Here’s What Novel Coronavirus Could Do to Your Lungs, According to Doctors

The novel coronavirus, officially named SARS-CoV-2, is often compared to the flu, due to their overlap in symptoms. But when you take a closer look at how this newly discovered virus impacts the body, that comparison doesn’t seem to be totally accurate anymore.
COVID-19, the respiratory illness caused by this coronavirus, seems to have the potential to cause more respiratory distress than the flu. Out of its three symptoms listed by the Centers for Disease Control and Prevention (CDC)—fever, dry cough, and shortness of breath—one seems to set COVID-19 apart from other similar illnesses.
Shortness of breath: The latest to speak publicly about this symptom is former Bachelor star Colton Underwood. The 28-year-old shared an update on his condition on Instagram, and said his “most prominent symptoms” are a cough, night sweats, and shortness of breath. Breathing is “challenging,” Underwood wrote. “The best way to describe it is feeling like I only have access to 20% of my lungs.”
The World Health Organization (WHO) says that COVID-19 can actually cause a range of symptoms—from a sore throat to muscle aches—and the illness varies in severity. But experts believe that, in more advanced cases, this coronavirus can directly damage the lungs, the effects of which may last even after a person has recovered. Here’s what doctors know so far.
What does the novel coronavirus do to your lungs?
“SARS-CoV-2 and influenza are different viruses with different behaviors and sites of attack,” explains Reynold Panettieri, M.D., a lung specialist and vice chancellor for translational medicine and science at Rutgers University. “SARS-CoV-2 is very aggressively attacking the upper airway, throat, sinuses, and mouth cavity as compared to flu. As a consequence, the infectivity is greater.”
Any coronavirus infection starts with your respiratory system via infected droplets, which are released into the air when you cough or sneeze, per the CDC. If you’re close enough to someone who is sick, those droplets can make their way into your body through your eyes, nose, or mouth.
In 80% of patients, the illness that ensues will be mild, per a recent report from the WHO. “Many cases of COVID-19 are going to be an upper respiratory infection that usually spares the lungs,” says infectious disease expert Amesh A. Adalja, M.D., senior scholar at the Johns Hopkins Center for Health Security.
But ultimately, the way in which coronavirus impacts your lungs largely depends on the severity of your infection, Dr. Adalja says. If you’re in a high-risk group, it can even cause life-threatening complications.
Mild infection
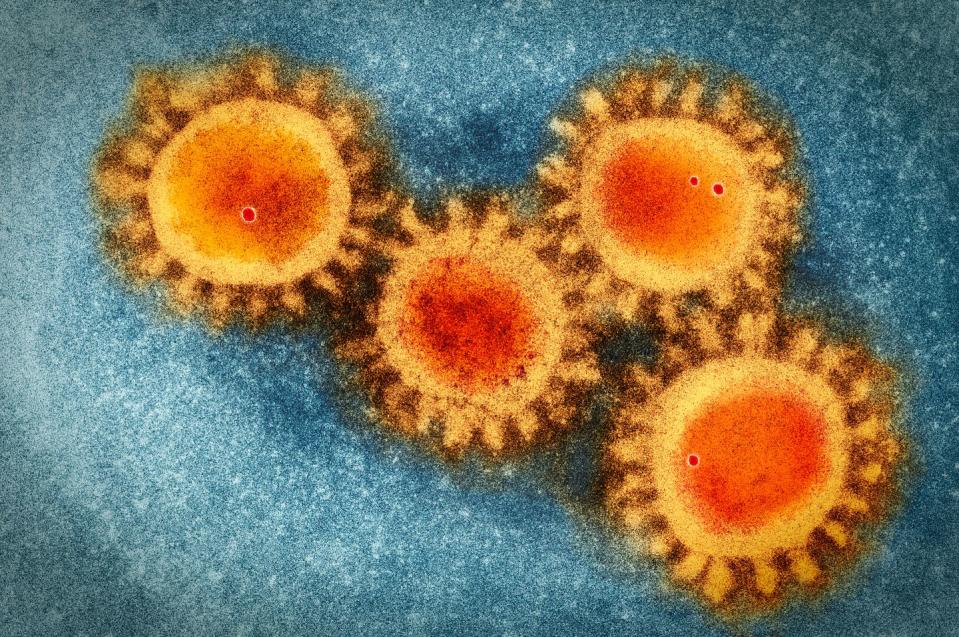
The coronavirus has crown-like spikes on its surface, which help the virus latch onto and hijack healthy cells—say, in the back of your throat or other parts of your upper airway. This causes symptoms “from the neck up—a sore throat, stuffy nose, and a little bit of fever,” says William Schaffner, M.D., an infectious disease specialist and professor at the Vanderbilt University School of Medicine. These patients can often recover on their own at home under self-quarantine.
