thickening. There will be pain and the onset of limited range of motion. Inflammation may affect other body areas, especially the skin and eyes.
Stage 3 or severe stage RA: In this stage, there will be severe pain and swelling, muscle weakness, mobility problems, and bone and joint damage.
Stage 4 or end-stage RA: In stage 4, the joints no longer work, and there is severe pain and a loss of function or disability. Surgery is the only way to treat RA-damaged joints and improve mobility and function at this stage. Progression to stage 4 can take many years or decades, but thanks to treatment advances, most people with RA never make it to this stage.
Related: What Does Rheumatoid Arthritis Progression Look Like?
Whole-Body Effects
RA mainly affects the joints but can also affect other body systems. This is because RA leads to whole-body effects that can damage joints and organs and affect life span. Many of these are also considered disease complications.
Additional body areas RA can affect are:
Eyes: RA can affect the eyes and lead to dry eye and redness. It can also lead to more severe eye conditions like scleritis (inflammation of the white part of the eyes) and uveitis (inflammation of the middle layer of the eye). RA can also increase the risk for another autoimmune disease called Sjögren's syndrome, which affects the tear and salivary glands.
Mouth: RA can cause dry mouth, gum disease, gum infections, and dental problems.
Skin: Skin rash and ulcers of the arms and legs can occur in RA. Another skin manifestation of RA is rheumatoid nodules—lumps of inflammatory tissue just below the skin near a joint.
Heart and blood vessels: People with RA have a higher risk for heart disease because of high inflammation levels in their bodies. Inflammation can also affect the blood vessels, leading to narrowing and slower blood flow.
Anemia: Many people with RA will also experience anemia (low red blood cell counts) or lower hemoglobin levels.
Lung problems: Uncontrolled inflammation can cause interstitial lung disease (ILD)—scarring of lung tissue. This scarring makes it harder for oxygen in the lungs to enter the bloodstream and travel to other organs.
Kidney function: People with RA have a higher risk for chronic kidney disease, although the use of biologic drug therapies and decreased nonsteroidal anti-inflammatory drug (NSAID) use have brought these numbers down over the years. RA is also associated with amyloidosis, an abnormal protein buildup that impairs kidney function. Amyloidosis can affect any organ in the body, including the skin and heart.
RA on its own is usually not fatal. But complications like those above can shorten a person's life. Fortunately, newer, more aggressive treatments have reduced disease complications, which means people with RA are living longer.
Related: How Rheumatoid Arthritis Affects Different Body Systems
RA Causes, Risk Factors, and Triggers
RA is an autoimmune disease resulting from a malfunction in the immune system that causes it to attack healthy tissues.
The exact cause of RA is unknown, but researchers have identified specific genetic, environmental, lifestyle, and hormonal factors they believe are linked to its development. These risk factors may work alone or in combination to trigger the malfunctioning of the immune system.
Such risk factors include:
Genetics: A family history of RA increases your risk for the disease. But family history alone is not enough to trigger the disease, and getting RA without a family history is possible.
Environment: Certain aspects of your environment might increase your risk for RA. These include exposure to chemicals and pollutants, chronic stress, past physical or emotional trauma, an illness, or a viral or bacterial infection.
Lifestyle: Researchers believe that lifestyle risk factors can lead to the development of RA. This includes smoking, having obesity, and diet.
Hormones: Research shows RA affects people assigned female at birth more so than people assigned male at birth. Women are 3 times more likely to have RA. Because of this, researchers believe sex hormones contribute to disease development. About 50% of women with RA develop it during their reproductive years.
(Note that when research or health authorities are cited, the terms for sex and gender in the source are used.)
Related: Diagnosing and Treating Rheumatoid Arthritis in Men
Early RA Treatment
Treating rheumatoid arthritis focuses on controlling inflammation and pain, stopping joint damage, and preventing disability. That is achieved with medicines, therapies, lifestyle changes, and surgery to restore joint function and repair damaged joints.
