PCOS vs. Endometriosis: What Are the Differences?

Photo Illustration by Zack Angeline for Verywell Health; Getty Images
Medically reviewed by Kiarra King, MD
Endometriosis and polycystic ovary syndrome (PCOS) are both linked to hormonal imbalances and can lead to infertility. However, these two conditions affect female reproductive organs differently.
PCOS primarily affects the ovaries and is linked to excess androgens, commonly considered male hormones, though females do make them in small amounts. Endometriosis is associated with higher levels of the female hormone estrogen. It can affect the ovaries, the uterus, and other organs in the lower abdominal cavity, such as the bladder and intestines.
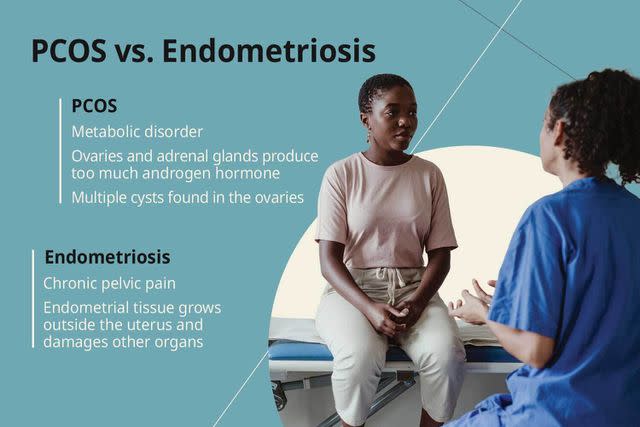
Photo Illustration by Zack Angeline for Verywell Health; Getty Images
Approximately 6% to 10% of people with a uterus are diagnosed with endometriosis. Between 6% and 12% of people assigned female at birth are diagnosed with PCOS. Both occur during the childbearing years.
This article explains the differences between PCOS and endometriosis. It also discusses the symptoms of each and how they are diagnosed and treated.
How to Know if It's Endometriosis or PCOS
Although endometriosis and PCOS share symptoms, they are different conditions. Endometriosis causes chronic pelvic pain, while PCOS is a metabolic disorder.
What Is Endometriosis?
The innermost lining of the uterus is called the endometrium. The endometrium helps keep the uterus functioning properly, especially during pregnancy. When the endometrial tissue begins to grow outside the uterus, it's called endometriosis. Endometriosis is the most common cause of pelvic pain in women of childbearing age.
What Is PCOS?
PCOS occurs when the ovaries and adrenal glands produce too much androgen hormone. This is called hyperandrogenism.
The ovaries have several important functions, including the release of reproductive hormones. The growth and release of an egg from the ovary (ovulation) depend on those reproductive hormones.
In addition, cysts (fluid-filled sacs) form in the ovaries of most people with PCOS.
Symptoms
Endometriosis and PCOS have a few common symptoms, including heavy menstrual periods and infertility. However, several differences set them apart.
Endometriosis
Constipation
Frequent urination
Heavy periods
Infertility
Painful bowel movements
Painful sex
Urinary urgency
PCOS
Diabetes and insulin resistance
Fluid-filled sacs in the ovaries
Excess body and facial hair
Infertility
Infrequent menstrual cycles
Male-pattern baldness
Masculine features
Obesity
Severe acne
Endometriosis is primarily marked by chronic pelvic pain and painful, heavy periods. It can also cause bladder, bowel, and sexual dysfunction.
Signs of PCOS are more systemic. In addition to infrequent periods, the hormonal imbalance in PCOS leads to excess hair growth on the face and body (hirsutism), severe acne, and male pattern baldness.
PCOS is a metabolic disorder. It commonly presents along with excess body weight, obesity, diabetes, insulin resistance, and acanthosis nigricans—patches of thick, velvety, darkened skin on the neck and skin folds associated with insulin resistance.
Causes and Risk Factors
Although hormonal imbalances play a part in endometriosis and PCOS, other causes and risk factors are unique to each condition.
Endometriosis
It's unclear what causes endometriosis, but possibilities include retrograde menstruation (menstrual blood flowing in the wrong direction), genetics, impaired immune system, increased estrogen levels, and abdominal surgery (endometrial tissue can be transferred to other organs during surgery).
Endometriosis risk factors include:
Early menarche (before age 11)
Family history of endometriosis (mother or daughter)
Short monthly periods (27-day cycle or less)
Heavy menstrual bleeding
Infertility
High estrogen levels
Alcohol use (increases estrogen levels)
PCOS
Although the exact reason why PCOS occurs is not fully understood, experts agree that it is a complex endocrine condition with multiple causes, including diet and lifestyle factors.
Fat cells also release androgens, which is why it's not uncommon for obese people to experience PCOS. Hyperandrogenism also leads to insulin resistance and diabetes.
Additionally, the hormonal changes lead to anovulation, subsquently irregular menstrual cycles, and possible infertility. PCOS is one of the most common causes of female infertility, affecting 70% to 80% of people wanting a pregnancy.
Risk factors for having PCOS include:
Obesity
Diabetes
Hyperandrogenism
Family history of PCOS
Premature puberty (before age 8 or 9)
Is There a Link Between Endometriosis and PCOS?
