How Is MRSA Diagnosed?
Rodolfo Parulan Jr. / Getty Images
Medically reviewed by Ronald Lubelchek, MD
Methicillin-resistant Staphylococcus aureus (MRSA) infection is caused by a type of Staphylococcus (or “staph”) bacteria. What makes MRSA problematic is that it is resistant to certain antibiotics, namely methicillin. Staph bacteria are very commonly found on the skin, but MRSA can affect the skin, lungs, bones, and joints, sometimes spreading to the blood or even the heart. This infection can present as a skin rash or wound, heavy cough, rapid breathing, fever, chills, and inflammation and swelling in the joints or bones.
Alongside your medical history and assessment of symptoms, several tests help providers diagnose MRSA and assess its spread. We'll discuss these tests, what healthcare providers are looking for, and other conditions that they have to rule out to detect MRSA infection.
Medical History
In order to diagnose MRSA infection, healthcare providers will first assess any impacted areas and ask about your symptoms, medical history, and medications. In particular, they look for risk factors for this condition, which include:
Previous (especially recent) or current hospitalization
Admission to the intensive care unit (ICU)
Recent use of antibiotics
Surgery or other invasive procedures
Human immunodeficiency virus (HIV) infection
Residency in a nursing home
Open wounds
Hemodialysis (a procedure that cleans out blood when there's kidney failure)
Long-term use of a catheter into central, major veins (central venous access) or for urination
Physical Examination
Initial evaluation of any affected areas is also a big part of diagnosis. In fact, practice guidelines note that if MRSA infection is suspected, antibiotic treatment may be called for even before the results are confirmed by laboratory evaluation.
Alongside standard measures of health status, such as blood pressure and heart rate, providers will examine:
Any skin symptoms
How your lungs are functioning
Bone or joint pain symptoms
Presence of fever or other signs of broader infection
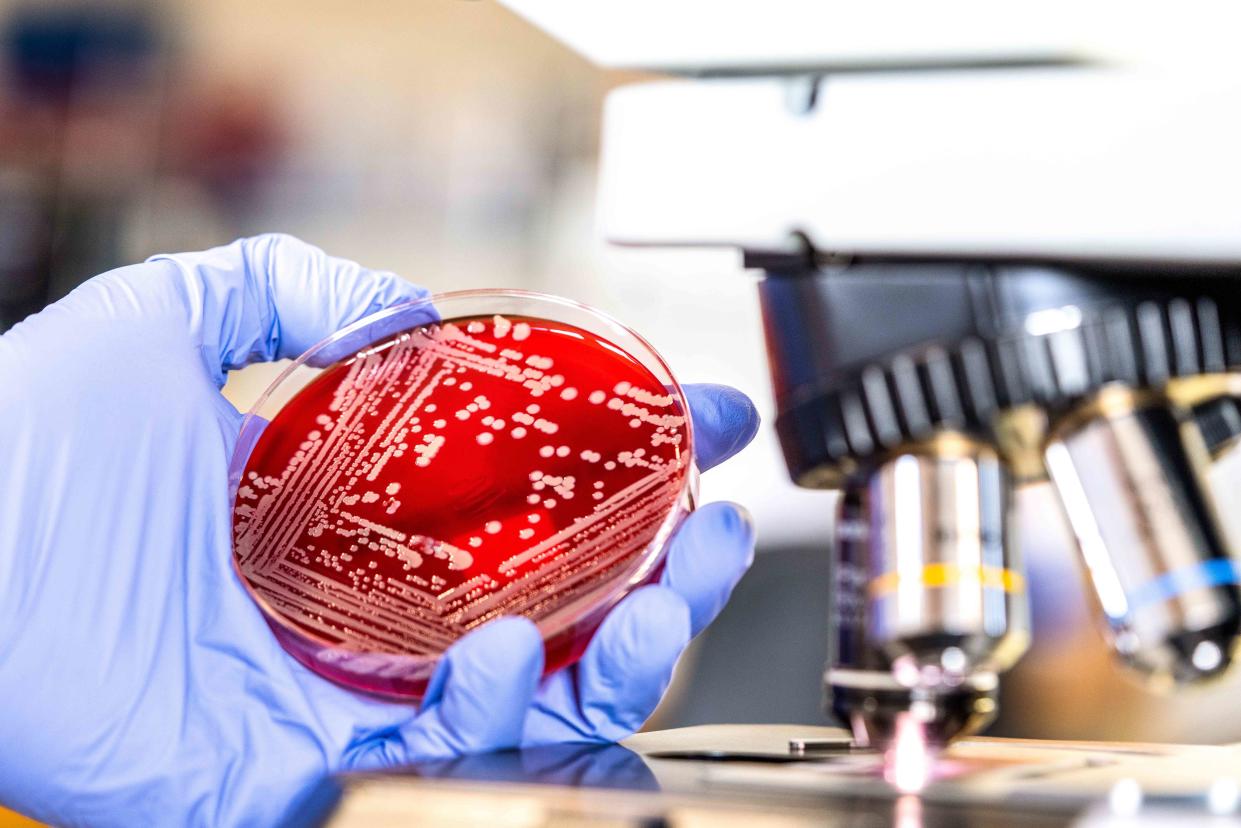
MRSA Culture
Laboratory evaluation of a culture is used to confirm a MRSA infection and is helpful for determining what type of antibiotic to prescribe. This involves laboratory examination of samples taken from different parts of the body. These include:
Wound sample: If the MRSA infection is believed to be associated with an infected wound, the provider will use a swab to collect a sample for laboratory evaluation.
