How Is Macular Degeneration Diagnosed?

FG Trade / Getty Images
Medically reviewed by Johnstone M. Kim, MD
Macular degeneration, also known as age-related macular degeneration (AMD), is a progressive form of vision loss that affects the center of what you see. Among the methods optometrists (eye doctors) or ophthalmologists (specialty eye doctors) use to diagnose macular degeneration are several kinds of eye tests and certain imaging techniques. This helps them assess the scale of any damage and ensure that AMD (and not another condition) is leading to vision loss.
AMD occurs due to age-related changes to the macula—the central part of the light-sensitive nerve tissue, or retina, of the eye. Though it doesn’t affect side (peripheral) vision and only rarely causes complete blindness, this condition can progress gradually or rapidly, causing blurriness and other symptoms.
Diagnostic Criteria
There are two types of macular degeneration: dry (non-exudative) and wet (exudative). Dry AMD causes a more gradual loss of vision and progresses through stages. Wet AMD is always severe, and the symptoms advance quickly. Dry AMD can progress into wet AMD, as well.
In the case of dry AMD, your eye doctor can make a diagnosis even before you have symptoms. The following are diagnostic criteria for macular degeneration:
The presence of “drusen,” cone-shaped deposits of protein on the macula (which can emerge before symptoms in dry AMD)
Damage or changes to retinal pigment epithelium (RPE) cells, which are found on the outside of the retina
Geographic atrophy—areas of dead cells in the macula
Abnormal blood vessel growth near the macula (a sign of wet AMD)
Blurriness or loss of parts of central vision upon examination
Medical History
Because many different health factors can cause vision loss, your healthcare provider will need to assess your medical history and any medications you’re taking. Since macular degeneration has a genetic component, they may also ask about any family history of vision problems. They’ll also consider age, as those older than 55 are at increased risk.
You’ll also need to tell your provider about the nature of your symptoms (if any). They’ll want to know when you first started noticing changes, and how they’re affecting you. Signs include blurriness or fuzziness in parts of your central vision, especially in low light, as well as distortions in central vision (straight lines or faces appearing crooked, etc.).
Optometric Exam
To assess the scope of any visual impairment or find early signs, you’ll undergo a complete eye exam (optometric evaluation). This includes tests of visual acuity (how well you see near and far away) and peripheral (side) vision, which is unaffected by macular degeneration.
In addition, they’ll assess how well your eyes work together, whether ocular (eye) muscles are working, as well as your ability to dilate (open) your pupils and adjust to different lighting. They’ll also perform tonometry—a test of eye pressure to detect glaucoma risk—by seeing your eye’s reaction to puffs of air.
With this information and your medical history, your healthcare provider can determine if you need additional testing.
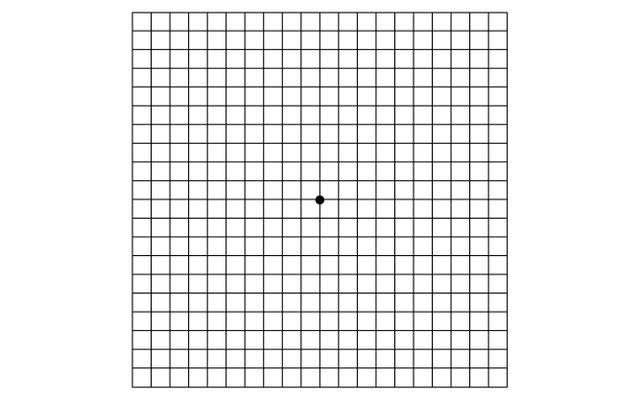
Amsler Grid
Often part of the exam is the Amsler grid, a test you can also do at home, which directly screens for problems with central vision. You stare at a dot in the center of a grid and see if there are any distortions, fuzzy areas, or other issues. Straight lines appearing bent or crooked and blank spots are common symptoms of AMD.
Below is an example of an Amsler grid.
TAK / Getty Images
Slit Lamp Exam
Also known as a fundus examination, this exam lets the optometrist or ophthalmologist look for drusen, or signs of damage on the macula. This can confirm diagnosis even before there are symptoms.
To conduct the exam, your eye doctor will use special drops to dilate your pupils. Then, using a specialized light and microscope device called a slit lamp, they’ll observe areas of the eye. In addition, they’ll test pressure inside the eye (tonometry), muscle response, and other measures of eye function.
Optical Coherence Tomography (OCT)
To help confirm a diagnosis, eye doctors rely on optical coherence tomography (OCT). This non-invasive form of imaging relies on distortions of specific frequencies of light (interferometry) to generate cross-sections of nerve, muscle, and tissue layers in the back of the eye.
Using OCT, ophthalmologists or optometrists can detect signs of both dry and wet AMD. However, this type of imaging isn’t as effective for differentiating between these types of macular degeneration.
Fluorescein Angiography (FAA)
If your provider suspects you have wet AMD, they may also call for fluorescein angiography (FAA). This type of imaging lets them evaluate the progression of macular degeneration and differentiate between dry and wet types.
Healthcare providers first inject a specialized dye into your bloodstream. This makes blood flow in the eye more visible. With the help of highly-sensitive cameras, they can detect the abnormal blood vessel growth or fluid leak around the macula that characterizes wet AMD.
Stages of Macular Degeneration
Dry AMD—which represents about 90% of macular degeneration cases—goes through distinct phases, gradually worsening. Wet AMD is always considered to be advanced. After evaluating your test results and performing imaging, your eye doctor will determine what stage you have. Stages are broken down into early, intermediate, and advanced:
Early dry AMD: Early dry macular degeneration doesn’t usually affect vision; however, small drusen will be visible upon examination of the macula.
Intermediate dry AMD: By the intermediate stage, there may or may not be symptoms, but the drusen are now large. Some may experience slight blurriness or difficulty seeing in low light, which are typical early symptoms of the condition.
Advanced dry/wet AMD: In both advanced dry AMD and wet AMD, the symptoms are pronounced, and the central part of the macula (fovea) has damaged areas (geographic atrophy). This causes visual distortions, blurriness or blank spots, and some loss of color sensitivity in your central vision.
Screening for Related Conditions
During the slit lamp exam, ophthalmologists or optometrists also need to differentiate signs of dry AMD from diseases like vitelliform macular dystrophy, a genetic eye disorder, and retinal drug toxicity, which is damage to the eye due to medications, or many other conditions. Retinal drug toxicity can be caused by Plaquenil (hydroxychloroquine), Desferal (deferoxamine), and Cisplatin, a form of chemotherapy.
If your healthcare provider suspects wet AMD, they will work to differentiate that condition from polypoidal choroidal vasculopathy (PCV), which causes detachments of the RPE layer of the macula. During fluorescein angiography, they look for characteristic signs like orange nodules, bleeding, or fluid buildup under the retina.
Related: Could You Be at Risk of Macular Degeneration?
A Quick Review
Macular degeneration causes blurriness, blank spots, and visual distortion in you the center of what you see. It occurs due to aging-related changes in the macula—the central part of the light-sensitive retina of the eye. AMD is a leading of central vision loss in those older than 55. Though macular degeneration can’t be reversed, timely diagnosis is essential for treatment.
Optometrists and ophthalmologists use several methods to detect AMD. Since early stages of this condition don’t usually cause symptoms, they use the slit lamp exam to detect initial signs, alongside standard eye exam techniques. Imaging techniques help to confirm suspected cases and rule out other potential causes of the condition.
For more Health.com news, make sure to sign up for our newsletter!
Read the original article on Health.com.