Medications used alone or in combination to treat the condition include:
NSAIDs, such as Advil (ibuprofen) and Aleve (naproxen sodium) to reduce mild to moderate inflammation and pain
Corticosteroids for treating flares and short-term control of pain and inflammation
Traditional disease-modifying anti-rheumatic drugs (DMARDs) to slow down disease progression and save your joints from permanent damage
Biologic DMARDs when traditional DMARDs don't help. These drugs are potent and affect inflammatory proteins called cytokines.
Janus kinase (JAK) inhibitors to tamp down the immune system, ease inflammation, and prevent joint damage
If you are recently diagnosed with RA, your healthcare provider will typically start you out on a traditional DMARD, which is usually methotrexate, unless there is a reason you can't use it.
You will continue the initial treatment for at least six months. A biologic DMARD might be added if there is little or no improvement or symptoms have worsened.
Long-Term RA Treatment and Managing Flares
You will need to treat RA for the rest of your life. This includes regular medical visits with a rheumatologist and tests to assess how well treatments are working and to monitor medication side effects. Long-term treatment for RA is crucial in controlling inflammation and minimizing joint damage.
What Is a Rheumatologist?
A rheumatologist is a medical doctor (M.D.) who specializes in diseases that affect the bones, joints, and muscles. A rheumatologist can confirm an RA diagnosis and provide a treatment plan.
In addition to medication, your rheumatologist will recommend non-drug therapies to help you manage pain and symptoms.
For example, physical therapy can help keep joints strong and mobile. Research on physical therapy for managing RA finds it to help manage RA pain and stiffness, improve movement, restore function, and prevent disability.
An occupational therapist might suggest ways to protect your joints while doing daily tasks. They can also recommend assistive devices that help avoid stress on your joints.
If you experience RA joint damage, your healthcare provider might recommend surgery to repair or replace damaged joints. Surgery can reduce pain and improve joint function.
Managing RA Flares
People with RA will experience periods where their disease flares up. These are times when their symptoms are worse. Symptoms experienced during a flare include severe joint pain, swelling, stiffness, and fatigue.
Specific events, including stress, diet changes, illness or infection, weather changes, overexertion, missing medication doses, and smoking (including secondhand smoke), may trigger flares. You might be able to reduce the frequency of flares by avoiding such triggers.
Most people can manage flares at home with rest and home remedies. Some at-home remedies for managing flares include:
Cold and heat therapies: You can relieve pain using ice packs on inflamed joints. Dry or moist heat can help relieve sore muscles. Dry heat options include heating pads and hot water bottles; moist heat includes hot showers and baths.
Over-the-counter (OTC) NSAIDs: If RA pain and swelling are severe, consider an OTC pain reliever like Advil to bring down inflammation and reduce pain. OTC topical pain relievers, such as Voltaren (diclofenac), can also help with pain and inflammation. A plus with topical pain relievers is they cause fewer side effects.
Rest: Rest is key to managing a flare. If you need extra sleep or rest, make that time. You will still want to include some light activity as you recover. But you want to avoid pushing yourself to avoid injury or increase inflammation.
Relax: Finding ways to relax can help ease your mind and body as you recover. Try deep breathing, meditation, visualization, yoga, or tai chi. You might also consider pampering yourself by soaking in a warm bath, listening to music, or enjoying hot tea.
Make healthy diet choices: Inflammation-producing foods, like fried foods, processed foods, and junk foods, can increase inflammation. As you recover, consider adding anti-inflammatory foods to your diet, such as fatty fish, lean proteins, whole grains, and fruits and vegetables.
Call your healthcare provider: If symptoms of a flare-up last longer than a few days or become severe, let your healthcare provider know. They can prescribe a corticosteroid or other treatments to manage inflammation and pain.
