Not All Forms Of Multiple Sclerosis Have The Same Symptoms
Whether you realize it or not, you likely know someone with multiple sclerosis, since one in every 300 people in the United States has this autoimmune disease. But what you may not realize is not everyone has the same type of MS.
Multiple sclerosis (MS) is a chronic, inflammatory, and neurodegenerative disease that attacks the healthy tissue in your nervous system—particularly your optic nerve, brain, and spinal cord, says Adil Javed, MD, a neurologist and associate professor of neurology at the University of Chicago. The inflammation seen in MS is caused by immune cells which damage neurons and the myelin sheath—a.k.a the fatty tissue that protects your nerves. “The result of that damage is essentially the destruction of these nervous tissues which then leads to disability and symptoms,” explains Dr. Javed.
Meet the experts: Adil Javed, MD, a neurologist and associate professor of neurology at the University of Chicago; Thomas Shoemaker, MD, a neurologist and multiple sclerosis specialist at Rush University Medical Group.
Every MS diagnosis is different, but common symptoms include vision loss or double vision, facial numbness, urgency or inability to urinate, difficulty walking, poor balance, and numbness, weakness, or tingling in the limbs, says Dr. Javed. However, some patients may also experience excessive fatigue, tiredness, lethargy, decreased endurance, short term memory recall, and slow processing speed of information, he adds.
About 1 million people are living with MS in the United States, but it is more common in women than men, with the average age of diagnosis around 30 years old, says Dr. Javed. And while MS has historically been associated as a white or Caucasian disease, it is severely underreported in Black and Hispanic communities. “There is a lot of research going on looking at this minority population of MS patients, and MS prevalence may be just as high if not more than the Caucasian cohort,” he adds.
It’s also worth noting that in 2013, the four types of MS were revised to reflect new research. “The previous progressive-relapsing multiple sclerosis category was dropped,” says Dr. Javed. “We now think of the disease as either relapsing-remitting multiple sclerosis, secondary-progressive multiple sclerosis, or primary-progressive multiple sclerosis, and then there was an introduction of another clear entity [of the disease] called clinically isolated syndrome.”
To help distinguish between the four types of MS, read on to learn the associated symptoms and prognosis, according to experts.
1. Clinically Isolated Syndrome (CIS)
Clinically isolated syndrome (CIS) is the very first manifestation of neurological symptoms caused by inflammation and demyelination (the loss of myelin) in the central nervous system, says Thomas Shoemaker, MD, a neurologist and multiple sclerosis specialist at Rush University Medical Group. Symptoms persist for at least 24 hours and cannot be caused by anything else such as a fever or infection, he adds.
The most typical symptoms are painful vision loss in one eye, vertigo, inability to control your eyes or face, and/or sensory loss in one or both extremities with the sensation usually coming up from your feet. “These symptoms are episodic and usually last for a period of days, or sometimes weeks, and then they will remit and go away to a certain extent,” explains Dr. Shoemaker. “Most people completely recover, especially with their first relapse, and then go for a period of time without any symptoms.”
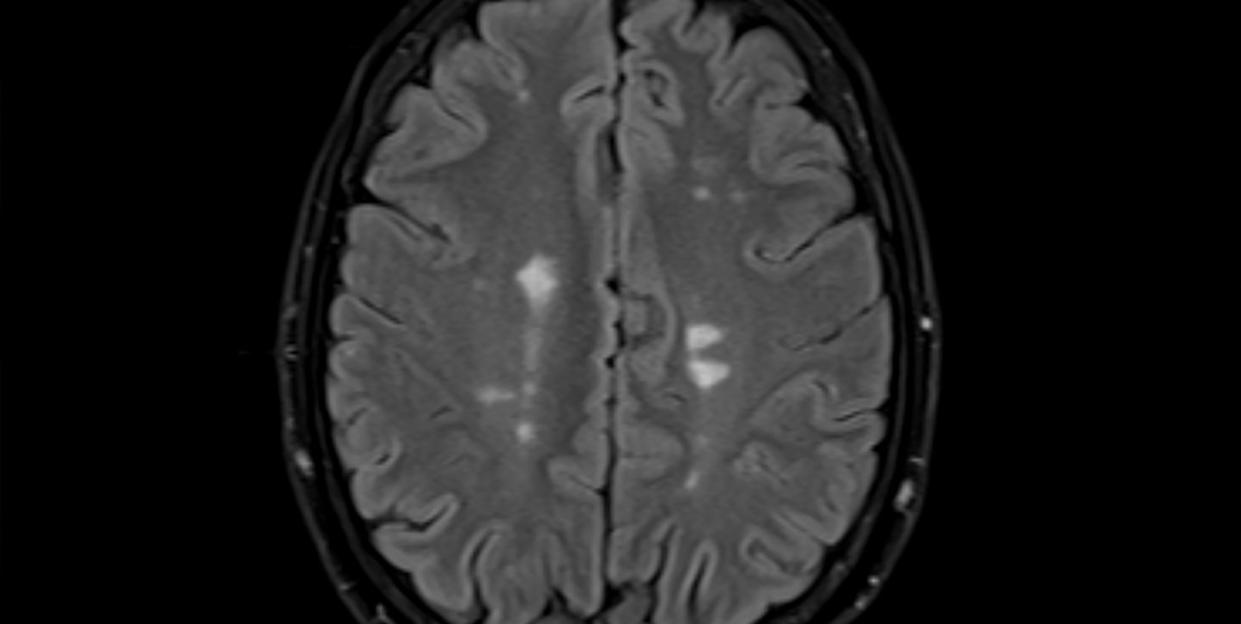
Patients with CIS may have only one attack and never develop MS, but another relapse months or years later is possible. “If you do have a relapse, it tends to be associated with changes to a brain or spine MRI which will show new, active lesions,” says Dr. Shoemaker. If CIS is accompanied by changes to the brain on an MRI, a person is at risk for another episode and a MS diagnosis, he explains.