Nasal swap: Staph bacteria can also be detected in a sample of your sputum (spit), which is collected by swabbing the inside of your nasal passages.
Urine test: Bacteria can also be detected in the urine; you’ll be asked to provide a sample for clinical evaluation.
Typically, it takes 24 to 48 hours to test these samples, though a new rapid nasal swab test, the cobas vivoDx MRSA test, yields results in five hours.
Several bacteria culture tests of these samples are used to either confirm the case or rule out other potential causes of the infection. Primarily, MRSA is detected in a lab by using combination of tests to detect bacterial growth and tests to identify antibiotic resistance. In addition, polymerase chain reaction (PCR) tests (which are used to detect COVID-19) are used to rule out other causes, though they can't be used to confirm if you have MRSA.
Imaging
If a MRSA infection is detected and suspected to have spread to your lungs, bones, or joints, additional screening is needed. Primarily, this work is done using imaging techniques, which allow healthcare providers to assess if the bacteria has spread to these areas and how much. This greatly influences the course of treatment.
Commonly used approaches for MRSA include:
X-ray: This relies on radiation to produce images, which are used to see signs of MRSA infection in the lungs or bones
Computerized tomography (CT) scan: CT scans rely on multiple X-rays from multiple angles to produce three-dimensional images of potentially affected areas.
Magnetic resonance imaging (MRI): This type of imaging relies on magnetic fields and radio waves to produce detailed, three-dimensional images.
Echocardiogram: Since MRSA can spread to the heart (known as MRSA endocarditis), echocardiograms (ECG or EKG) rely on sound waves to track blood flow and its interior structure.
Screening for Related Conditions
A major challenge of a MRSA diagnosis is ruling out other conditions that can cause similar symptoms. Your healthcare provider may need to perform testing to ensure you have MRSA and not other conditions that can resemble this infection, including:
Chemical burn
Kawasaki disease, a vein disease that commonly affects children under the age of five
Leptospirosis, or an infection spread through contact with urine
Pediatric endocarditis, or an infection of the heart valves that occurs in children
Pediatric osteomyelitis, or bone swelling in children
Juvenile arthritis, or arthritis in children
Comorbid Conditions
A wide range of conditions are associated with MRSA infection, especially because many cases are acquired in the hospital. Additional screening and testing may be needed to detect these diseases. These include:
HIV/AIDS: Because HIV attacks the immune system, those with this acquired sexually transmitted infection are more likely to develop MRSA infection. Blood tests may be performed to screen for this condition.
Cardiovascular disease (CVD): Conditions that affect the health of the heart, arteries, and vessels are seen at higher rates with MRSA infection. MRSA diagnosis may prompt screening for stroke, heart failure, and peripheral vascular disease (a narrowing of arteries), among others.
Cancer: Cancer—as well as the treatments for it—can significantly impact immune function, making patients more susceptible to MRSA infection. In suspected cases, blood tests, biopsy, or other assessments may be used to screen for the condition.
Diabetes: Diabetes, an inability of the body to digest sugars, can also significantly affect the immune system; as a result, MRSA infection and this condition often go hand in hand. Blood tests may be called for to screen for this condition.
Chronic obstructive pulmonary disease (COPD): COPD is a set of conditions that affect breathing, such as emphysema and bronchitis; this makes the lungs more susceptible to MRSA infection.
Systemic lupus erythematosus (lupus): Systemic lupus erythematosus (SLE) is an autoimmune disorder, in which the immune system attacks organs and tissues in the body, making patients more susceptible to infection. In one study, about 11.6% of those with SLE also had MRSA infection, so X-rays, lab tests, and other assessments may be needed.
Rheumatoid arthritis: This is joint inflammation due to an autoimmune disorder; both this condition and the treatments for it can affect immune function, raising the risk of MRSA infection.
A Quick Review
Methicillin-resistant Staphylococcus aureus (MRSA) infection is a disease caused by a strain of Staphylococcus (or "staph") bacteria that's resistant to certain antibiotics. MRSA is often acquired in hospital or clinical settings, though it can be spread anywhere.
Diagnosis primarily involves a combination of physical assessment and laboratory evaluation of blood, wound, or other samples from the body. If the MRSA infection has spread to the bones, joints, or heart, healthcare providers may call for imaging techniques, such as X-ray or CT scan, to evaluate affected areas. Additional tests may also be called for to detect associated conditions, such as diabetes, cancer, rheumatoid arthritis, and others.
For more Health news, make sure to sign up for our newsletter!
Read the original article on Health.

