Identifying Mouth Sores From Pictures
Medically reviewed by Edmund Khoo, DDS
Mouth sores form in places that include your inner cheeks, gums, tongue, lips, and the bottom or roof of your mouth. They can appear as lesions, bumps, blisters, rashes, or white or colored patches that may be painful.
Mouth sores are related to a wide range of factors that include infection, dental hygiene, or oral cancer. Other mouth sores like a Behcet ulcer or oral lichen planus are symptoms of chronic diseases. Some mouth sores, like aphthous ulcers (canker sores), can occur without a known cause.
Determining the type of mouth sore you have can help you decide on the right course of treatment. Some mouth sores heal on their own; other types require special care.
This article includes pictures of mouth sores and ways to identify the types. It also explains how to treat mouth sores and when to consult your healthcare provider and/or a dentist.

urbazon / Getty Images
Types of Mouth Sores
With so many types of mouth sores, it can be difficult to determine whether a bump or lesion is a serious condition. The following pictures and descriptions provide a basis for identifying some of the most common types of mouth sores. Contact your primary care provider and/or a dentist for a more definitive diagnosis and treatment advice.
Canker Sore (Aphthous Ulcer)

batuhan toker / Getty Images
A canker sore, also known as an aphthous ulcer or recurrent aphthous stomatitis, can appear on the softer parts of your mouth such as your tongue, lips, soft palate, or cheeks. It typically forms as a small pitted lesion that can be painful. A canker sore is often small and round or oval with a yellow-gray color. It typically forms without a known cause.
The three main forms of canker sores are:
Minor aphthous stomatitis: Less than 1 centimeter in diameter
Major aphthous stomatitis: Over 1 centimeter in diameter
Herpetiform aphthous stomatitis: Pinhead-sized ulcers (smaller than 1 millimeter each) that can merge to form larger ulcers
Oral Lichen Planus

Reproduced with permission from © DermNet and © Raimo Suhonen dermnetnz.org 2023
Oral lichen planus is an autoimmune disease that causes chronic inflammation in your mouth. It is characterized by networks of painful white ulcers with fine white lines on your tongue, gums, or inner cheeks. These mouth sores, which can look like a rash in your mouth, can become more painful when you have anxiety or stress.
Behcet's Ulcer

Reproduced with permission from © DermNet and © Raimo Suhonen dermnetnz.org 2023
A Behcet's ulcer is a painful canker sore that appears on the mucous membranes of your mouth. It is a symptom of Behcet's disease, an autoimmune disorder. This type of mouth sore is round or oval with reddish borders. The lesion can be shallow or deep, appearing alone or in a cluster of multiple lesions.
Infectious Sores (Herpes)

Reproduced with permission from © DermNet and © Dr. Mashihul Hossainwww.dermnetnz.org 2023.
Infectious sores (herpes) often look like a cluster of small, fast-developing blisters. They are infectious and spread by skin-to-skin contact with someone who carries the herpes simplex virus (HSV).
The most common symptoms of infectious sores include the following:
Initial redness, heat, swelling, and pain in the affected area before the sores erupt
Painful sores that exist under your nose or on your lips
Blisters that merge then break open when they seep fluid and crust over
Healing in about four to six days
Dental Hygiene-Related
Poor dental hygiene can leave your mouth vulnerable to viral and bacterial infections. These germs can cause gingivostomatitis, a gum and mouth infection that leads to small, painful blister-like sores, gum swelling, and bleeding. Halitosis is also common.
Recurrent Erythema Multiforme

Reproduced with permission from © DermNet and © Te Whatu Ora Waikato dermnetnz.org 2023
Recurrent erythema multiforme is a bull's-eye lesion. It appears as a round sore with three concentric color zones: a darker center with a blister, a middle raised paler pink circle around the center, and a bright red outermost ring. It typically occurs after a herpes simplex virus (HSV) infection.
Hand, Foot, and Mouth Disease

Mouth sores caused by hand, foot, and mouth disease start as small red sores on your tongue and inside your mouth. The spots typically blister and become painful. At the same time, a fever and skin rash on the palms of your hands and soles of your feet may also appear.
COVID-19-Related Sores

Oral symptoms have been linked to infection with the SARS-CoV-2 virus causing COVID-19. These include nonspecific mouth ulcers (can be from many causes), which may be accompanied by tongue inflammation and discoloration. However, it is unclear whether these problems are directly related to the virus, underlying conditions, or treatments.
HIV-Related Sores

