How Often to Test Your Blood Glucose
Make the Most of Your Meter

How often should you check your blood sugar? The answer depends on the type of diabetes you have, your blood glucose level targets, and more practical matters, such as whether you can afford or have enough test strips.
Don't Miss: 12 Healthy Ways to Lower Your Blood Sugar
Recent studies show that people with type 2 diabetes (PWDs type 2) who don't use medications but do self-monitor blood glucose might not see much difference in blood glucose control compared with people who don't self-monitor. But using a meter to check your blood glucose levels strategically can provide helpful information to guide you in selecting:
* foods
* portions
* exercise
* medication doses
With this guide on finding how often to test, discovering how accurate your meter is, and more, we'll show you what you need to know about testing your blood sugar.
When Is the Best Time to Test Blood Sugar?

Many people newly diagnosed with type 2 are encouraged to check fasting blood glucose levels. Diabetes educator Deb Bjorsness, R.D., CDE, from Great Falls, Montana, says: "It's pretty common for providers to say, 'Just check first thing in the morning; that's good enough.' "
Bjorsness has seen when it isn't good enough. "People come in and the only time they test is first thing in the morning, and their A1C has come back 8, 9, or 10 percent. That's the beauty of doing blood sugars at other times of the day, like after meals. This can help you and your providers see where the problems are."
If you've settled into a diabetes plan and your fasting blood glucose results are within your goal range, a better use of the next test would be to check at a different time. There are many times when you can test your blood sugar, such as an hour or so after you eat, when you're sick, after you start a new medication, after medication changes, or when you're under a lot of stress. Some standard blood sugar checkpoints include:
* fasting
* before meals
* after meals
* before bed
* during the night
Consider Testing Before a Meal

If you're on a flexible insulin plan (multiple daily injections of long- and rapid-acting insulins or an insulin pump), you need to check before you eat to determine the dose of rapid-acting insulin you need. If you have type 2 diabetes and are starting to take insulin once a day, your provider or diabetes educator will probably adjust your dose based on your daily fasting glucose results and perhaps other results.
Below are target blood sugar guidelines for adults with diabetes who have no other health issues. There's a slight difference between the two organizations' recommendations. Ask your provider about specific fasting and after-eating glucose levels and A1C targets that are right for you.
Guidelines for testing before a meal:
American Diabetes Association: 70-130 mg/dl
American Association of Clinical Endocrinologists: Less than 110 mg/dl
Consider Testing After You Eat

Whether or not you take insulin or one or more other glucose-lowering medications to control your blood glucose levels, consider checking one to two hours after you eat to see how certain meals affect your blood sugar. This is especially helpful when you are first diagnosed. It's also useful to do what's called paired testing, which is testing before you eat and then again after you eat. Doing this at your biggest meal of the day can be valuable.
Below are target blood sugar guidelines for adults with diabetes who have no other health issues. There's a slight difference between the two organizations' recommendations. Ask your provider about specific fasting and after-eating glucose levels and A1C targets that are right for you.
Guidelines for checking glucose after a meal (postprandial):
American Diabetes Association: Less than 180 mg/dl (1-2 hours after start of meal)
American Association of Clinical Endocrinologists: Less than 140 mg/dl (2 hours after meal)
Consider Testing at Night
Bedtime checks (at least two hours after the evening meal) are recommended for:
* People who take multiple daily injections.
* People who use an insulin pump.
Checking before bed may be recommended if you take basal insulin, such as Levimir or Lantus, once a day at bedtime or split your dose of long-acting insulin into two injections.
What you should know about middle-of-the-night checks:
* People who use insulin may be advised to do checks in the middle of the night to reveal hypoglycemia (blood glucose under 70 mg/dl) during the night. Talk to your provider about nighttime testing options for you.
Consider Testing Before and After Exercise

