What Is Male Infertility?
Medically reviewed by Jamin Brahmbhatt, MD
Male infertility is when a sexually mature male is unable to get a fertile female pregnant. There are many possible causes for this, including genetics, trauma, diseases or infections of the male reproductive tract, and even lifestyle factors like smoking.
Treatment may involve medications, hormone therapy, surgery, and specialist procedures like intrauterine insemination (IUI).
This article looks at the various causes of male infertility and walks you through what is involved in the diagnosis and treatment. It also offers tips on how to prevent male infertility with healthy lifestyle choices.
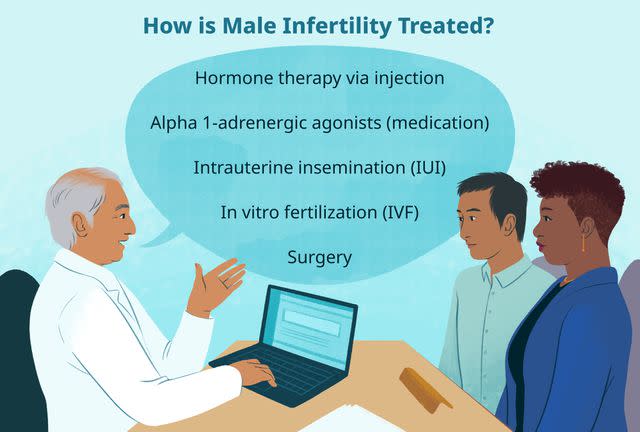
Illustration by Mira Norian for Verywell Health
A Note on Gender and Sex Terminology
Verywell Health acknowledges that sex and gender are related concepts, but they are not the same.
Sex refers to biology: chromosomal makeup, hormones, and anatomy. People are most often assigned male or female at birth based on their external anatomy; some people do not fit into that sex binary and are intersex.
Gender describes a person's internal sense of self as a woman, man, nonbinary person, or another gender, and the associated social and cultural ideas about roles, behaviors, expressions, and characteristics.
Research studies sometimes don't use the terminology in this way. For example, terms that describe gender (“woman,” “man”) may be used when terms for sex (“female,” “male”) are more appropriate.
To reflect our sources accurately, this article uses terms like "female," "male," "woman," and "man" as the sources use them.
Male Infertility Symptoms
Male infertility is defined as the inability of a male to make a fertile female pregnant after a minimum of one year of unprotected sex (sex without using any form of birth control). Other signs and symptoms may be noted depending on the underlying cause.
Causes of Male Infertility
There are many causes of male infertility. These can be broadly categorized as being either congenital (something you are born with), anatomical (related to your body), pathological (caused by disease), sexual (due to sexual dysfunction), or acquired (due to trauma or toxic exposure).
Congenital Causes
Congenital causes of male infertility involve abnormalities of either the endocrine system (which produces hormones) or the male reproductive system (comprising the penis, testicles, and other sex organs). These include genetic disorders that can impair either of these systems.
Some of these congenital conditions cause azoospermia (the inability to produce sperm), oligospermia (the production of low-quality sperm), or male hypogonadism (a lack of the hormone testosterone).
Others can affect the structure or function of the testicles ("balls"), urethra (the tube that transports sperm out of the penis), or vas deferens (the duct that transports sperm from the testicles to the urethra).
Common congenital (present at birth) causes of male infertility include:
Cryptorchidism: Also known as undescended testicles
Cystic fibrosis: A genetic disorder that can manifest with a missing vas deferens
Epispadias: An anatomic variation in which the urethra does not fully form
Hypospadias: A anatomic variation in which the opening of the urethra is not at the end of the penis
Kallman syndrome: A genetic disorder that can cause cryptorchidism and micropenis
Klinefelter's syndrome: A genetic disorder that causes azoospermia in some males
Noonan syndrome: A genetic disorder linked to cryptorchidism, azoospermia, and oligospermia
Prader-Willi syndrome: A genetic disorder associated with hypogonadism and incomplete sexual development
Anatomical Causes
Anatomical causes of male infertility are those in which parts of the male reproductive tract malfunction, typically due to defects that develop later in life.