2. Relapsing-Remitting MS (RRMS)
This type of MS is the most common disease course, making up 85 to 90 percent of the MS population, says Dr. Shoemaker. “The classic MS patient is going to be a relapsing-remitting patient, and it’s more than likely a young woman of reproductive age,” he explains. “Men still get relapsing MS, but it is female predominant with a three to one female to male ratio.”
RRMS symptoms are typically defined attacks or “relapses” that worsen neurological functioning for days or months at a time, with the most common symptoms including extreme fatigue or weakness, impaired vision, spasticity or stiffness in the limbs, numbness in the feet, bowel and bladder problems, depression, short term memory loss, and difficulty thinking clearly. “Most people completely recover [from these symptoms], especially with their first relapse, and then they'll go for a period of time without having any symptoms,” explains Dr. Shoemaker. “That's the relapse and then the remission.”
And while the attack is usually followed by a period of remission where symptoms disappear, it’s possible for the same or new symptoms to occur with another relapse. “The course [of symptoms] or progression of the disease can be altered, depending on how early the diagnosis is made, and how early the treatment begins,” says Dr. Javed. “Prognosis is highly dependent on when you catch the disease, and how quickly you can get the patient on board with treatment.”
Treatment options include oral or intravenous medications which can slow disease worsening and/or reduce the number of relapses, but physical therapy, consistent exercises, healthy diet, weight management, and regular sleep can also help manage symptoms, adds Dr. Javed.
3. Secondary-Progressive MS (SPMS)
Secondary-progressive MS follows an initial relapsing-remitting disease course and is often diagnosed after at least a year of MS-related relapsing symptoms, says Dr. Shoemaker. In other words, SPMS is a second phase of the disease. “SPMS is the worsening of neurologic functioning that predominantly manifests as gait or walking impairment,” explains Dr Shoemaker. “This progression is the state of a slow, steady, worsening of symptoms over a sustained period of time, in the absence of a relapse.”
The progressive course of disability varies on the person, but there is usually a slow decline in terms of functioning and ability, says Dr. Javed. However, SPMS can be treated if the disease is still active. “If disease activity is detected at the secondary-progressive stage and that activity is defined with new lesions on an MRI, then those patients do fairly well with treatment,” he says. A doctor may suggest medications called disease-modifying drugs that are similarly used during relapsing stages of MS to help prevent and minimize further relapses.
4. Primary-Progressive MS (PPMS)
You may have heard primary-progressive MS referred to as progressive-relapsing MS, but this terminology is no longer used, says Dr. Shoemaker. In PPMS, the disease gradually worsens from the time of first presentation and there are no relapses, he says. Neurological functioning decreases with consistent symptoms and there is little to no improvement or change. “If someone is having a relapse, they are not in a progressive phase of MS and they are still in a relapsing phase,” he explains.
PPMS makes up about 15 percent of MS patients, with the median age between 45- to 55-years old, and is equally common in men and women, adds Dr. Javed. And while there are no new or well-defined attacks of symptoms, there is a slow decline in ability leading to physical disability earlier in life, he says. There are unfortunately very few treatments for PPMS, but there is currently one FDA-approved IV infusion treatment that is administered every six months.
You Might Also Like

