Norton emerging as a top program for new Alzheimer's drug. What it means for patients

The week before Pam Jeffries began treatment, she spent eight days at sea on an unforgettable cruise to the Southern Caribbean.
But by the time she settled into the doctor's office for her first dose of Lecanemab, she couldn't remember she’d ever stepped onto the ship at all.
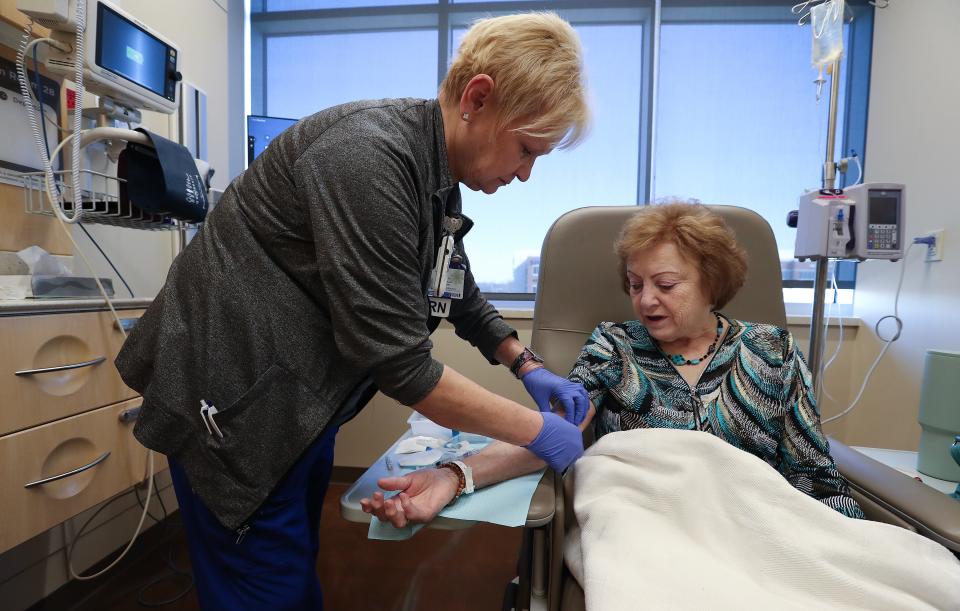
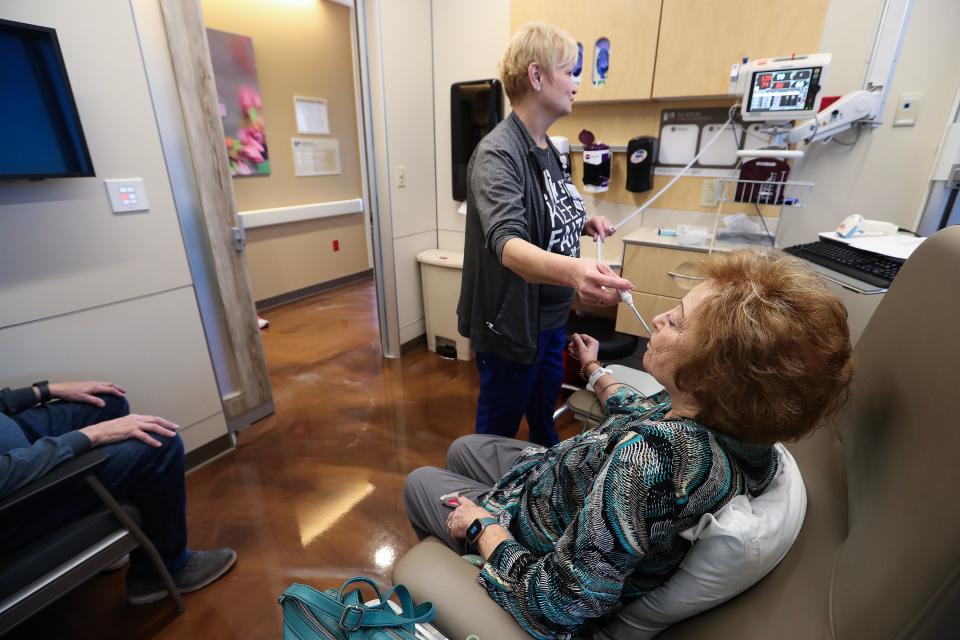
Jeffries is one of dozens of patients in the Louisville area who is taking a new ground-breaking drug designed to slow down the progression of Alzheimer’s disease. The twice-a-month infusion through Norton Neuroscience Institute isn’t a cure, but rather, a way for her to hold on to the memories she still has. It won't bring back the memory of that cruise, but early studies show that Lecanemab can slow the devastating disease's progression by 30%.
