Which Medications Cause Sundowning Symptoms?
Medically reviewed by Mary Choy, PharmD
Sundowning refers to a number of behaviors, feelings, and thoughts that people with dementia may experience toward the end of the day, such as in the late afternoon or evening. During sundowning, these individuals may have more anxiety, agitation, confusion, and sleeping problems.
Though the exact cause of sundowning is unknown, the interplay of multiple factors—like certain medications—may contribute to it by affecting the sleep-wake cycle. These factors may also interrupt the ability to regulate behavior.
This article discusses what you should know about sundowning, including contributing medications, triggers, and treatment options.
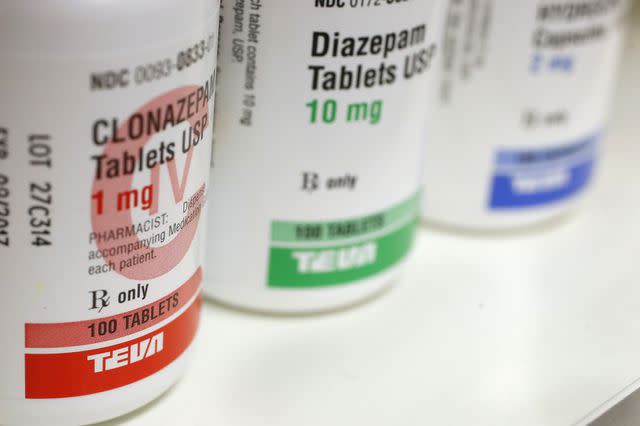
Getty Images / Bloomberg / Contributor
What Is Sundowning?
Sundowning isn't a disease. Instead, it's a group of symptoms or behaviors that people with dementia—like Alzheimer's disease—may experience. In these individuals, sundowning tends to happen toward the end of the day and at night when it gets dark.
Some sundowning symptoms or behaviors may include more difficulty with the following:
Can Medications Worsen Sundowning and Dementia?
The exact cause of sundowning is unknown. However, several factors—like certain medications—may work or interact together to play a role in the sundowning effect. Some medications may contribute to sundowning by interrupting the sleep-wake cycle and interfering with behavior regulation.
In older adults, an altered (changed) part of the brain is linked to sleep-wake cycle medical conditions. People with conditions like Alzheimer's disease also experience these changes, among others, which may disturb the sleep-wake cycle and lead to behavior problems. Certain medications may worsen these issues.
Anticholinergic Medications and Sundowning
Anticholinergic medications treat several medical conditions relating to the bladder, digestive system, brain, and more. They generally work by blocking the activity of a naturally occurring chemical in the body called acetylcholine.
According to a 2023 study, however, the risk of dementia and Alzheimer's disease increases with a higher usage or number of anticholinergic drugs taken.
People with Alzheimer's experience changes in parts of the brain that affect the sleep-wake cycle and lead to behavioral effects. Anticholinergics may worsen these problems further by disrupting the sleep-wake cycle and interfering with how a person can regulate their behavior. As a result, anticholinergics can trigger sundowning symptoms, like agitation, as a side effect.
Examples of anticholinergic drugs include:
Benadryl (diphenhydramine)
Oxytrol (oxybutynin)
This isn't a complete list of anticholinergic medications. If you're unsure whether your medication is an anticholinergic drug, talk to a healthcare provider or pharmacist.
Benzodiazepines
In general, benzodiazepine medications work by enhancing gamma-aminobutyric acid (GABA) activity, which calms down brain activity. GABA is a naturally occurring chemical in the brain. Benzodiazepine medications are taken for various symptoms, which may include:
Agitation
Anxiety
Breathing difficulties
Terminal restlessness in cancer
Though benzodiazepines might have several uses, older adults should avoid these medications.
Older adults experience changes to a part of the brain connected to sleep-wake cycle medical conditions. People with Alzheimer's disease also experience similar changes—in addition to alterations in other parts of the brain—that interrupt the sleep-wake cycle and result in behavioral problems.
Hypnotic medications—like benzodiazepines—might worsen these concerns. In fact, benzodiazepine use is linked to uninhibited behaviors, brain function decline, and agitation in older adults.
Benzodiazepine examples include Xanax (alprazolam) and Versed (midazolam).
This isn't a complete list of benzodiazepines. If you're unsure whether your medication is a benzodiazepine, talk to a healthcare provider or pharmacist.
