How Oral Cancer Is Treated
Medically reviewed by Gagandeep Brar, MD
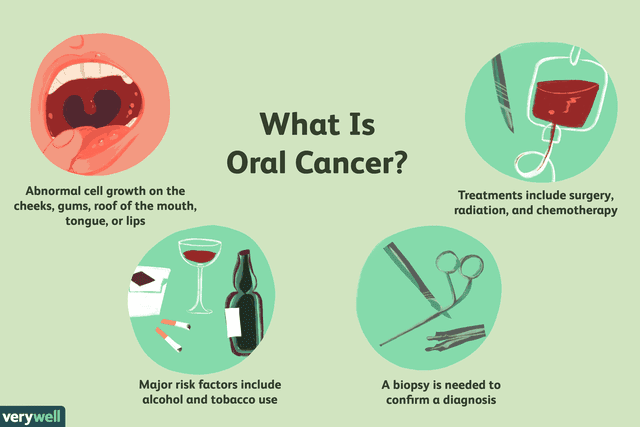
The best treatment options for oral cancer depend on many factors, including the location of the tumor, the stage of the disease, and general health. Unlike many cancers, the mainstay of therapy can be surgery, chemotherapy, or radiation therapy, and both chemotherapy and radiation may be used with a curative approach.
When surgery is used, it is not always the first step. Chemotherapy (with radiation) may be given either before surgery, to reduce the size of the tumor, or after surgery, to clean up any cancer cells that may have been left behind. If there is a chance that a cancer has spread to lymph nodes, a lymph node dissection is often done. Reconstructive surgery with skin, muscle, and/or bone grafts may be needed. There is also one targeted therapy that can be used for some people with oral cancer, as well as clinical trials looking at newer treatments such as immunotherapy.
Most people with oral cancer will have a team of healthcare providers they work with. This can include an otolaryngologist (ear, nose, and throat specialist or ENT), different types of oncologists such as a medical oncologist and radiation oncologist, a plastic and reconstructive surgery specialist, and dentists. Support specialists such as speech pathologists, physical therapists, and dietitians are also often included.
A psychologist is an important member of the team in helping people cope not only with a diagnosis of cancer, but the physical issues and emotional changes that can accompany a diagnosis of oral cancer.
Surgery
Surgery is the mainstay of treatment for oral cancer, but is not always the first step in care. Since these surgeries can sometimes be complicated and disfiguring, choosing a surgeon who performs a large number of such surgeries is wise. Experience can make a big difference not only in successfully removing an oral cancer, but doing so with the least amount of damage to healthy tissue.
Takeaway
As has been seen with some other cancers, a 2017 study found that people who seek treatment for oral cancer at cancer centers that treat large numbers of people with the disease, may have better outcomes.
If you're not certain where to begin in locating a surgeon with a great deal of experience, some healthcare providers recommend seeking out an opinion at one of the National Cancer Institute designated cancer centers.
Surgery to Remove the Tumor
Surgery to remove oral cancer offers the chance for a cure, and may be done right after diagnosis, or following treatment with chemotherapy (and possibly radiation therapy) to reduce the size of the tumor. The tumor is removed completely when possible, along with a margin of normal tissue. Specific procedures may include:
Mohs surgery: Mohs surgery is a surgical approach in which a surgeon removes a small amount of tissue and looks at it under the microscope. This is done repeatedly until no evidence of cancer remains. The procedure may be beneficial with tumors such as those of the lip, where removing even a small amount of normal tissue could be disfiguring.
Laryngectomy: Removal of the voice box is sometimes necessary to remove a tumor completely, but not often.
Glossectomy (partial or total): Partial or total removal of the tongue may be needed for cancers of the tongue. When a third or less of the tongue is removed, speech therapy can often help people regain their normal speech.
Maxillectomy (partial or total): Removal of the bone that forms the roof of the mouth is sometimes needed.
Mandibulectomy (partial or total): Removal of part, parts, or all of the jaw bone is sometimes needed. When this occurs, bone grafts from the hip and other regions of the body can often repair the defect left.
