PMS vs. PMDD: Understanding the Symptom Differences
Medically reviewed by Cordelia Nwankwo, MD
Premenstrual syndrome (PMS) is a condition of physical and emotional symptoms that occur prior to a menstrual period. Premenstrual dysphoric disorder (PMDD) is similar to PMS but much more severe in its symptoms. It impacts nearly 6% of people who menstruate.
A characterizing symptom of PMDD is that it negatively impacts everyday functioning, significantly affecting quality of life. This article will explore and compare PMS and PMDD symptoms, causes, diagnosis, and treatment options.
PMS vs. PMDD: How to Differentiate Symptoms
While PMS and PMDD are both premenstrual disorders with some overlapping symptoms, they are not the same disorder. It’s important to be accurate when discussing symptoms with your healthcare provider so you can get appropriate treatment.
PMS symptoms are less severe than those of PMDD. They include bloating, constipation, breast tenderness, and trouble concentrating, But these symptoms are not severe enough to interfere with daily activities or functioning.
Similar to PMS, symptoms of PMDD can appear in the days preceding your period and pass within a few days of the start of your period.
Symptoms of PMDD are typically more severe than PMS—significantly so, in that they negatively disrupt your life, work, relationships, and functioning. Symptoms can be wide-ranging and include:
Psychological: Irritability, anger, trouble concentrating, paranoia, severe fatigue, sleeping difficulties, lack of control
Physical: Changes in vision, eye infections, reduced urination, breast fullness and pain, skin inflammation and itching
Gastrointestinal: Nausea and/or vomiting, bloating, constipation, pelvic pressure
Neurologic/vascular: Heart palpitations, headache, fainting
The symptoms of PMDD can be so severe that they look like separate medical conditions. If you’re unsure about the severity of your symptoms and whether you might have PMDD, talk with a healthcare provider about what you’re experiencing.
What Causes PMS Compared to PMDD?
It’s not clear what causes either PMS or PMDD.
Changing hormone levels in the menstrual cycle impact people differently, which might be a cause. Hormonal changes may disrupt serotonin levels (a chemical messenger in the nervous system that regulates mood, digestion, and sleep), which can then impact mood and cause a variety of physical symptoms.
Any menstruating person can develop PMDD, but possible risk factors include:
A family history of PMS or PMDD
A personal or family history of mood disorders, including bipolar disorder, with the prevalence of bipolar disorder in people with PMDD being about 7 times higher than those without PMDD
Other factors are associated with higher risk, like smoking cigarettes or having fewer years of schooling, but more research needs to be done on this subject. PMDD is also more prevalent in people with attention deficit hyperactivity disorder (ADHD).
Talk with a healthcare provider about your risk for developing PMS or PMDD and what to watch for.
Is There a Test to Diagnose PMDD?
No specific test is used to diagnose PMDD. A complete medical history will be taken, along with a physical exam and a pelvic exam, to rule out any other possible causes. A mental health evaluation will usually be done.
You may have to document your symptoms over multiple months to give the provider a complete picture of what’s occurring. A healthcare provider will then look at your symptoms and their severity and use all available information to make an informed diagnosis.
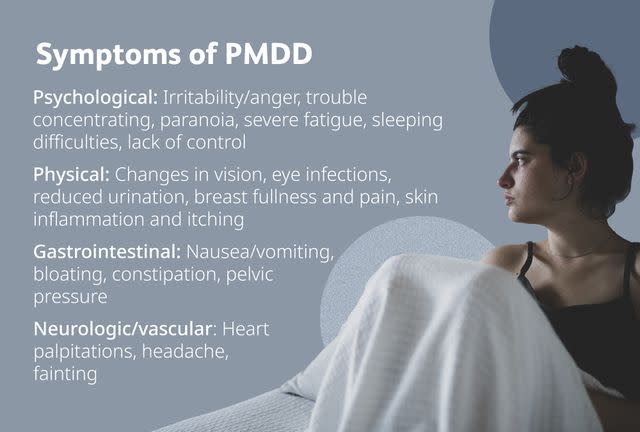
Photo Composite by Amelia Manley for Verywell Health; Getty Images
With PMDD, the symptoms are severe enough that they disrupt daily living. The symptoms can impact work, relationships, and daily functioning and are significantly different than at other times of the month.