Other Factors That Trigger Sundowning
Aside from medications, other factors may trigger sundowning. Some examples may include:
Blood pressure cyclical (cycle) changes
Blood sugar cyclical changes
Body temperature cyclical changes
Hunger
Inadequate light
Loud noises and chaos
Mood conditions
Sleep-related medical conditions
Tiredness
Unmet physical or mental needs
Sundowning is likely an interplay of several factors, and this isn't a complete list of possible triggers.
Medications and Supplements for Sundowning
There are treatment options for sundowning. Treatment choices may include:
Melatonin
Cholinesterase inhibitors
Antipsychotics
Hypnotics
Antidepressants
Melatonin
Melatonin is a naturally occurring hormone that your brain makes when it gets dark. It's important in regulating your sleep-wake cycle. These levels are lower in older adults and people with certain conditions like Alzheimer's disease. This is the logic behind melatonin supplementation in people who have a disrupted sleep-wake cycle. However, more high-quality clinical trials to confirm this are necessary.
Cholinesterase Inhibitors
Brain cells transfer information to each other using several naturally occurring chemicals, including acetylcholine. Some researchers believe a disruption of acetylcholine-related transfer of information in the brain might interfere with the sleep-wake cycle and lead to behavioral problems.
In fact, cholinesterase inhibitors that block acetylcholine breakdown showed fewer behavioral issues in people with dementia.
However, there is conflicting data when it comes to these medications' effects on sleep conditions, sleep-wake cycle changes, and sundowning-related behavioral problems in people with Alzheimer's disease and other forms of dementia.
One example of a cholinesterase inhibitor is Aricept (donepezil).
Antipsychotics
Examples of antipsychotics include Haldol (haloperidol), Seroquel (quetiapine), and Risperdal (risperidone).
Antipsychotic medications are often taken for sundowning. However, most clinical trials primarily focus on delusions, hallucinations, and agitation—not sundowning specifically. What's more, experts typically avoid antipsychotic use due to a higher risk of stroke, a faster rate of declining brain function, and death in people with dementia.
Hypnotics
Hypnotic (sleep-inducing) medications may include benzodiazepines, such as Ativan (lorazepam). Though these medications have been taken for sundowning, little data supports this use. Though it sounds contradictory, these medications may also exacerbate behavioral issues.
Antidepressants
In a 2021 review article, the authors presented an approach to appropriately treat acute (short-term) and chronic (long-term) agitation. This treatment approach mentioned several different medications, including the following antidepressants:
Remeron (mirtazapine)
Though agitation is a symptom of sundowning, this treatment approach didn't directly address sundowning.
When to See a Healthcare Provider
If you're caring for a loved one who experiences sundowning, you might wonder when to see a healthcare provider. When it comes to sundowning, experts typically recommend trying nondrug options first. This may include the following:
Identify what is triggering your loved one's sundowning symptoms.
Calmly listen to your loved one's concerns.
Distract your loved one from what is stressing or upsetting them.
Let your loved one know that everything is all right.
Decrease noise and remove chaos.
Choose quieter activities in the evening.
Choose activities that require more attention or alertness earlier in the day.
Get some sunlight outside earlier during the day.
Adjust the lighting by letting in natural light earlier in the day and using softer room lighting when it gets dark.
Limit daytime naps if your loved one has sleeping problems at night.
Limit alcohol, caffeine, and nicotine to prevent sleeping problems.
Eat larger lunches and lighter dinners.
Walk with your loved one to decrease restlessness.
Try to keep to a routine with your loved one
If these nondrug tips aren't helpful, talk with a healthcare provider. A healthcare provider might help identify other potential sundowning triggers, such as pain or certain medications. The healthcare provider might also recognize some medical conditions that may worsen sleeping problems. Examples may include a urinary tract infection (UTI), restless leg syndrome, and sleep apnea.
Summary
Sundowning isn't a medical condition. Instead, it's a group of symptoms and behaviors that people with dementia may experience when it gets darker toward the end of the day.
Though the exact cause of sundowning isn't clear, an interplay of multiple factors may trigger it. For example, certain medications may worsen sundowning.
Other than identifying and removing triggers, there are nondrug ways to help prevent and manage sundowning. If the nondrug tips aren't enough, reach out to a healthcare provider who may recognize other sundowning triggers, like certain medications and medical conditions.
Read the original article on Verywell Health.