Tracheostomy: Creating a hole in the trachea (the windpipe) may be needed with some oral cancers. This may be a permanent procedure when an extensive tumor is involved, or it may be a temporary solution to make sure the airway is maintained while swelling from surgery, chemotherapy, or radiation is present.
Feeding tube: Oral cancer surgery can cause difficulty with eating, and a temporary feeding tube such as an NG tube or G tube may be needed to maintain nutrition.
Takeaway
Different surgical techniques, such as robotic surgery, may be used, particularly with cancers such as throat cancer.
Lymph Node Dissection
If an oral cancer has spread to lymph nodes in the neck, or if there is a possibility that it has, a lymph node dissection is usually done at the time of surgery. In this procedure, surgeons predict which lymph nodes a cancer is likely to drain to and remove these nodes so they can be examined for the presence of cancer cells.
At some institutions, a sentinel lymph node biopsy (similar the a breast cancer sentinel node biopsy) may be performed. In this procedure, a radioactive marker and dye are injected into a tumor, and traced to the first lymph nodes to which the cancer would spread. These specific lymph nodes can then be biopsied, and if no cancer is found, further removal of lymph nodes may not be necessary.
Variations of lymph node dissection may include a partial dissection, in which only a few nodes are removed, a modified radical lymph node dissection, in which most lymph nodes are removed as well as some muscle and nerves, and a radical lymph node dissection in which muscles, nerves, and veins are removed in addition to lymph nodes.
Reconstructive Surgery
Depending on the location and extent of the original surgery, further reconstructive surgeries may be needed. These may include bone, muscle, or skin grafts, or flap procedures. Dental implants may also be needed.
Takeaway
Recent advances in reconstructive surgery now allow many people who have had even major oral cancer surgery to achieve a cosmetically acceptable result.
Side Effects
Possible complications of surgery can include problems related to anesthesia, infection, or bleeding. Depending on the size or extent of surgery, eating, talking, and breathing can be compromised. A tracheostomy tube may be needed to assist with breathing, and a feeding tube may be needed to ensure good nutrition.
Speech therapy and physical therapy may also be needed. Any surgery carries the risk of blood clots, as does the presence of cancer itself, and therefore precautions should be taken to minimize the risk of blood clots.
Chemotherapy
Chemotherapy is frequently used to treat oral cancers. It works by killing rapidly growing cells in the body such as cancer cells. Since normal cells (such as hair follicles and cells that line the digestive tract) may also divide rapidly, side effects are common.
Timing
Chemotherapy for oral cancer may be given as:
Adjuvant therapy: The term adjuvant means "in addition to" and refers to chemotherapy that is given along with (and after) surgery. While surgery may remove all visible signs of a cancer, any leftover cancer cells may continue to grow, resulting in a recurrence of the cancer. Adjuvant therapy is given in combination with radiation in the hope of reducing the risk of recurrence.
Chemotherapy Drugs
There are many different types of chemotherapy drugs that work on different parts of the cell cycle (the stages a cell goes through in the process of dividing into two cells instead of one). These drugs may be used alone or in combination, and are usually given in cycles every few weeks. Drugs commonly used for oral cancer include:
Platinol (cisplatin)
Paraplatin (carboplatin)
5-FU (5-fluorouracil)
Taxol (paclitaxel)
Taxotere (docetaxel)
Trexall (methotrexate)
Side Effects
There are a number of side effects of chemotherapy, though the management of these effects has improved significantly in recent years. Common side effects include:
Hair loss
Bone marrow suppression: Cells in the bone marrow that develop into white blood cells, red blood cells, and platelets, divide rapidly, and therefore levels of these cells is often reduced in people on chemotherapy.
A decrease in a specific type of white blood cells known as neutrophils (chemotherapy-induced neutropenia) can lead to an increased risk of infections. A decrease in red blood cells (chemotherapy-induced anemia) can cause fatigue and palor. A decrease in platelets (chemotherapy-induced thrombocytopenia) can lead to easy bruising and bleeding.