However, people with mild cases of COVID-19 may not even realize they’re infected, he adds. The incubation period is typically between two and 14 days, meaning someone can carry the virus for up to two weeks before they begin to show any signs of illness.
Moderate infection
“If you have a fever and cough, you already have a moderate illness,” Dr. Schaffner explains. Fortunately, many people impacted with a moderate case of COVID-19 “are being sent home and are doing perfectly well.”
In this stage, the virus has replicated enough to travel down your chest and into the bronchial tubes, “causing inflammation that will result in a dry cough,” Dr. Schaffner says.
Your bronchial tubes lead directly to your lungs from your trachea (a.k.a. windpipe), so they’re a key player in circulating oxygen effectively. When they become irritated or swollen due to inflammation, they have a harder time performing their job well.
Severe to critical infection
When someone has a severe case of COVID-19, the coronavirus leaves the bronchial tubes and gets deep into the lungs, Dr. Schaffner says, impacting “the tissue that’s involved in gas exchange—getting good air in and bad air out.” These patients often have severe shortness of breath and develop pneumonia from the virus itself.
That’s different from the flu, where patients may develop pneumonia as a secondary infection, Dr. Schaffner says. “Unlike other kinds of pneumonia, coronavirus pneumonia tends to affect most or all of the lungs, instead of just certain areas,” he explains.
In severe cases, COVID-19 also has the capacity to cause what’s known as acute respiratory distress syndrome, or ARDS, says Richard Watkins, M.D., infectious disease physician and professor of internal medicine at the Northeast Ohio Medical University.
ARDS is a dangerous and potentially fatal condition that happens when lungs are severely injured, typically by an infection or trauma. In the condition’s earliest stages, small blood vessels in the lungs start to leak fluid into the tiny air sacs responsible for oxygen exchange, which eventually makes it difficult to breathe as the lungs become smaller and stiffer. At this point, your body is likely firing an excessive immune response as it tries to fight the virus, possibly attacking healthy cells in the process, which can “lead to worsening respiratory failure,” Dr. Schaffner says.
Patients with a severe to critical case of COVID-19—often those in high-risk groups, such as the elderly or immunocompromised—“are being admitted to the hospital, may need to be admitted to the intensive care unit, and be put on ventilators,” Dr. Schaffner says. “Often both lungs are affected.”
Can COVID-19 cause lasting lung damage?
In a media briefing earlier this month, Hong Kong doctor Owen Tsang Tak-yin, medical director of the authority’s Infectious Disease Centre at Princess Margaret Hospital, said that doctors have seen about a dozen former coronavirus patients for follow-up appointments. About three of them were unable to do things they had done in the past. “They gasp if they walk a bit more quickly,” Tsang said, per the South China Morning Post. “Some patients might have around a drop of 20 to 30% in lung function [after recovery].”
It’s definitely possible that this novel coronavirus can cause lasting lung damage, Dr. Adalja says. “We know that when an individual has severe pneumonia—irrespective of the cause—they are going to be left with diminished lung function for some time.”
This includes decreased exercise capacity and pulmonary reserve, or the additional air volume your lungs can inhale and exhale at capacity in times of stress. “It may be months or years, it all depends on severity,” Dr. Adalja says.
It’s “unclear” what long-term damage COVID-19 might cause, though, says Dr. Panettieri. “Some apparent long-term consequences are seen in anyone who develops ARDS, but our experience is inadequate to say the lungs are irreparable,” he says. “Collectively, our global experience is only three to four months.”
Dr. Watkins agrees. “We are still in the early stages of the pandemic,” he says, “and don’t yet know if this will be an issue.”
Like what you just read? You’ll love our magazine! Go here to subscribe. Don’t miss a thing by downloading Apple News here and following Prevention. Oh, and we’re on Instagram too.
You Might Also Like

