My OCD Symptoms Controlled My Life for 15 Years—Then, the Pandemic Hit

"Hearst Magazines and Yahoo may earn commission or revenue on some items through the links below."
When I was first diagnosed with obsessive compulsive disorder (OCD) in college, a psychologist gave me a book called The OCD Workbook. That night, in my dorm room, I read the book cover to cover and felt a wave of relief wash over me. Inside its pages were all the things I’d been going through: checking behaviors, ruminating thoughts and irrational health fears. For years, I’d been constantly checking to make sure doors were locked and appliances were unplugged. I’d then obsessively worry that I missed something while checking and it would cause something horrible to happen like a fire or a burglary. Although, it was comforting to know that there were other people like me in the world, but I didn’t fill out the workbook. I was embarrassed and didn’t want to admit I had OCD, so I stopped seeing my therapist.
What is OCD?
Obsessive-compulsive disorder (OCD) is characterized by repetitive, unwanted, intrusive thoughts (obsessions) and irrational, excessive urges to do certain actions (compulsions). Although people with OCD may know that their thoughts and behavior don’t make sense, they are often unable to stop them. Symptoms typically begin during childhood, the teenage years or young adulthood, although males often develop them at a younger age than females. 1.2% of U.S. adults experience OCD each year, according to the National Alliance on Mental Health.
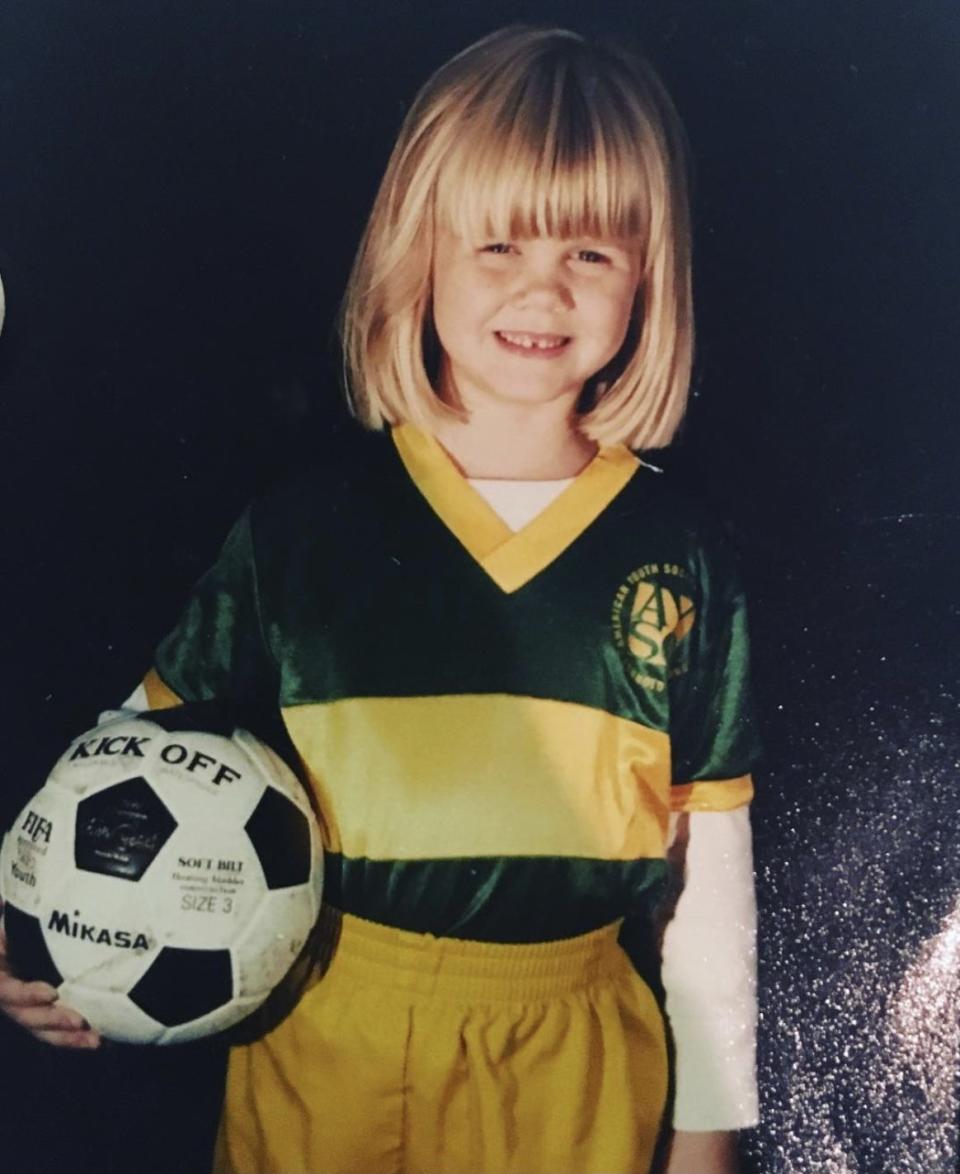
My OCD symptoms affected my life at least as far back as first grade.
I didn’t develop OCD in college; I have always had it. Even though I was really outgoing, I was still an anxious kid. In first grade, I quit the Girl Scouts because I feared my mom would forget to pick me up afterwards. I didn’t have any fun because I was sick with worry the entire time. In fifth grade when a man’s leg rubbed up against mine while waiting for a ride in Disney World, I somehow thought I got pregnant. It ate at me the entire vacation until I finally caved and told my mom my concern, who reassured me that it was impossible for me to pregnant from one leg touching another leg. For years, I babysat but was always a wreck thinking the kids might die in their sleep. I’d check on them every few minutes to make sure they were breathing.
As I got older, my OCD got increasingly worse. I started taking pictures on my phone of all the appliances in my apartment before I left, so I’d know I didn’t start a fire. I’d circle the block of my house numerous times to make sure I didn’t hit anyone with my car. I bought Plan B regularly for fear I had sex and didn’t remember. But in February 2020, I found myself picking up $300 worth of anti-HIV medication that I did not need. I hit my OCD rock bottom.
Still, no one would know I was suffering, because I could act laid back when I needed to be. I have a loving family and friends, and I’ve been in serious relationships and take care of my dog. I have my own condo and a great job. On the side, I do stand-up comedy and tell self-deprecating jokes about my anxiety. Even though my career is in sales, I hold a master’s degree in social work. I studied OCD and still did nothing about it.
After I took that anti-HIV medication unnecessarily, I knew something had to give.
I made an appointment with a new therapist who specialized in OCD and promised myself I’d tell her the truth. I have been seeing therapists on and off for years, but I’d often lie. See, if I were honest, I’d have to stop these behaviors and the idea of that was too scary—they were my security blanket.
That’s not uncommon. There are actually several reasons a person might lie to their therapist, explains Kelley Kitley, L.C.S.W. The biggest? They’re ashamed or embarrassed by what they did, said, or thought. “With OCD, it’s difficult for patients to say their intrusive thoughts out loud,” she explains. “Even though the patient knows they’re speaking to a trained professional, there is still internal shame of saying it out loud. Keeping it all in, patients can feel very isolated and embarrassed. However, once it’s said out loud, it gets rigorously easier for the patient.”
Not telling the truth is a “protection mechanism,” she adds, which can thwart a person’s progress in therapy. “Some patients might not be ready to go there,” Kitley says. “Some aren’t ready to really make the change and don't want to be held accountable.”
Once I explained all my behaviors to my new therapist and admitted that I never actually put any work into trying to manage my OCD, I felt free. She and I constructed a plan of how we would work together. We decided I would see her twice a week: one session for intensive OCD treatment and one for talk therapy.