A study found that although endometriosis and PCOS share abnormalities in hormonal balance, body weight, age of menarche (when periods start), and reproductive irregularities, the causes of those abnormalities differ. Therefore, a link between the two gynecologic disorders cannot be made.
Can You Have Both?
Although rare, people can have both endometriosis and PCOS. Such reported cases show that endometriosis is often mild when found in combination with PCOS.
Diagnosis
Endometriosis and PCOS require several tests to confirm their diagnosis. Endometriosis often takes longer to diagnose than PCOS.
Diagnosing Endometriosis
The following are ways to diagnose endometriosis:
Pelvic exam: Identifies masses, cysts, and areas of pain.
Imaging tests: A pelvic ultrasound can help find cysts in the ovaries, while magnetic resonance imaging (MRI) recognizes endometriosis by taking pictures of organs and tissues.
Laparoscopy: A surgery that looks in your abdominal cavity to find signs of endometriosis. The surgeon may diagnose endometriosis by visualizing the invading tissue; however, a biopsy (removing a sample of tissue to be examined in a lab) may be required to confirm the diagnosis.
Your healthcare provider may give you medications that help decrease estrogen levels. If medications relieve your symptoms, you likely have endometriosis.
Diagnosing PCOS
The following are ways to diagnose PCOS:
Physical exam: Identifies increased body mass index (BMI), and signs of other conditions that could be responsible for PCOS symptoms
Pelvic ultrasound: Helpful in finding ovarian cysts
Blood work: Checks for increased androgen levels, thyroid disease, diabetes, and cholesterol level
Your healthcare provider will also review a history of your menstrual cycles and fertility.
Treatment
Medications, surgery, and lifestyle changes can improve the symptoms and quality of life for people with endometriosis or PCOS.
How Endometriosis Is Treated
Treatment for endometriosis is often geared toward pain management. However, considering the person's desire for pregnancy is also important.
Medications: Nonsteroidal anti-inflammatory drugs (NSAIDs) are used first to decrease inflammation and alleviate discomfort. Hormonal medications such as Myfembree (relugolix, estradiol, and norethindrone acetate) and Orilissa (elagolix), and non-hormonal medications (aromatase inhibitors) can help reduce pain and inflammation.
Surgery: Removal of the uterus, fallopian tubes, and ovaries may be necessary to alleviate the symptoms of endometriosis. In addition, removing endometrial tissue from other organs (bladder, colon) may also be an option. Unfortunately, it's not uncommon for endometriosis to recur (come back) after surgery.
Lifestyle: A study found that cooking with clean ingredients, eating more fresh fruits and vegetables, and decreasing gluten and dairy improved endometrial symptoms. This study was supported by other research indicating a healthy lifestyle can improve both the physical and mental challenges of endometriosis.
How PCOS Is Treated
Treatment of PCOS is tailored to decrease the symptoms and reduce the long-term health implications caused by it, which include diabetes and cardiovascular disease. The following are ways to treat PCOS:
Medications: Increased androgen levels lead to health complications such as insulin resistance, diabetes, increased cholesterol levels, and heart disease. Oral contraceptives and antiandrogens help alleviate PCOS symptoms and reduce androgen levels.
Lifestyle: Making lifestyle changes is the first-line treatment for PCOS. Losing 5% to 7% of body weight can produce a regular menstrual cycle, improving pregnancy chances. Anxiety and depression are prevalent in people with PCOS. An improved lifestyle and sense of well-being have improved the quality of life for those with PCOS.
When to See a Healthcare Provider
Call your healthcare provider for the following symptoms:
Heavy, irregular, or absent periods
Chronic pelvic pain
Signs of androgen excess
Infertility
Summary
Endometriosis and PCOS are different gynecologic disorders but are both chronic conditions that are difficult to manage.
Endometriosis occurs when endometrial tissue travels outside the uterus and damages other organs. PCOS, however, occurs when androgen levels are abnormally elevated, and multiple cysts are found in the ovaries. PCOS results in signs of androgen excess and infertility.
Endometriosis and PCOS are managed with medications, surgery, and lifestyle changes. Although treatable, neither condition is curable.
A Word From Verywell
Endometriosis and PCOS can be frustrating conditions to manage. Fortunately, they rarely occur together, but each disorder can negatively affect your quality of life.
Although living a healthy lifestyle can alleviate the symptoms of endometriosis and PCOS, having a sense of well-being also improves these conditions. It's essential to have social support in addition to medical help when living with endometriosis or PCOS.
Frequently Asked Questions
Can endometriosis cause you to gain weight?
No. Endometriosis does not usually cause weight gain; most people with this condition are average or underweight.
Can PCOS trigger endometriosis?
PCOS and endometriosis are not linked and do not trigger one another.
Is PCOS an autoimmune disease?
PCOS is not considered an autoimmune disease; it is the most common endocrine disorder in women.
What is the best diet for PCOS and endometriosis?
A diet of natural ingredients and rich in fresh fruits and vegetables improves symptoms of endometriosis and PCOS. Exercising also improves quality of life.
Can PCOS cause cancer?
PCOS has been shown to increase the risk of developing certain types of cancer, such as endometrial cancer.
Can PCOS and endometriosis cause infertility?
PCOS and endometriosis have high rates of infertility. About 30% to 50% of people with endometriosis are infertile, and 70% to 80% of people with PCOS experience infertility.