Check to see how exercise affects blood sugar by occasionally testing immediately before and after exercise. Aerobic activity tends to lower blood sugar, even hours after stopping. This is not the case if you take insulin and start exercising when your blood sugar is high. Exercise can cause blood sugar to rise because you don't have enough insulin to get glucose into the cells. Strength training, such as weight lifting, may temporarily increase blood sugar levels, but it has long-term glucose-lowering benefits.
Don't Forget These Important Times to Test
You should also test your blood sugar if you:
* Are sick or have an infection. Illness can send blood sugar levels up. Do a check every two to four hours. If it's:
* Over 250 mg/dl, check your urine for ketones (a sign the body is burning fat for energy and might have insufficient insulin); if ketones are present in more than trace amounts, call your doctor.
* Over 250 mg/dl for more than six hours, call your doctor.
* Over 350 mg/dl even once, call your doctor.
* Start a new blood glucose-lowering medication or change the dose of one. A prescription or over-the-counter medicine for a condition other than diabetes may affect blood sugar levels. Steroids are one example.
* Are under a lot of stress. Emotional stress may lead to higher blood sugar numbers. Exercise -- even just a walk around the block -- can help reduce stress and glucose levels.
* Feel as though your blood sugar level is too low. If your meter confirms it with a number of 70 mg/dl or less, eat 15-20 grams of pure glucose (tablets or gel) or drink 1/2 cup fruit juice or regular soda. Wait 15 minutes and check again to make sure it has come back into the normal range.
Get the Best Use Out of Your Strips

There are many times you could check. How often should you? "Everyone wants black-and-white answers," says Mary M. Austin, R.D., CDE. "It's not how often you do it; it's what you do with the information."
Endocrinologist Tom Elasy says people and health care providers need to distinguish between the intensification stages of diabetes -- when diabetes is newly diagnosed or when you and your provider make changes in your treatment plan -- and the maintenance phase -- when you are reaching your glucose goals and things are in a pretty steady state.
How to Make the Best Use of Your Strips: Medicare, for people who have Part B, covers 100 test strips every three months for a PWD who doesn't take insulin.
For someone newly diagnosed with type 2, how can you make the best use of your strips? According to Elasy, use more strips when you're diagnosed and learning about the impact of what you eat, your physical activity, and medications on your glucose levels. Once you get a sense of your fluctuating glucose levels, testing doesn't need to happen as often. As type 2 diabetes progresses over time, renewed, more frequent testing often is necessary.
People who do not take any glucose-lowering medications might want to check at least once or twice a week just to keep track. It is recommended that you do monitor and use your allotted strips wisely. Monitoring can have a powerful, positive effect on how you subsequently eat or the likelihood that you'll take a walk, Elasy notes.
When your glucose levels are pretty stable, move around the times that you check. If you're not willing to check regularly, diabetes educator Deb Bjorsness says to at least do some spot checks. "Two hours after your biggest meal is probably your best time for information," she says.
What You Need to Know About Glucose Meter Accuracy
Here are some things that can affect readings:
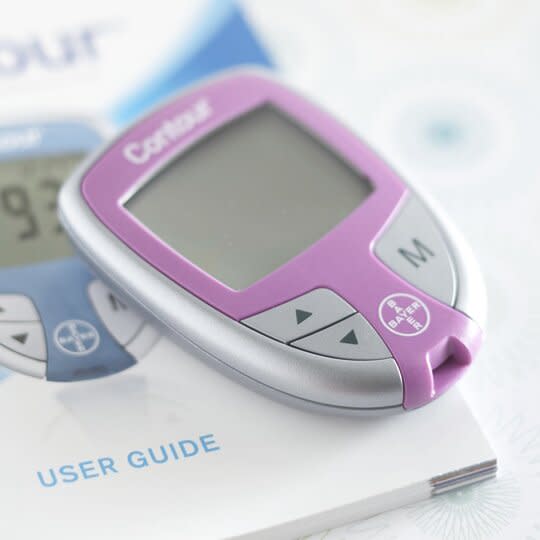
User error. Suspicious of the results? Read and follow the user guide instructions that come with your meter. Store your meter and strips away from sunlight and temperature extremes. Check the viability of each new bottle of test strips by running a check using glucose control solution (if your meter uses control solution).
Laboratory versus at-home results. Meters intended for self-monitoring by people with diabetes are allowed to vary by as much as plus or minus 10 percent from the results laboratory equipment would give.
Location of the blood. Blood glucose levels differ within the body. Rapid changes from dosing insulin or eating show up first in blood obtained from the fingertips.
Keep Track Of and Learn From Your Blood Glucose Checks
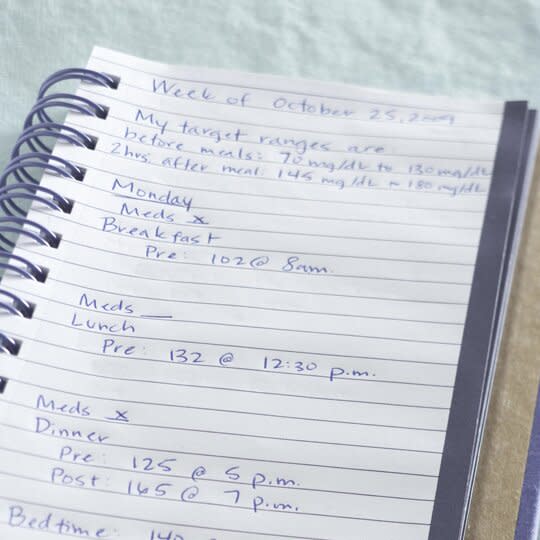
You should keep a record of your glucose checks in the format you prefer. Perhaps you like writing your results into a record book. Or you want to go high-tech and use one of the many mobile or online apps that are available. Find what works best for you.
Keeping track of your results is important because they enable you and your provider to look back and observe trends and patterns in your numbers. With this information, you and your provider can make changes in and improve your management as needed. Don't wait for your provider to download your meter at each visit. Keep track of your results, observe them, and be ready to discuss them with your provider at each visit.
Make use of any data you collect:
* Circle, highlight, or make note in some way of the numbers that are outside your target range.
* Three glucose levels from the same time of day that are out of range are a pattern. If you don't know what to do about the pattern, call your health care provider.
* If you use a logbook to record your results and run out of room, go to the meter manufacturer's website. Some have log sheets you can print.
Get a Good First Drop for Accurate Blood Glucose Results

