Insulin Resistance: How to Test and Manage Symptoms
Medically reviewed by Kelly Wood, MD
Insulin resistance occurs when a person's body becomes tolerant to the effects of insulin, a hormone that helps blood sugar enter cells for energy.
The exact cause of insulin resistance is unknown but strongly linked to excess body weight and a sedentary lifestyle. Over time, insulin resistance can lead to prediabetes, a precursor to type 2 diabetes.
This article will provide an overview of insulin resistance and how to reverse this abnormal response through physical activity, dietary changes, and weight loss.
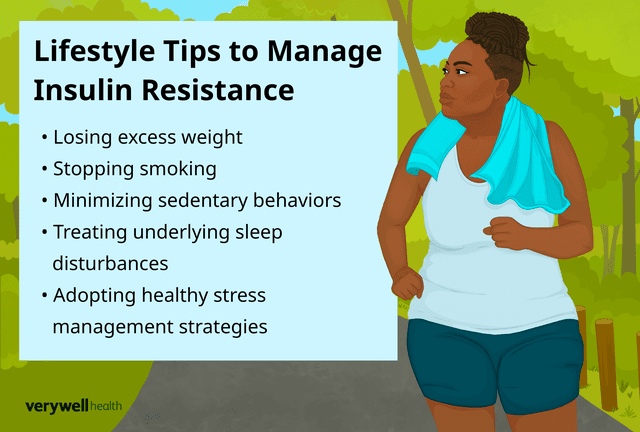
Illustration by Zoe Hansen for Verywell Health
Insulin Resistance: How Symptoms Start
Under normal circumstances, during a meal, a person's stomach breaks down food into glucose (sugar).
The following steps then occur:
Glucose enters the bloodstream, triggering the pancreas (located just behind the stomach) to release insulin.
Insulin guides glucose into cells to be used for energy or stored for later.
As glucose enters these cells, levels decline in the bloodstream, signaling the pancreas to stop producing insulin.
In people with insulin resistance, cells aren't as efficient in taking up insulin to store or use for energy. To overcome this weak cell response, the pancreas produces more and more insulin—what's known as hyperinsulinemia.
Over time, the pancreas cannot keep up with the demands of insulin production, causing blood glucose levels to rise (called hyperglycemia).
Chronic hyperglycemia is a stepping stone to the development of prediabetes and, eventually, type 2 diabetes.
Individuals usually have no symptoms in the early stages of insulin resistance.
As insulin resistance persists and blood sugar levels become chronically elevated, symptoms like the following may manifest:
Excessive thirst (polydipsia)
Frequent urge to urinate (polyuria)
Blurry vision
Unusual tiredness
There are also potential warning signs of insulin resistance on physical examination, such as:
Acrochordons (tiny, harmless skin tags typically found in skinfolds like the neck, groin, and underarms)
Acanthosis nigricans (dark or thick patches of skin often found in skin folds).
Excessive hair growth in females (hirsutism) or male/female pattern hair loss (androgenetic alopecia)
High blood pressure (hypertension)
Hormonal Imbalance in Insulin Resistance
The exact cause of insulin resistance is unclear, although research suggests that in most cases, its development is strongly related to physical inactivity and obesity.
Specifically, physical inactivity leads to fat deposition in the belly, muscles, and liver. Through complex pathways, the accumulation of excess fat impairs insulin signaling (pathways that regulate glucose, fat, and energy steady state) and insulin's ability to regulate glucose uptake by cells.
The presence of metabolic syndrome—a cluster of symptoms that increases a person's risk for type 2 diabetes and heart disease—is also a risk factor for insulin resistance.
Other than obesity, features of the metabolic syndrome include:
High blood pressure
High levels of triglycerides (a type of fat in the blood)
Low levels of high-density lipoprotein (HDL) cholesterol ("good cholesterol")
High levels of blood glucose
Additional risk factors for insulin resistance include:
Increasing age (45 years or older)
Having a parent or sibling with diabetes
Cigarette smoking
Use of certain medications, like chronic glucocorticoid (steroid) use
Having a history of certain health conditions, like polycystic ovary syndrome (PCOS) or Cushing's syndrome
Numerous genes have also been identified that appear to make a person more or less vulnerable to developing insulin resistance and subsequent prediabetes/type 2 diabetes.
In addition to chronic factors like weight gain and lack of physical activity, acute stresses to the body (e.g., severe burn injury or sepsis) can also lead to a diminished response to insulin's effects.
Testing to Diagnose Insulin Resistance
While high insulin levels are often an early marker of prediabetes, insulin levels are not generally tested for unless a person is participating in a clinical research trial.
That said, healthcare providers can test for prediabetes/type 2 diabetes if a person has risk factors for or symptoms of hyperglycemia.