A diagnosis of PMDD involves criteria such as:
Marked symptoms of low mood or reduced interest or pleasure
Having at least five symptoms, either physical or psychological
Symptoms that are present during the week before menses in most cycles of the previous year
Symptoms that stop before the period is over, and do not return again until one to two weeks prior to the next cycle
Symptoms that cause moderate to severe distress or interference with daily life
How to Manage PMS
Some PMS symptoms can be managed with diet or lifestyle changes, although sometimes medication can help as well. Depending on your age, symptoms, health, and other factors, you can talk with a healthcare provider about what might work best for you.
Diet and lifestyle changes can include:
Increasing protein in the diet and reducing or cutting out sugar and caffeine
Supplementing with vitamin B6, calcium, and magnesium
Incorporating regular, consistent exercise into your routine
Medication can include:
Antidepressants
Diuretics taken before symptoms begin to aid in reducing uncomfortable fluid retention
Nonsteroidal anti-inflammatory drugs (NSAIDs) for pain relief, such as Advil or Motrin (ibuprofen) and Aleve (naproxen)
Medicines to temporarily stop estrogen and progesterone production
How to Cope Through PMDD Episodes
It’s important to get treatment from a medical professional for especially bothersome symptoms, since these are much more significant than those from PMS. You do not have to deal with this by yourself. To cope with PMDD episodes:
Talk with a healthcare provider about steps you can take to change your diet and lifestyle behaviors, such as getting enough rest, drinking enough water, cutting back (or out) caffeine and alcohol, and minimizing sugar.
Seek out support, whether it’s peer support, a trusted friend or family member, a support group, or a counselor, don’t be shy about asking for the emotional support you need during these times.
Vitamin supplements may be helpful, but it’s best to talk with a healthcare provider before taking any to ensure they won't interfere with medication you are or a condition you have
When to Call for Help
PMDD can result in significant feelings of depression, feeling overwhelmed or out of control, and feeling like you’re not interested in anything anymore. This might increase suicidal feelings. You are not alone, and there is help out there. In the United States, call or text 988 for the 988 Suicide & Crisis Lifeline. It’s open 24/7 and is free and confidential.
Medications to Manage PMDD
Medications can help manage symptoms of PMDD, including:
Selective serotonin reuptake inhibitors (SSRIs) are the first-line treatment for PMDD; they include Prozac (fluoxetine), Zoloft (sertraline), and Paxil (paroxetine).
Oral contraceptive pills can help keep hormone levels steady, especially Yaz, a birth control pill with a progestin called drospirenone.
Gonadotropin releasing hormone (GnRH) agonists, such as Lupron (leuprolide) stop the production of both estrogen and progesterone. These are used less often because of side effects.
What works for one person might not work for another, and you might have to try more than one medication to find what works best for you.
Therapy and Alternative Ways to Improve PMDD
In addition to medications and lifestyle changes, some people find that there are additional treatments that can help them manage symptoms of PMDD. Always talk with your healthcare provider before adding any treatments to ensure it won’t interfere with any medications you’re taking.
Other treatments that have been found to help some people include:
Cognitive behavioral therapy (a form of talk therapy)
Herbal medicine
Summary
PMS and PMDD may share some symptoms and can look similar at times, but PMDD involves symptoms that are much more severe than PMS. These symptoms interfere with daily functioning.
There is no cure for PMS or PMDD, but there are ways to manage the symptoms, including things like lifestyle and diet changes, medication, therapy, and alternative treatments. Talk with a healthcare provider about what treatments might be best for you and your symptoms.
Read the original article on Verywell Health.