Diabetes educator Deb Bjorsness, R.D., CDE, suggests taking these steps to get a good drop of blood with the least pain and most accurate results:
1. Wash. "It's amazing how many people don't wash their hands prior to doing a check," Bjorsness says. "Say you eat an apple. You don't realize you have apple residue on your fingers. If you don't clean your hands, you could have a blood sugar result that is artificially high. If you use insulin, that can be a real issue." Bjorsness recommends just using soap and warm water. "Save the alcohol pads for when you are out and about and don't have access to a sink," she says.
2. Shake. Give your hands three to five shakes below your heart to get the blood down to the fingertips. For those of you who remember shaking down a mercury thermometer, that's the snap you want.
3. Stick. Set your lancet to the right depth for you. "You need a depth on the device to get just enough blood without having to squeeze the life out of your finger. Don't go deeper than you need," Bjorness says. For less pain, use the sides of your fingers, which have fewer nerve endings than the pads. Or try an alternate lancing site, such as the fleshy parts of your palm or forearm.
4. Milk. Gently milk the finger down. Don't squeeze hard or you might change the composition of the blood, affecting the result.
Know Your Blood Glucose Targets
Before you use another test strip, make sure you know your blood glucose targets.
In a telephone survey of 500 people with type 2 diabetes, over half of those taking no diabetes medication, 30 percent of those taking pills, and 12 percent of those taking insulin did not have blood sugar level targets. See our blood glucose guidelines for general targets. Then ask your health care provider what ranges are right for you.
Type of test: Fasting (before breakfast)
American Diabetes Association recommends: 70-130 mg/dl
American Association of Clinical Endocrinologists recommends: Less than 110 mg/dl
Type of test: A1C (shows blood sugar levels over time)
American Diabetes Association recommends: various A1C goals, from 6.5 percent to less than 8 percent. Talk to your provider about what A1C goal is best for you based on your diabetes control, age, and overall health. If you can keep your glucose levels in tight control with minimal hypoglycemia, then 6.5 percent may work well for you. However, if you are older, have had diabetes for many years, or have some unawareness of hypoglycemia, then an A1C of 8 percent may be better.
American Association of Clinical Endocrinologists recommends: 6.5 percent or less
Note: A woman who is pregnant or trying to get pregnant will have lower target numbers for the health of her baby. Children have higher target numbers. Elderly people, especially those who have cardiac disease, may have higher target numbers.
Have you heard about continuous glucose monitoring? The finger prick may become a thing of the past as continuous glucose monitor (CGM) technology improves. Could these systems help with your diabetes management?