Everything was off to a great start, until the pandemic hit.
My therapist and I could no longer meet in person, so we switched to weekly phone calls in April 2020. However, my OCD was minimal at the time because my life wasn’t my life anymore. I wasn’t leaving my apartment, driving, dating, or going out with friends. I felt in control, at least for a moment.
Then, in June, my fear of STDs started to take over my thoughts again—and I spiraled. I emailed my gynecologist numerous questions and spent hours reading about STD symptoms online. I told my therapist I couldn’t stop myself and it was then she felt she couldn’t help me just by talking weekly on the phone. Instead, she recommended intensive outpatient treatment.
I had investigated a similar treatment plan years before, but I had every excuse for why I couldn’t do it. I might have a client event, dinner plans, or a stand-up comedy show. When would I work out? How could I date? But things were different during lockdown. In June 2020, I had nowhere to go: no events, dinners, shows, or dates.
I didn’t even have to leave my couch: The outpatient program was three hours each evening, four days per week, via Zoom. I literally had no excuse not to participate.
The idea of the treatment terrified me, but my OCD terrified me more.
The symptoms were paralyzing, and I wanted them to stop, so I agreed to do the program. For four weeks, I worked with different therapists, participated in group therapy that had an educational component, and practiced exposure response prevention (ERP) therapy.
The International OCD Foundation states that, the exposure in ERP refers to exposing yourself to the thoughts, images, objects and situations that make you anxious and/or start your obsessions. While the response prevention part of ERP refers to making a choice not to do a compulsive behavior once the anxiety or obsessions have been triggered.
So, for example, I had to stop taking pictures of my appliances when I left my apartment. In treatment, I’d write out a worst-case scenario repeatedly: I forgot to turn off my hair straightener, which then started a fire that burned down my building and killed my neighbors.
I hated writing this down. My chest would feel heavy, and my throat would close up. However, after writing it on repeat for an hour, the anxiety started to fade, and I eventually got bored of it. I realized it was just a thought, not a fact, and it had no meaning.
The next step was putting ERP into action. One Friday, I went to my sister’s house for the weekend. As I was leaving my apartment, I started feeling nervous. I had not left my apartment without taking a picture in 15 years. I told myself that my OCD could sit with me, but I wasn’t giving in. I did not take one picture. An elephant of anxiety sat on my chest as I got in my car. I wanted to turn around and go back, but instead, I started driving. About five minutes later, the anxiety was gone.

My life has completely changed since I finished the program.
I am not free from OCD, nor will I ever be—it’s simply how I am wired. The difference now is that I have the tools to help manage it, in addition to my weekly therapy sessions where I’m completely honest and open. I’ve come to realize that when life gets stressful, my OCD will flare up—but instead of letting it take control over me, I’m able to pinpoint it, do ERP exercises, and move on.
It may have taken a pandemic for me to realize it, but if you’re suffering from OCD, the best thing you can do is seek help and tell the truth in therapy. I wasted years of my life suffering over fake fears. I can’t get that time back, but I’m proud of myself for acting when I did and am excited for what the future holds, knowing that my OCD doesn’t control me.
You Might Also Like