The early results are encouraging overall, said Dr. Greg Cooper the chief of adult neurology and director of the Memory Center at Norton Neuroscience Institute.
For some patients, like Pam, memory loss symptoms have seemingly steadied.
More: Here are 5 things to know about Lecanemab, the new Alzheimer’s treatment
The Food and Drug Administration approved the drug in early 2023, and Pam made Kentucky medical history in August when she became the first patient to receive an infusion. Now six months later, 68 of Norton Neuroscience Institute's patients have had their first treatment, and the Louisville-based health system has emerged as one of the top programs in the nation for administering Lecanemab. There are another 30 or so memory loss patients who are on course to begin the process, too.
Since last summer, Rick Jeffries has watched his wife closely and lovingly as the medicine tries to shrink an abnormality in her brain. Just a couple of weeks ago, Pam, 74, flipped through an old school yearbook with childhood friends and swapped stories about teenage love and growing up in the 1960s. But some days, she can't remember which side of the bed she sleeps on or where she usually sits at the kitchen table.
Rick knows he can’t wish for her memory to come back. But with this medicine, he can only hope it doesn’t fade further.
'Today is a good day'

In the days leading up to Pam’s six-month evaluation after beginning the infusions, Rick felt a noticeable pit in his stomach.
Her short-term memory is mostly depleted. Pam can dress herself, prepare meals, and mostly go about her day, but just like she forgot about that cruise, she hasn't remembered that she is battling memory loss.
Experts believe Alzheimer's disease is caused by an abnormal protein, known as beta amyloid, in the brain that triggers the events that lead to dementia, said Dr. Greg Cooper, the chief of adult neurology and director of the Memory Center at Norton Neuroscience Institute. Once that trigger is removed using Lecanemab, the progression of the disease can slow down.
At the same time, the medicine only helps patients with mild cognitive impairment, and Rick doesn’t like to think about what may happen once his wife crosses into the moderate zone.
“You can always progress out of the treatment, and I'm always fearful that when we’re coming in and (her memory) has deteriorated,” Rick told Cooper during the appointment.
“That doesn’t mean it can’t, but today is a good day,” Cooper assured him.

Remarkably, Pam had scored a point higher on a memory test, known as the mini-mental state exam, than she did before the infusions started. Without the treatment, Cooper expects she would have scored two to three points lower than she did.
There could be many reasons for that, Cooper said, even as simple as him catching her on a good day. But with that positive score, and as long as she manages most of her day-to-day tasks without causing too much frustration, she’s still in that early onset bracket.
Pam, however, could be on this drug for the rest of her life, or until her memory depletes past the point where the drug is effective. Even if Lecanemab knocks out that trigger in her brain entirely, Cooper said, some experts would argue in favor of continuing the infusions to keep it from coming back. The treatment is so new that there are still several schools of thought around it, which leaves plenty of uncertainty for patients and families.
One abundantly clear thing is the sooner patients with that protein start on it, the better it will work.
'I know I've got it'

Noticing cognitive impairment early, though, isn’t necessarily easy. So often there is a stigma associated with the earliest stages of memory loss. Families can blame old age or chalk up lapses to distractions. Denial is common.
