Migraine vs. Headache: Treating the Pain

Tatiana Maksimova / Getty Images
Medically reviewed by Smita Patel, MD
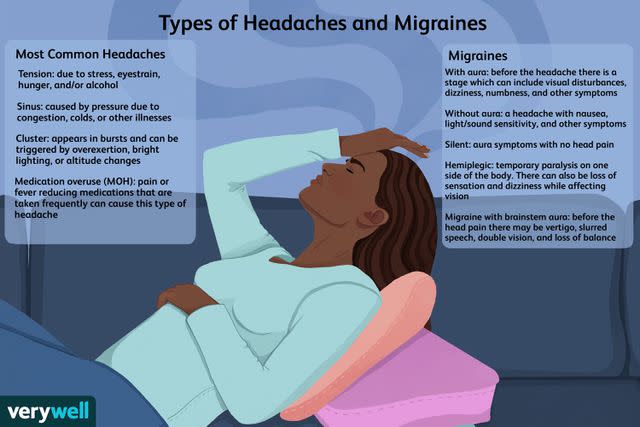
Over 200 types of headaches exist, varying in location, how they feel, severity, and associated symptoms. Determining whether you are experiencing a migraine or other type of headache is crucial to alleviating it effectively and promptly.
Migraine is a type of primary headache, as are tension-type and cluster headaches. Primary headaches exist on their own, whereas secondary headaches stem from an underlying health-related issue, like infection or trauma.
This article will review key symptom and treatment differences between migraines and other headache types, including tension, cluster, and common secondary headaches.
Verywell / Zoe Hansen
Migraine vs. Headache: Location and Quality Differences
Pain location and quality (how it feels) are vital clues in determining whether you are experiencing a migraine or other type of headache, as follows:
Migraine headaches are pounding, throbbing, or pulsating, like a drum beating on your skull. They are usually unilateral, meaning the pain is on one side of the head. Less commonly, migraines can be felt on both sides of the head (bilateral).
Tension-type headaches cause a pressing, tightening, or "band-like" sensation, always on both sides of the head.
Cluster headaches always occur on one side of the head, manifesting as severe, piercing pain localized in or around the eye, eyebrow, or near the temple.
Pain Duration: Another Valuable Clue
Migraines last from four to 72 hours, whereas tension-type headaches last 30 minutes to one week. Cluster headaches occur as attacks—up to eight daily—lasting 15 minutes to three hours.
The pain location and quality of common secondary headache disorders include:
Sinus headaches cause a diffuse or localized pressure-like sensation within the forehead, cheeks, and/or behind the eyes.
Caffeine withdrawal headaches resemble migraine (throbbing) or tension-type headaches (pressing). They are unilateral or bilateral in location.
Post-traumatic headaches resemble migraine (throbbing) or tension-type (pressing) headaches. They are unilateral or bilateral in location.
Giant cell arteritis (GCA), a form of vasculitis (blood vessel inflammation), causes a throbbing headache that can be unilateral or bilateral, often near the temple.
Migraine vs. Headache: Pain Intensity and Associated Symptoms
Pain intensity and associated symptoms are also relevant when sorting out headache type.
The pain of a migraine headache is moderate to severe in intensity, typically preventing a person from engaging in their daily routine. Additionally, migraines are often worsened by physical activity and accompanied by nausea, vomiting, sensitivity to light (photophobia), and/or sound (phonophobia).
An aura, a reversible phenomenon of visual or sensory disturbances, may also precede a migraine headache.
Related: An Overview of Migraine With Aura
Unlike a migraine, the pain of a tension-type headache is usually mild. While a nuisance, tension-type headaches are not debilitating, so most people experiencing one can get on with their daily routine.
Also, tension-type headaches are not aggravated by movement or associated with auras or vomiting, although they may cause a decrease in appetite or display pericranial tenderness (muscle soreness in the head, neck, or shoulder).
Related: Symptoms of Tension Headaches
Cluster headaches are excruciating, even more so than a migraine. The pain has been compared to or reported as feeling worse than a broken bone, kidney stone, or childbirth.
Cranial autonomic symptoms also accompany cluster headaches on the same side as the head pain. These symptoms include facial flushing and sweating, eye redness and tearing, and/or stuffy nose.