Related: Understanding Rheumatoid Arthritis Flares
Getting a Rheumatologist Referral for Diagnosis
If you are showing early signs and symptoms of RA, you should inform a healthcare provider. They can perform a physical exam, request testing, and refer you to a rheumatologist.
A healthcare provider might suspect RA if you experience:
General pain or stiffness of the joints
Joint swelling and redness regularly, even without activity
Symptoms in multiple joints, including in the hands and feet
Symmetrical symptoms
Joint stiffness, especially after waking up in the morning, lasting a half hour or more
Any of the above symptoms lasting six or more weeks
A diagnosis of RA typically involves a physical exam, medical history, including symptoms, family history, blood work and other lab testing, and imaging like magnetic resonance imaging (MRI) and X-rays. Once your healthcare provider has gathered the findings from all these diagnostic tools, they will look at the results and make a diagnosis.
RA symptoms can be mistaken for other conditions. This is why your healthcare provider will work to rule out all other possible conditions before making an RA diagnosis.
Related: Rheumatoid Arthritis Differential Diagnosis
Some conditions that cause similar symptoms or mimic RA include:
Rheumatoid Arthritis vs. Osteoarthritis
Osteoarthritis (OA) is the most common type of arthritis. Unlike RA, osteoarthritis is not an autoimmune disease. It results from the breakdown of joint cartilage.
Causes of OA include aging, joint injuries, repetitive joint use, being overweight, and having a family history of OA. Inflammatory processes do not cause OA, so it does not affect other body areas, such as the eyes or heart.
OA develops over many years and typically affects older adults. It does not cause whole-body symptoms like fatigue and fever. It can get progressively worse with age, but unlike RA, there are no disease-modifying treatments to prevent progression.
OA is classically asymmetric (affecting only one side of the body) but can sometimes affect joints on both sides of the body (both knees or hips, etc.) the way RA traditionally does.
Mental Health, Self-Care, and Lifestyle With RA
RA and mood disorders have a clear link because of the disease's effects, such as pain, limited mobility, stress, and response to the effects of the condition. You should seek help if you are finding it difficult to cope while managing RA. Your healthcare provider can provide a counseling referral.
Self-care and lifestyle changes can help to reduce the physical and emotional effects of RA. These include:
Being active: Gentle exercise can help strengthen the muscles around the joints. Being active can also improve fatigue levels, enhance mood, and help you sleep better at night.
Learning to cope: It is essential to find ways to cope by reducing stressors in your life. Yoga, meditation, and deep breathing are good ways to manage stress.
Not smoking: Research has found smoking can lead to more severe RA, and people who smoke are less likely to experience remission (inactive disease). Smoking might also decrease the effectiveness of RA medicines and increase your risk for disease complications.
Improving sleep: Poor sleep and RA often go together. Pain makes falling and staying asleep harder, and lack of sleep increases pain. To reduce sleep troubles, set a sleep schedule, avoid caffeine later in the day, and limit screen time before bed. Talk to your healthcare provider if you are still having sleep issues.
Caring for your oral health: Gum disease has been found to cause RA progression. Make sure you schedule dental cleanings and exams and that you are brushing and flossing daily.
Summary
Rheumatoid arthritis is a common type of autoimmune arthritis that occurs when the body's immune system overreacts and attacks healthy tissues. These attacks lead to significant inflammation in the joints, organs, and other body tissues.
Common symptoms of RA are joint pain, swelling, stiffness, and systemic symptoms like fatigue and low-grade fever. RA often starts in the small joints of the hands and feet but can also affect larger joints.
Researchers do not know exactly what causes RA, but they have long suspected genetics and environmental factors might be to blame. RA development is also believed to be linked to triggers like exposure to chemicals and pollutants, chronic stress, emotional or physical trauma, lifestyle factors, an illness, or a viral or bacterial infection.
RA is manageable and treatable but currently has no cure. Early diagnosis and the right treatments can reduce pain and other disease symptoms and prevent joint damage and disability.
Read the original article on Verywell Health.