But for Bobbie West, 75, it was quite the opposite. She could feel her memory slipping.
Her late sister had Lewy Body Dementia that caused haunting hallucinations. The small memory lapses and names Bobbie just couldn’t bring to the tip of her tongue weren’t that extreme, but she began to notice behaviors in herself that reminded her of her sister.
Rather than wait it out, she called a doctor.
When Bobbie passed a memory test, she took another one.
“I know I’ve got it; I know I’ve got it,” she remembers telling her husband, Ralph.
She shuffled through physicians and tests for months, until Dr. Rachel Hart at the Norton Neuroscience Institute recognized the same struggle in her that Bobbie overwhelmingly sensed in herself. When tests showed she had the markers for Alzheimer’s, she was almost relieved. At least now, she had an answer to why she was feeling as lost as she did.
The timing was flawless — about a week after her diagnosis, Lecanemab was approved by the FDA.
Bobbie became the sixth patient at Norton to start infusions. After the first two, the couple didn’t really notice a change, and frankly, knowing the drug's limitations they didn't expect one. But for whatever reason, after the third dose, Bobbie felt a fog lift from her. She still struggled with her memory, but overall, her sense of awareness returned.
“I just really felt like my old self by the end of the week,” she remembered.
“She still has a lot of issues, but it hasn’t gotten worse,” Ralph explained. “But she seemed, just to be a lot more alert, and she could remember things a little bit better.”
That upswing hasn’t kept them from planning ahead. They’ve looked into nursing homes, in case it gets to that point, and adjusted their financials accordingly.
Both Ralph and Bobbie participate in support groups for patients and caregivers with mild cognitive impairment, and it helps them in a couple of ways. It gives the Wests the assurance they’re not alone in some of the hiccups they experience, but it also makes them grateful for the hand they’ve been dealt.
They caught Bobbie’s condition before it truly whittled away at her short-term memory.
Now, they’ve got a head start in this program that most families could only dream about.
'What did we come here for?'
While Rick hasn’t noticed that same alertness in Pam as Ralph sees in Bobbie, he has caught flickers of success.
When the memory loss first hit, Pam stopped working on her longtime writing projects. She’s been published before, and over the years, she’s put a lot of energy into writing her memoir. In the past few months, Rick has found her in her old office reading her stories on the computer. Before the infusion, she never had any interest in doing that.
At the same time, they’ve spent hours on more than one occasion searching for her hearing aids once she places them down. Once she took off all her jewelry before they left the house for an MRI, and when they returned home, Rick realized with horror he hadn’t watched where she put it.
While evaluating patients like Pam, Cooper relies on the mini-mental state exam, but he also pays close attention to what Rick relays about their life at home. Based on everything he saw in that six-month evaluation, he was confident the protein in her brain was shrinking.
“Is there anything else we need to talk about?” Cooper asked as the evaluation slipped from memory loss to a little banter about allegiances to Cards and Cats.
“What did we come here for?” Pam asked.
At the moment, it wasn’t clear whether she was joking or the context of the appointment had been lost in the latest basketball scores.
“Just to chat,” the doctor said, kindly.
Some days Pam seems just ever so slightly better, Rick says, and in other moments, he frets her memory is getting worse. It’s hard to know whether she really remembers things when the family prods her, or if she’s just figured out how to nod along and play the game.
At the very least, Pam’s mild cognitive impairment hasn’t taken her sense of humor.
As part of the memory evaluation, Cooper gave her three words to remember at the beginning of the appointment: ball, flag and tree.
When Pam first began struggling with her memory, Rick could usually get her to remember the word tests with hints and clues. That hasn't worked in a while.
But this time, Pam came up with her own answer at the end of the appointment.
“I am beautiful,” she said.
Reach Courier-Journal Features Columnist Maggie Menderski at mmenderski@courier-journal.com.
This article originally appeared on Louisville Courier Journal: Louisville Norton Hospital top program for Alzheimer's drug Lecanemab