Interestingly, cranial autonomic symptoms can occur in individuals with migraine; however, if they do, they usually occur on both sides of the head, not unilaterally as with cluster headaches.
Related: Causes of Ongoing Cluster Headaches
The pain intensity and associated symptoms of common secondary headaches include:
Sinus headaches are mild to moderate and accompanied by thick, greenish-yellow nasal discharge.
Caffeine-withdrawal headaches can be mild or severe and are often associated with fatigue and difficulty concentrating.
Post-traumatic headaches can be mild or severe. Sleep difficulties and dizziness may accompany them.
A giant cell arteritis headache tends to be severe and associated with scalp tenderness, jaw claudication (pain when chewing), and possible vision loss.
Headache vs. Migraine: Does One Turn Into the Other?
A migraine or other primary headache disorder does not turn into the other; however, the migraine or headache can transform into a chronic form.
Chronic Migraine
Chronic migraine, or "transformed migraine," is characterized by 15 or more headache days per month. Various lifestyle factors increase the risk of progression into chronic migraine.
These factors include:
High caffeine consumption
Weight gain
Poor sleep quality and sleep disorders
Migraine and Sleep Are Intertwined
Interestingly, many people with migraine have sleep disorders like obstructive sleep apnea and insomnia. Moreover, sleep deprivation is a common migraine trigger, and sleeping is a classic home remedy for easing migraine attacks.
See a healthcare provider if you have migraines and sleep disturbances. Your provider may suggest keeping a headache diary and sleep log and undergoing a sleep study.
Chronic Tension-Type Headaches
Chronic tension-type headaches occur frequently, sometimes daily, on at least 15 days per month. They are sometimes continuous and can be triggered by chronic stress and the overuse of headache medications.
Chronic Cluster Headaches
Cluster headache attacks occur in cycles. These cycles generally last six to 12 weeks, followed by remission (no attacks), lasting months to years. With chronic cluster headaches, attacks last for a year or longer without remission, or with remission periods lasting less than three months.
It's unclear what causes the shift from episodic to chronic cluster headaches, although alcohol consumption and cigarette smoking may play a role.
Migraine vs. Headache: Treatment Differences
Primary headache treatment depends on type and severity and often involves a combination of medication, lifestyle behaviors, and home remedies.
Depending on the type of secondary headache, lifestyle behaviors and home remedies may play less of a role.
Medication
Mild to moderate migraines can usually be eased with an over-the-counter painkiller like Tylenol (acetaminophen) or a nonsteroidal anti-inflammatory drug (NSAID) like Motrin (ibuprofen) or Aleve (naproxen sodium).
A triptan like Maxalt (rizatriptan) or a combination NSAID/triptan like Treximet (sumatriptan/naproxen) may be needed to stop a severe migraine.
Triptans are prescription drugs that bind to serotonin docking sites in the brain, preventing the action of this chemical messenger. They are available in several formulations, including pills, dissolvable tablets, nasal sprays, and injections.
If a person cannot tolerate or take a triptan (e.g., those with or at high risk for heart disease), a calcitonin gene-related peptide (CGRP) blocker, like Ubrelvy (ubrogepant) or Nurtec ODT (rimegepant), may be recommended.
Likewise, Reyvow (lasmiditan)—a drug that targets serotonin but appears safe in people with or at risk for heart disease—might be prescribed.
Related: How Migraines Are Treated
Like mild-to-moderate migraines, tension-type headaches are treated with Tylenol or an NSAID. Triptans and calcitonin gene-related peptide (CGRP) blockers do not play a role in their treatment.
Related: Tylenol or Advil for Headache
Cluster headaches can be treated with a triptan, but only an injectable or inhaled one since the attacks are short-lived. Oxygen therapy (inhaling oxygen through a facemask) is another treatment for cluster headaches.
Related: How to Get Rid of a Cluster Headache
Medical treatment of secondary headaches involves addressing the root cause:
Sinus headaches are generally treated with OTC painkillers like ibuprofen. Depending on the cause, other medications may be used—for example, a corticosteroid ("steroid") nasal spray for allergies and an antibiotic for a bacterial infection.
