Never-before-seen antibodies can target many flu viruses
A newly discovered class of antibodies in human blood can neutralize different types of the flu virus and could be key to the development of broadly protective vaccines against the seasonal viruses, scientists say.
Circulating flu viruses constantly mutate, so "we need annual influenza virus vaccines to keep pace with continuing viral evolution," the researchers behind the discovery said in a statement. "Our work suggests that the barriers to eliciting more broadly protective immunity may be surprisingly low," they said.
There are four types of flu virus, known as influenza A, B, C and D, with A and B being responsible for the seasonal flu epidemics in the U.S. every year.
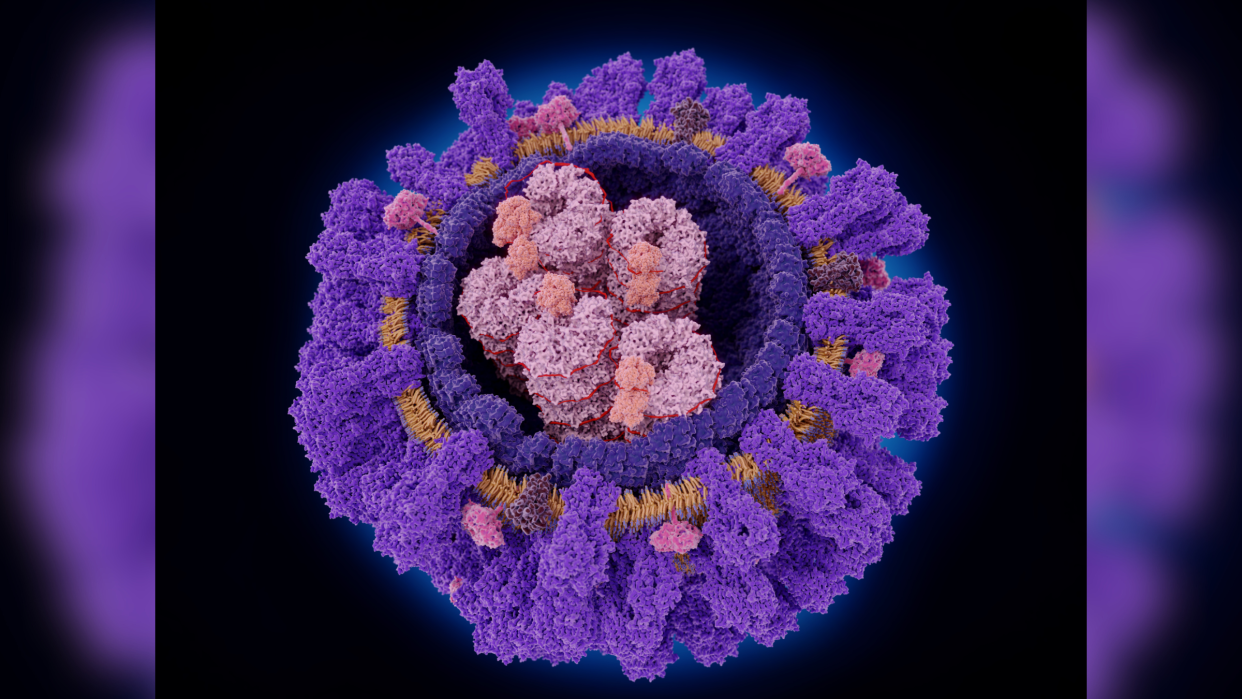
Influenza A comes in many subtypes whose differences lie in two proteins that the virus uses to infect our cells: hemagglutinin (H) and neuraminidase (N). For example, H1N1 and H3N2 are subtypes of influenza A that routinely infect people.
Within each subtype are different "strains" that constantly tweak their genetic code. For example, a strain of H1N1 is currently the dominant virus causing flu in the U.S. Influenza B, meanwhile, is divided into two lineages — Yamagata and Victoria — and is typically responsible for a much smaller proportion of flu cases.
Making effective flu shots relies on harnessing the protective power of antibodies — immune proteins that attack invading pathogens — but the virus' ability to quickly mutate makes this challenging. Flu vaccines prime the immune system to produce specific antibodies that latch onto a flu virus and prevent it from infecting cells after it invades the body. However, these vaccines are formulated to target specific strains, and because those strains mutate year over year, people then need a new flu shot each year to keep up.
Related: 'Long flu' is real, and we've likely 'ignored it for a long time'
In the new study, published Thursday (Dec. 21) in the journal PLOS Biology, scientists described a newfound class of antibodies in human blood samples that target multiple forms of the influenza A virus.
The research was conducted only in the lab, so the scientists aren't sure exactly how these antibodies contribute to the body's flu shot response. However, one day, these antibodies could be used to develop vaccines that are more effective at protecting people from multiple strains of flu at the same time.
To guard against influenza A, conventional flu vaccines usually prompt the immune system to produce antibodies against the H protein on the surface of the virus. Antibodies have previously been discovered that target two main types of hemagglutinin, called H1 and H3, at the same time. However, they can only do this if there is a specific mutation in H1, namely the insertion of an amino acid in the outer edge of the protein that binds to a receptor on the outside of our cells. This consequently limits the antibodies' efficacy against different flavors of flu virus.
Through lab experiments, the study authors identified antibodies that are abundant in human blood and can bind to certain H1 and H3 strains of influenza A, whether or not this hemagglutinin mutation is present. This means that they'd theoretically be able to provide broad protection against both subtypes of virus, potentially even as circulating strains mutate over time.
The authors also looked at how well these antibodies targeted strains of H1 and H3 that have circulated in the past. The antibodies reacted with H3 strains from the late 1980s to late 1990s and H1 strains from the early 2000s through to 2015.
This suggests the patients whose blood was sampled originally made the antibodies in response to H3 strains of the virus. Then, after a later exposure to H1 strains at a later date through either infection or vaccination, the antibodies became primed to target H1 as well.
RELATED STORIES
—When should you get a flu shot? What to know for the 2023-2024 flu season
—Could we ever eradicate the flu?
—Skeletons from 1918 flu dispel myth that young, healthy adults were more vulnerable to the virus
These findings may have important applications for future vaccine design.
"Given the right series of influenza virus exposures/vaccinations, it is possible for humans to mount robust antibody responses that neutralize divergent H1N1 and H3N2 viruses, opening new avenues to design improved vaccines," the authors said in the statement.
In other words, there may be a way to ensure vaccines trigger the production of these broad-acting antibodies, to ensure the shots guard against both subtypes of the virus equally well.
Ever wonder why some people build muscle more easily than others or why freckles come out in the sun? Send us your questions about how the human body works to community@livescience.com with the subject line "Health Desk Q," and you may see your question answered on the website!