Anatomical causes of male infertility include:
Retrograde ejaculation: A condition in which semen does not exit the body during ejaculation but flows back to the bladder as a result of a failing bladder sphincter
Varicocele: A condition in which an enlarged, blocked vein near a testicle increases the temperature within the scrotum, damaging sperm cells
Related: Reproductive Health Issues
Pathological Causes
Pathological causes of male infertility include infections, diseases, or malignancies (cancers) that directly or indirectly affect the male reproductive tract.
Some of these cause epididymitis (inflammation of the coiled tube that transports sperm from the testicle), while others cause blockages of ducts and vessels (such as ejaculatory duct obstruction).
Others still affect the endocrine organs that regulate the production of sex hormones like testosterone and estrogen.
Common pathological causes of male infertility include:
Adrenal cancer: Cancer of the adrenal glands (which stimulate testosterone production)
Chlamydia: A sexually transmitted infection (STI) caused by the bacterium Chlamydia trachomatis
Diabetes: A blood sugar disorder that can lead to hypogonadism and azoospermia
Gonorrhea: A bacterial STI caused by Neisseria gonorrhoeae
Pituitary adenoma: A tumor of the pituitary gland (which regulates testosterone production)
Prostatitis: Inflammation of the prostate gland (which can decrease semen production)
Recurrent urinary tract infections: Typically involving males with suppressed immune systems
Sarcoidosis: An inflammatory disease that can cause obstructions in the male reproductive tract
Syphilis: A bacterial STI caused by Treponema pallidum
Testicular cancer: Cancer involving one or both testicles
Tuberculosis: A bacterial lung infection that can spread to the male reproductive tract
What Is Idiopathic Male Infertility?
Not all causes of male infertility are known. Between 10% and 15% of cases are idiopathic, meaning of unknown origin. Idiopathic male infertility is characterized by poor semen quality and/or a low sperm count for reasons that cannot be found.
Sexual Causes
Sexual dysfunction is a common cause of male infertility. It can do so by blunting a person's response to sexual stimulation or by affecting their ability to achieve an erection (the hardening of the penis) or ejaculate (eject semen from the penis).
Sexual dysfunction in males may be due to physical causes, psychological causes, or both. In some cases, the underlying cause may be unknown.
Common forms of sexual dysfunction linked to male infertility include:
Anejaculation: The inability to ejaculate
Erectile dysfunction: The inability to achieve or sustain an erection suitable for sex
Low libido: The lack of sex drive and sexual desire
Acquired Causes
Acquired causes of male infertility are those that result from an injury to the male reproductive tract. These include problems caused by trauma, medications, toxins, and medical treatments as well as certain lifestyle factors that directly contribute to male infertility.
Common acquired causes of male infertility include:
Alcohol use disorder: Linked to testicular atrophy (shrinkage) and azoospermia
Anabolic steroids: Synthetic forms of testosterone linked to testicular shrinkage
Brain or spinal cord injury: Commonly linked to erection and ejaculation problem
Chemotherapy: Especially alkylating drugs that impair sperm quality
Opioid drugs: Prescription painkillers linked to impaired pituitary gland function
Lead poisoning: Associated with both azoospermia and oligospermia
Cannabis (marijuana): Linked to poor sperm quality and reduced motility (movement) when overused
Pelvic radiation: Treatment for prostate and testicular cancer linked to poor sperm quality
Pelvic trauma or surgery: Includes testicular trauma and pelvic nerve injury
Prostatectomy: Prostate removal surgery linked to erection and ejaculation problems
Smoking: Associated with azoospermia, oligospermia, and erectile dysfunction
How Common Is Male Infertility?
Around 15% of couples in the United States experience infertility. Of these, 20% of cases are due to issues related solely to the male partner. Another 30% and 40% involve issues with the male partner that contribute to the couple's inability to get pregnant.
Related: Can Laptops Cause Male Infertility?
How Male Infertility Is Diagnosed
Diagnosing male infertility can be complicated and involve an extensive process of elimination, exploring and excluding all "likely suspects" until a definitive cause is found.
If you and your partner have been unable to get pregnant despite trying for at least a year, speak with your healthcare provider or a specialist in disorders of the male reproductive system known as a urologist.
Medical History
Your healthcare provider will start by reviewing your medical history to determine if you have (or have had) any diseases, conditions, or treatments that could contribute to male infertility.
These include testicular or penile injuries, heavy alcohol or drug use, prior radiation or pelvic surgery, or medications that contribute to sexual dysfunction or male hypogonadism. Your sexual practices would also be discussed.