Caffeine withdrawal headaches are relieved by consuming 100 milligrams (mg) of caffeine—equivalent to around one cup of coffee—within one hour of the pain.
Post-traumatic headaches are usually eased with Tylenol or an NSAID, although stronger painkillers may be required for severe headaches.
Giant cell arteritis headache (and the condition itself) is managed with high doses of corticosteroids.
Precautions
Due to possible harm, not everyone can take Tylenol or NSAIDs. Only take these medications under the guidance of a healthcare provider.
Lifestyle Behaviors and Home Remedies
Depending on the type of headache you have—primary or secondary—various lifestyle behaviors and home remedies can be helpful.
Migraines
Migraine headaches are often improved by napping in a dark, quiet room and placing an ice pack on the neck. Limiting or avoiding exposure to triggers is also encouraged for people with migraine.
Common migraine triggers include strong smells, sunlight, lack of sleep, hunger, thirst, alcohol, nitrate-containing foods (e.g., bacon or hot dogs), and stress.
Related: Coping With Migraines at Work
Tension-Type Headaches
Like migraine, tension-type headaches can be helped by placing an ice pack on the neck or forehead.
Avoiding triggers is also essential. Interestingly, many migraine triggers are similar to those for tension-type headaches, although odor and hormonal changes (e.g., menstruation or menopause) tend to be specific to migraine.
Cluster Headaches
Although the scientific evidence is scant, some people with cluster headaches benefit from deep breathing techniques during an attack.
Cluster headaches also share a few common triggers with migraine, namely alcohol, nitrate-containing foods, and strong smells. Limiting or avoiding these triggers can help prevent these excruciating headaches.
Lastly, smoking is linked to more severe and frequent cluster headaches. As such, smoking cessation is advised.
Related: Relationship Between Smoking and Headaches
Secondary Headaches
Lifestyle behaviors or home remedies are sometimes helpful in improving certain secondary headaches.
By way of example:
Saltwater rinses and, for some people, steam inhalation may improve sinus headaches.
Physical rest and cognitive behavioral therapy may improve post-traumatic headaches. Preventing these headaches by wearing a helmet and using a seat belt is also crucial.
Keep in mind that most headache disorders, whether migraine or another type, can be helped by engaging in healthy behaviors like regular sleep, exercising, drinking enough water, and eating a well-balanced diet.
Related: Using Your Diet As a Migraine Therapy
For primary headaches, mind-body therapies like meditation, acupuncture, and progressive muscle relaxation can also enhance pain management and help you feel well overall.
Severe Migraine or Headache Not Improving
The vast majority of migraines and other primary headaches can be treated safely at home with OTC or prescription medications. However, a new, severe, or persistent migraine or headache or one that is accompanied by concerning symptoms requires urgent or emergent medical investigation.
Call or see a healthcare provider in the following scenarios:
Your migraines or headaches are occurring more often or preventing you from engaging in daily activities.
You have a new migraine or headache and are over 65, have a history of cancer or weakened immune system, or are pregnant or postpartum.
Your migraines or headaches are associated with taking painkillers regularly.
Your migraines or headaches are brought on by sneezing, coughing, or exercising.
Seek Emergency Medical Attention
Go to the nearest emergency room or call 911 if your headache:
Is severe and starts abruptly, and/or is the "worst headache of your life"
Is severe and associated with a painful red eye, high fever, stiff neck, fainting, confusion, or stroke symptoms
Occurs after a head or neck injury
Related: When Should You Worry About a Headache?
Summary
It can be challenging to distinguish a migraine from other primary headache disorders, like tension-type and cluster headaches, and common secondary headaches, like sinus headaches.
Migraine headaches are pounding and throbbing and usually located on one side of the head, although they can be on both. They are often severe enough to impair functioning at home or work and may be accompanied by nausea, vomiting, and light/sound sensitivity.
Treating a migraine involves a combination of medication (e.g., ibuprofen or a class of drugs called triptans) and home remedies like resting in a dark, quiet room until the pain abates.
Lifestyle behaviors like limiting or avoiding exposure to migraine triggers (if possible), like strong smells or skipped meals, is also essential to migraine care.

