How Much Should You Care About Inflammation?
If you're a healthy adult with no inflammatory conditions, what does it mean to control inflammation, and does it really matter for your long-term health?
Fact checked by Nick Blackmer
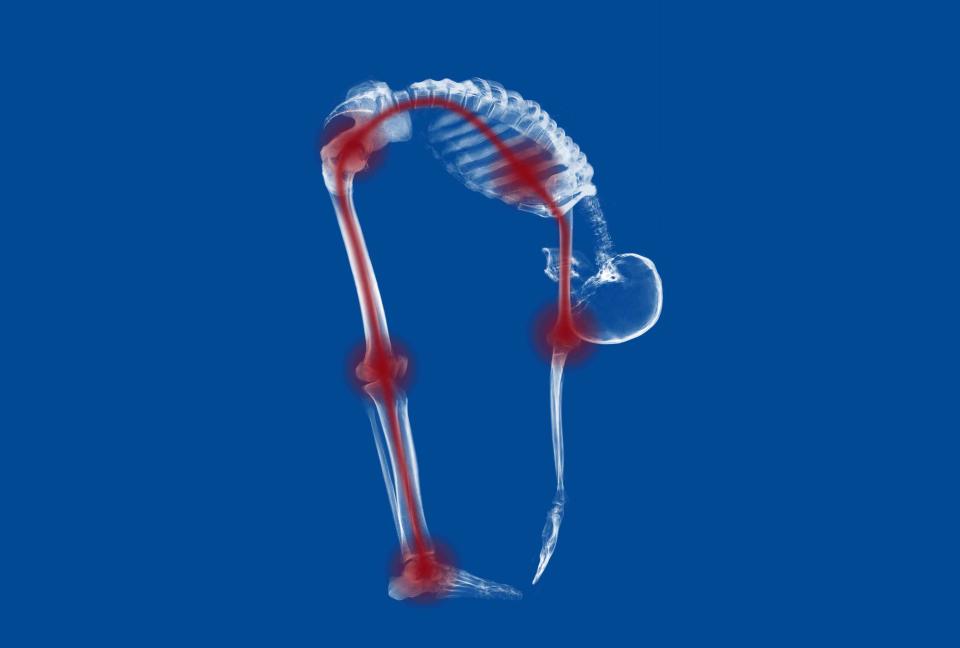
Inflammation gets a bad rap, and understandably so. It’s connected to a host of health problems, and more than half of all deaths in the world are attributable to inflammation-related diseases.
It is, however, an essential part of keeping the body healthy. Anyone who has ever sprained an ankle, been stung by a bee, or overcome a cold has experienced inflammation. The swelling and tenderness you may experience in an inflamed area is a sign that a small army of immune cells has rushed to the scene to flush out unwanted pathogens or heal injuries.
But sometimes, an inflammatory response doesn’t subside after the body has been healed. A constant attack of immune cells can damage tissues and blood, which flows through just about every part of the body. Over time, persistent low-grade inflammation can contribute to conditions including dementia, cancer, heart disease, type 2 diabetes, skin conditions, and more.
There are many reasons why someone might experience chronic inflammation. For example, it can arise after a traumatic injury, alongside a chronic disease, or as a result of smoking.
For most healthy people who have not been diagnosed with an inflammatory disorder, there may be no way to know whether you’re living with low-grade chronic inflammation. But taking steps to protect your heart health and bolster your immune system can help stave off the effects of aging and several serious health conditions over time.
Related: Inflammation: Types, Signs, Causes, and Treatment
When Does Inflammation Become Problematic?
Inflammation is like a flame, according to Sonia Sharma, PhD, associate professor in the Center for Autoimmunity and Inflammation at the La Jolla Institute for Immunology in California.
It typically burns low and gets turned up when there is a wound to heal, a pathogen to fight, or a cancerous growth to quell. It might burn on high for a brief time to fight an acute injury. But when a low or medium flame smolders for a long time, meaning several years, the constant activity of immune cells can damage cells in the intestine and to the veins and arteries that carry blood throughout the body.
How Long Does it Take for Inflammation to Cause Health Issues?
There are no clear-cut human studies about how long the buildup of inflammatory biomarkers takes before contributing to disease. But it's a process that takes years, according to existing research. For example, in studies of diets considered to be “pro-inflammatory,” participants were twice as likely to be diagnosed with prostate cancer and 20% more likely to be diagnosed with colorectal cancer within about 12 years. And in a study evaluating a modest increase in ultraprocessed food consumption (10%), participants’ all-cause mortality risk increased by 14% over seven years.
“In the immune system, you really want targeted fire, like drones. It should go to the right place,” Sharma told Verywell.
In cases of chronic inflammation, however, that immune response is diffuse. People with inflammatory bowel disease or rheumatoid arthritis, for instance, live with chronic inflammation that damages their gastrointestinal tract and nervous system, respectively.
Chronic inflammation can lead to atherosclerotic disease (hardening or thickening of arteries), which can increase the risk of heart attack, strokes, and cancer. These health problems can be silent for a long time before causing symptoms serious enough to lead to a diagnosis.
Related: The Link Between Inflammation and Heart Disease
Because blood runs through every tissue and organ system, damage to the vascular system can affect the whole body. That includes the brain, which may lead to neurodegenerative diseases like vascular dementia, Alzheimer’s, and other forms of dementia.
Cancer and inflammation also tend to go hand-in-hand, though scientists are still probing why that is. Research so far suggests that sites of chronic inflammation provide an environment that promotes the growth of cancer cells.
For most healthy people, some degree of harmful environmental exposures and eating occasional ultra-processed foods are unlikely to cause immediate and substantial inflammation. Over time, however, that drip can turn into a flood, Sharma said.