Medications are available that can stimulate the production of white blood cells, making chemotherapy safer than in the past.Nausea and vomiting: One of the more dreaded side effects of chemotherapy is nausea and vomiting, though many people now experience minimal symptoms with the use of medications to prevent nausea.
Peripheral neuropathy: The chemotherapy drugs used for oral cancer, such as the taxanes Taxol and Taxotere, and platinums, often cause peripheral neuropathy. Symptoms include numbness and tingling in the hands and feet. This symptom may be temporary, or it may persist long-term after treatment. There are currently studies looking at methods to reduce this risk, and it is worth talking to your oncologist about these.
Mouth sores and taste changes: Mouth sores are common with chemotherapy, and chemotherapy drugs, especially platinum drugs such as Platinol and Paraplatin, often cause a metallic taste in the mouth.
Takeaway
Long-term side effects of chemotherapy may also occur, though the benefits of treatment usually far outweigh these risks. Some chemotherapy drugs can increase the risk of heart disease, or increase the risk of developing secondary cancer such as leukemia.
Radiation Therapy
Radiation therapy uses high energy waves to destroy cancer cells. It may be used alone, as the primary treatment for oral cancer, or it may be used before or after surgery (with or without chemotherapy). It can also be used to reduce symptoms related to advanced cancers. In general, radiation alone is an option as the primary treatment only for smaller oral cancers. Radiation can be given in one of two ways:
External beam radiation therapy: External radiation is the type of radiation that most people are familiar with. It is often given five days a week for six to seven weeks. It can also given as stereotactic body radiation (SBRT) in single treatment or several bi-weekly treatments administered over two to three weeks.
Internal radiation therapy (brachytherapy): Less commonly, radioactive seeds can be implanted in a tumor to treat the cancer.
Takeaway
Of note is that people with oral cancer who smoke do not respond as well to radiation therapy as those who do not smoke during treatment.
Proton Beam Therapy
Proton beam therapy is a newer option in treating oral cancer. It works in a way similar to radiation, but instead uses high energy protons to destroy cancer tissue. In general, the effectiveness of proton beam is similar to that of radiation therapy, but due to the mechanism of how it works (high energy rays continue on beyond a tumor to some degree while protons stop), it may cause less damage to normal tissues than traditional radiation therapy.
Side Effects
Common side effects of radiation therapy are redness and discomfort of the skin overlying the area where radiation is given, and fatigue. Inflamed mucous membranes in the mouth are also common. Damage to salivary glands can cause a dry mouth. Damage to the jaw bone can sometimes result in a condition known as osteonecrosis of the jaw. A loss of the sense of taste and hoarseness also occur at times, depending on the location of the tumor. Radiation to the neck region may cause inflammation of the esophagus (radiation esophagitis).
Radiation can also result in scarring and tightening of tissue (radiation fibrosis) causing stiffness of the jaw, but it's been found that treating people with a drug called Ethyol (amifostine) reduces radiation damage to normal tissue.
With cancer survival rates improving, its become more important to consider the long-term side effects of radiation therapy as well. In addition to radiation fibrosis (which is permanent) leading to stiffness, radiation may cause hypothyroidism due to damage to the thyroid gland, and dental decay due to disruption of the salivary glands. Like chemotherapy, radiation may cause a slight increase in the risk of heart disease as well as secondary cancers, especially when combined with chemotherapy.
Targeted Therapy
Targeted therapies are drugs that specifically target cancer cells or the pathway that is used in the process of a cancer cell reproducing.
Takeaway
Since these drugs are more specific for cancer, they often (but not always) have fewer side effects than chemotherapy.
Erbitux (cetuximab) is a monoclonal antibody that targets a protein on the surface of cancer cells that causes them to divide and reproduce. Targeted therapies do not "cure" cancer, but may control the growth of a cancer for a significant period of time. They are often used along with chemotherapy and radiation. Erbitux may be used alone in advanced or metastatic tumors. When indicated, Erbitux may improve survival for those with oral cancer.