Physical Exam
The physical exam should involve a comprehensive examination of your penis, scrotum, testicles, vas deferens, urethra, and lower abdomen. A tool called an orchidometer may be used to measure the volume of your testicle to check for discrepancies in sexual development.
A digital rectal exam (DRE) may also be performed. This involves the insertion of a gloved finger into the rectum to check for problems with your prostate gland.
Semen Analysis
A spermiogram is typically the tool used to investigate male infertility. Also known as a semen analysis, the test evaluates the number and quality of the spermatozoa (sperm cells) along with their shape, size, and motility.
The semen sample can be collected at the healthcare provider's office by masturbating and ejaculating into a cup. If you cannot do so for religious or personal reasons, semen can be collected by using a special condom during intercourse.
Lab Tests and Procedures
Various lab tests and procedures may be ordered to check for the underlying causes of male infertility, including:
Hormone tests: Used to check for imbalances in testosterone and other hormones in the blood
Genetic tests: Used to detect genetic disorders like Klinefelter's syndrome or cystic fibrosis
STI screening panel: Used to detect sexually transmitted infections in blood and/or urine
Post-ejaculation urinalysis: Used to detect sperm in your urine due to retrograde ejaculation
Testicular biopsy: Used to obtain a tissue sample from your testicle to check for problems with spermatogenesis (sperm cell production)
Sperm FISH: Used to check for sex chromosome abnormalities in sperm cells using a technology known as fluorescent in situ hybridization (FISH)
Imaging Studies
The main imaging tool used to diagnose male infertility is a sonogram (also known as an ultrasound). The noninvasive test uses high-frequency sound waves to generate images of internal organs and tissues.
There are different types your healthcare provider may use:
Scrotal ultrasound: Used to check for abnormalities in the testicles, epididymis, and vas deferens
Transrectal ultrasound: Used to check inside the rectum for abnormalities of the prostate gland and nearby structures
Related: Best At-Home Sperm Test
How Is Male Infertility Treated?
The treatment of male infertility varies by the underlying cause. This may involve the treatment of testicular diseases, STIs, or conditions like erectile dysfunction. Oftentimes, several conditions are involved, each of which needs to be treated individually.
Although the actual cause of male infertility may not be found, there may still be treatments available to improve your chances of conception. Even so, not all cases can be "fixed," and some couples may need to consider adoption or a sperm donor to achieve pregnancy.
Some of the more common treatments used for male infertility include:
Hormone therapy: A treatment involving medications to boost testosterone and sperm production or injections of hormone stimulators to treat low sperm count in people with hypogonadism
Alpha 1-adrenergic agonists: A class of medications used to treat anejaculation, including pseudoephedrine, midodrine, and Tofranil (imipramine)
Intrauterine insemination (IUI): An assistive reproductive technique in which sperm is collected, washed, concentrated, and delivered to the uterus of the female partner
In vitro fertilization (IVF): An assistive reproductive technique in which an egg is removed from a female partner's ovary, fertilized with sperm in the lab, and returned to the female's uterus
Surgery: Examples include varicocelectomy to treat varicoceles, transurethral resection of the ejaculatory duct (TURED) to treat ejaculatory duct obstruction, and reconstructive surgery to repair conditions like epispadias
Can Supplements Help?
While there are many over-the-counter supplements marketed for male infertility, the American Urological Society states that they have "questionable clinical utility" and that the existing evidence is "inadequate" to endorse any such remedy.
Related: IUI vs. IVF: Making the Right Choice
Can You Prevent Male Infertility?
There are many causes of male infertility that cannot be prevented. With that said, male infertility often involves multiple factors that contribute to the loss of fertility over time. These include lifestyle factors like smoking and drinking.
These four simple tips may help reduce your risk of male infertility:
Quit smoking: Ask your healthcare provider about smoking cessation tools, some of which may be fully covered by health insurance.
Avoid heavy alcohol or cannabis use: If you cannot control your habit, speak with your healthcare provider about alcohol and substance abuse treatment programs.
Avoid overheating the testicles: This includes avoiding tight-fitting pants, switching from briefs to boxers, and wearing light, breathable fabrics during strenuous physical activities.
Wear protective sports gear: This includes jock straps or protective cups whenever engaging in sports like baseball, football, soccer, boxing, wrestling, martial arts, motocross, or horseback riding.
Read the original article on Verywell Health.