These three blood tests include:
Hemoglobin A1c measures a person's average blood sugar levels for the past three months.
Fasting plasma glucose (FPG) measures a person's blood sugar level when they have had nothing to eat or drink (except water) for at least eight hours.
Oral glucose tolerance test (OGTT) measures blood glucose levels before and two hours after a person drinks a standardized sugary drink.
Learn More: How Prediabetes Is Diagnosed
Role of Diet in Insulin Resistance
The Western diet is linked to insulin resistance. This eating pattern generally consists of a high intake of red and processed meats, refined grains, high-fat dairy products, fast and fried foods, sweets, and sugary drinks.
While diets high in cholesterol, saturated fats, salt, and carbohydrates are associated with insulin resistance, no single diet is found to be superior for reversing insulin resistance.
Instead, professional organizations like the American Diabetes Association (ADA) recommend individualized eating patterns based on personal goals and food preferences (e.g., culture, health beliefs, economics).
See a Dietitian
A registered dietitian (RD) or registered dietitian nutritionist (RDN) can help you create a meal plan based on your ideal daily calorie intake, weight goals, and personal food choices.
What to Eat to Lower Insulin Resistance
The ADA advises eating a diet rich in nutrient-dense foods like fruits, vegetables, whole grains, dairy products, legumes, seeds, and nuts.
Lean protein sources, including plant-based sources and lean meats, fish, and chicken, should also be consumed, with a minimal intake of processed foods and added sugars.
The Mediterranean diet is a prime example of an eating pattern that meets the above recommendations. This nonrestrictive diet encourages a high intake of fresh fruits and vegetables, whole grains, olive oil, beans, nuts, and seeds, and a moderate to low intake of fish, skinless chicken, eggs, cheese, and yogurt.
Other diets that resemble the Mediterranean diet and may be considered include:
Insulin Resistance Treatment
Reversing insulin resistance is primarily focused on healthy lifestyle behaviors.
In some cases, though, a medication called Glucophage (metformin) may be prescribed to improve insulin sensitivity. Metformin lowers blood sugar levels by decreasing gut absorption of glucose and the amount of glucose the liver produces.
It's approved by the Food and Drug Administration (FDA) to treat type 2 diabetes and is typically the first drug used for most people with this diagnosis.
Metformin is sometimes used off-label (prescribed for a condition or at a dosage not approved by the FDA) in people with prediabetes and/or other diagnoses like polycystic ovarian syndrome or obesity.
Related: Options for Treating Insulin Resistance
Complications of Untreated or Mismanaged Insulin Symptoms
If not reversed, insulin resistance can progress to prediabetes and, eventually, type 2 diabetes. Various health complications can then develop from long-term and untreated high blood sugar levels.
These complications include:
Kidney damage (nephropathy)
Nerve damage (neuropathy),
Eye problems, especially damage to the blood vessels in the back of the eye (retinopathy)
Cardiovascular disease, which can lead to a heart attack and stroke
Foot problems like ulcers (open wound/sore) stemming from nerve and blood vessel damage
Related: What Are Complications of Type 2 Diabetes?
Lifestyle Tips to Manage Insulin Resistance
In most cases, engaging in healthy lifestyle behaviors can reverse insulin resistance and prevent or delay the onset of type 2 diabetes.
Losing excess weight, in particular, is crucial to improving insulin sensitivity. Weight loss is optimally achieved through dietary changes, calorie restriction, and increased physical activity.
Specific Recommendations
In people at high risk for or with prediabetes, the ADA recommends at least 150 minutes of physical activity per week and a weight loss of 5% to 7% to prevent or delay the onset of type 2 diabetes.
When devising a plan for staying active (under the guidance of a provider), remember that exercise does not always need to be structured. Consider ramping up household or leisure physical activities like vacuuming, gardening, or enjoying playtime with your pet.
Other lifestyle behaviors to help reverse insulin resistance include:
Stopping smoking
Minimizing sedentary behaviors, especially TV watching
Treating underlying sleep disturbances (e.g., sleep apnea or deprivation)
Adopting healthy stress management strategies—consider daily relaxation techniques, like yoga, meditation, or deep breathing exercises
Summary
Insulin resistance occurs when a person's body develops a diminished response to the hormone insulin. As a result, cells do not efficiently take up blood glucose (sugar) for energy use.
As a stepping stone to prediabetes and type 2 diabetes, the cause of insulin resistance is complex but, in most cases, stems from a combination of health conditions and lifestyle factors, namely obesity and physical inactivity.
Insulin resistance can usually be reversed through sufficient weight loss, which should be achieved through both dietary changes and physical activity.
Specifically, the American Diabetes Association recommends at least 150 minutes of physical activity per week and adopting an individualized meal plan centered on eating nutrient-dense foods like fresh vegetables and whole grains.
Read the original article on Verywell Health.