Taking steps to counter inflammation can curtail inflammatory problems from snowballing.
Can You Test for Inflammation?
When healthcare providers are monitoring someone for an inflammatory condition or suspect harmful chronic inflammation, there are a couple of tests they can use. These include an erythrocyte sedimentation rate test, which measures how quickly red blood cells settle in a test tube, and a C-reactive protein test, which looks for a protein produced in the liver when inflammation is present.
Some companies sell direct-to-consumer inflammation tests. But those tests are not part of routine medical care and expert guidelines don’t recommend them, even for most people with cardiac risk.
Do Anti-Inflammatory Diets Really Work?
Foods high in saturated fat, trans fat, alcohol, and refined sugar can also mess with the gut microbiome and trigger inflammatory responses.
Scientists have long suspected that some fats can trigger immune responses that cause inflammation.
But not all fats are harmful. In recent decades, Sharma and other researchers have come to appreciate the anti-inflammatory protective benefits of polyunsaturated fats. Those healthy fats occur naturally in foods including fatty fish and fish oil, olive oil, and avocados.
“Choosing foods rich in polyunsaturated fats compared to trans fats or saturated fats is a good choice and not always immediately thought of when we think of anti-inflammatory diet,” Sharma said.
Meanwhile, some foods are widely understood to have anti-inflammatory properties. Omega-3 fatty acids, which are found in some fatty fish and seeds, and flavonoids, a compound abundant in leafy green vegetables, berries, and many other fruits and vegetables, help to resolve inflammation by interacting with certain genes. Eating oat bran and whole grains—and avoiding white flour and other refined grains—can also tamp down inflammation and decrease the risk of related conditions.
It’s not known exactly how much an anti-inflammatory diet tamps down inflammation nor how much of certain food items someone should eat to see the benefits, Sharma said. While no study definitely shows the Mediterranean diet, for example, is anti-inflammatory, scientists generally agree that the habit of eating lots of fruits and vegetables and few or no ultra-processed foods is a good idea.
In addition to what you eat, “total calorie intake is important,” said Jeffrey Hasday, MD, a physician at the University of Maryland Medical Center and division chief of pulmonary and critical care medicine at the University of Maryland School of Medicine.
There is, he said, an “epidemic of obesity and type 2 diabetes” in the U.S. Excess fat can increase the production of certain immune cells and affect insulin resistance, like heart disease and cancer. Some research suggests that obesity is pro-inflammatory in part because it disrupts the balance of microbes in the gut.
What About Anti-Inflammatory Supplements?
Anti-inflammatory foods tend to be high in antioxidants—compounds that can fight harmful free radical chemicals that can damage cells and increase inflammation.
There are hundreds of substances that act as antioxidants, including vitamin C, vitamin E, and beta-carotene.
While many of these compounds can be taken as supplements, Hasday said that receiving these nutrients through food tends to be more effective than taking the chemical isolates.
“Chemicals in certain foods have been shown to exert anti-inflammatory effects, including flavonoids and omega-3 fatty acids, but they are much less effective when ingested as supplements rather than in foods such as leafy vegetables, berries, and fatty fish,” he said.
Plus, the Food and Drug Administration (FDA) doesn’t regulate supplements. That means companies can sell supplements and market them as “anti-inflammatory” without first proving they are safe and effective.
Related: Natural Ways to Fight Inflammation
Does Exercise Reduce Inflammation?
While exercise is not as directly linked to inflammation control as factors like diet and smoking, research has long established moderate and long-term exercise as one of the best ways to bolster heart health and improve immunity.
“We know that exercise is heart healthy. And when I think heart health, I think vascular health, and I think systemic health,” Sharma said. “I do believe, fundamentally, that long-term vascular health is protective against certain chronic age-related inflammatory conditions.”
High-intensity exercise can hinder immune function, which can cause injury or chronic inflammation over time. But when people exercise with moderate intensity or vigorously, but give themselves plenty of rest time, they tend to see immunity benefits.
What Role Do Environment and Genetics Play?
Sometimes, a person’s risk for chronic inflammation is innate. Some genes can help direct an inflammatory response by turning on the immune system or switching off certain anti-inflammatory processes.
Sharma said there are at least 30 vasculitis syndromes—rare conditions that damage blood vessels through inflammation—that are caused by single gene mutations and can lead to systemic inflammation.
As personalized and precision medicine improves, scientists will better understand which genetic changes control inflammatory conditions and how to target them.
The environment in which a person lives can also increase their inflammatory response.
Breathing in smoke of any sort can cause inflammation. For instance, cigarette smoke contains several toxins that can impair immunity and wildfire smoke carries particles so small they can be absorbed through the lungs into the bloodstream, where they irritate blood vessels.
Disturbed sleep, isolation, and chronic stress also increase a person’s risk of developing chronic inflammation.
Is It Possible to Prevent Chronic Inflammation?
Some of the most common anti-inflammatory medications, such as IL-16 and TNF inhibitors for arthritis, can make patients more susceptible to infection, Sharma said.
If an individual can make dietary and behavioral choices so that they can avoid ever having to take such a medication, Sharma said, they should strive to do so.
When a genetic mutation or high levels of certain environmental exposures are to blame for an inflammatory response, diet is unlikely to make a meaningful difference, Sharma said. But aiming for a diet and lifestyle that keeps your immune system humming could only be beneficial.
“It’s a beguiling question: ‘Can we make certain tweaks to our diet and lower our baseline anti-inflammatory state over a long time to protect us from these inflammatory diseases?’” Sharma said. “Over time, paying attention to these anti-inflammatory factors might just help you.”
Read the original article on Verywell Health.