Side Effects
Side effects are usually milder than those with chemotherapy and can include an EGFR inhibitor skin rash (a rash similar to acne but not acne) and diarrhea. There is also a risk of allergic reactions.
Immunotherapy
Immunotherapy with Keytruda (pembrolizumab) is another treatment option.
Clinical Trials
There are many in-progress clinical trials looking for better methods of treating oral cancer or those that have fewer side effects. Some of these studies are looking at combinations of the treatments above, and others are looking at newer ways to treat cancer.
As with many other cancers, there is hope that immunotherapy might benefit people with oral cancer. Immunotherapy drugs such as Opdivo (nivolumab) and Keytruda (pembrolizumab) are currently FDA approved for the second line treatment of advanced and metastatic oral cancer. These drugs work, simplistically, by removing the brake that cancer cells are putting on the immune cells, helping the body's own immune system recognize and attack cancer cells.
Palliative Therapy
Many people are frightened by the term "palliative care," but in fact, palliative care can be helpful even for people with very curable cancers. Palliative care is defined as treatment that focuses on improving a person's physical, emotional, and spiritual well-being as they cope with a disease such as cancer. While hospice is considered a form of palliative care, palliative care is often used side by side with conventional treatments for cancer such as surgery, chemotherapy, and radiation.
Takeaway
Many of the larger cancer centers now have palliative care teams who can help coordinate care for those living with cancer. These teams may include a healthcare provider, a nurse specialist, therapists such as physical therapists and occupational therapists, and behavioral health professionals such as psychologists.
Since the concept of palliative care is so new, people may have to initiate the discussion asking for a consult. Symptoms that may be addressed with palliative care include pain control, nutrition, nausea, loss of appetite, and much more.
Complementary Medicine (CAM)
At the current time there are not any alternative therapies that are effective in treating oral cancers, yet many of the therapies that fall under this heading can help people cope with the symptoms of cancer and cancer treatment.
Many of the larger cancer centers now offer these treatments in an integrative approach to cancer; combining these modalities with conventional cancer treatments. Some of the alternative therapies to treat cancer symptoms that may benefit people with oral cancer include meditation, massage therapy, yoga, music therapy, art therapy, and even pet therapy.
There is also some evidence that acupuncture may help people with cancer but it's important to talk to your healthcare provider before you try this.
Many people wonder about the benefits of vitamins or dietary supplements with oral cancer. We still do not know if the findings from lab and animal studies will translate to any benefit when used in the human body.
Takeaway
If you do wish to try any of these modalities, first talk to your healthcare provider. There are some vitamin supplements that may interfere with chemotherapy or radiation.
Supportive Care/Lifestyle
In addition to the treatments above, there are many things you can do yourself to improve your quality of life and potentially, your outcome. Taking the time to learn about your cancer, and being an advocate for your own care, can help you feel on top of what is happening with your body, and may even improve outcomes. Gathering together a supportive community of friends and family is essential, as nobody should face cancer alone.
Becoming involved in a support community, either a local support group or an online support community can provide support, while helping you learn the latest about oral cancer treatment. Talking to others who have faced oral cancer can be priceless as you cope with some of the issues posed by oral cancer; issues such as speaking, eating, and breathing, that those not living with oral cancer take for granted.
Finally, if you smoke, seek out help in quitting. As noted earlier, people who smoke are less likely to respond to radiation therapy, and there are many other reasons why quitting smoking is important after a diagnosis of cancer.
Frequently Asked Questions
Can you talk and eat if you have tongue cancer surgery?
Yes, but it may take some time. After tongue surgery, speech pathologists can work with other healthcare providers to help you speak clearly again and re-learn how to swallow.
What is the prognosis for HPV oral cancer?
Survival rates are not specifically reported for HPV-related oral cancers, but some researchers believe that cancers that test positive for HPV may have better outlooks than non-HPV oral cancers. The HPV virus is usually linked to oropharyngeal cancer, which has an overall five-year survival rate of 49%.
Read the original article on Verywell Health.