Reproduced with permission from © DermNet and © Dr Richard Ashton dermnetnz.org 2023
The human immunodeficiency virus (HIV), the virus that causes AIDS, can cause canker sores on the inside of your cheeks and lips. They may also include red sores on the roof of your mouth and outside of your lips. White or yellowish patches and warts can also occur.
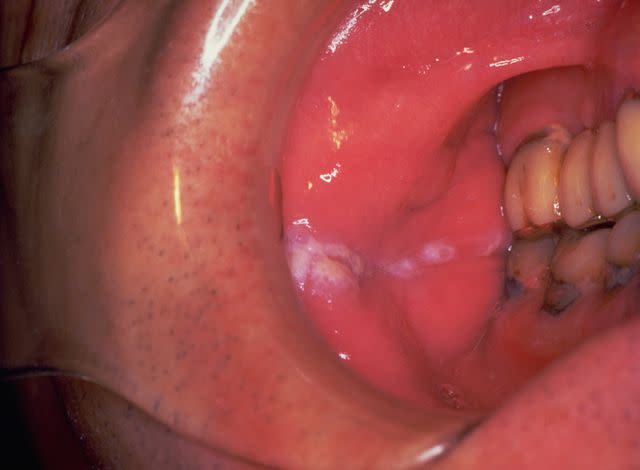
Leukoplakia

Reproduced with permission from © DermNet and © Professor Deborah Greenspan dermnetnz.org 2023
Leukoplakia causes thickened white patches on the mucous membranes of your mouth. The patches are slightly raised and with a hard surface that can't be scraped away. Leukoplakia patches are usually white or gray and do not cause pain. They are common in smokers.
Thrush (Oral Candidiasis)

Reproduced with permission from ©DermNet NZ www.dermnetnz.org 2022
Thrush (oral candidiasis) is an oral yeast infection that causes white or red raised patches inside your mouth or at the back of your throat. It can produce a white coating in your mouth that resembles cottage cheese. Thrush may also involve oral redness and burning.
Syphilis-Related Sores

Reproduced with permission from ©DermNet NZ www.dermnetnz.org 2022
Syphilis is a bacterial infection that starts with mouth sores known as chancres during its early stages. These typically appear on your lips or gums. They can also develop at the tip of your tongue or the back of your mouth. Chancres start as red patches that increase into larger open sores that are painful and change in color to red, gray, or yellow.
Vaping and Smoking-Related Sores
DermNet / CC BY-NC-ND
The nicotine involved in vaping and smoking restricts blood flow to your gums and mucous membranes. These types of mouth sores include abrasions, gingivitis (gum disease), leukoplakia, erosion of the palate, and squamous cell carcinoma (flat, reddish, or brownish patches in your skin).
Sexually-Transmitted vs. Nonsexually Transmitted Mouth Sores
Sexually transmitted infections, such as herpes, syphilis, and HIV, are typically spread to the mouth through oral sex. Nonsexually transmitted mouth sores are spread by close physical, nonsexual contact with an infected person. This is typically the course of transmission with infections such as hand-foot-and-mouth disease and COVID-19.
Cancerous Mouth Sores
Cancerous mouth sores often have many of the same characteristics as non-cancerous types. It is impossible to identify cancerous mouth sores without a biopsy (removing a sample tissue for analysis in a lab). Contact a healthcare provider if you notice signs of cancerous mouth sores or mouth sores that do not improve within two weeks of eruption.
Squamous Cell Carcinoma

Reproduced with permission from © DermNet dermnetnz.org 2023
Squamous cell carcinoma in your mouth starts as flat, thin cells that line your mouth and throat. Early signs of this type of oral cancer appear as a sore, lump, or thickening on your lips or inside your mouth. The sore may look like a white or red patch on your gums, tongue, or the lining of your mouth.
Lymphoma

Reproduced with permission from © DermNet dermnetnz.org 2023.
Lymphoma is classified as Hodgkin's lymphoma and non-Hodgkin's lymphoma. While it primarily affects your lymph nodes, lymphoma can appear as an infection in your mouth, causing mouth sores on your tonsils and tongue and bleeding gums.
Mucosal Melanoma
Mucosal melanoma can affect the mucous membranes in your mouth. Mouth sores can include bleeding lumps, discolored lesions, and ulcers (open sores).
Learn More: What Is Oral Cancer?
Home Remedies for Mouth Sores
Treatment isn't usually necessary for most mouth sores unless the symptoms are unbearable. Most mouth sores will clear on their own within about two weeks, but if they do not, you should see your oral healthcare provider.
Depending on the cause of your mouth sore, you may be able to use home remedies to treat the problem naturally. There is evidence that the following treatments may help some types of mouth sores, but before starting home remedies, please check with your oral healthcare provider. Home remedies include:
Saltwater solution: Rinsing your mouth with a saltwater solution (1 teaspoon of table salt and 8 ounces of lukewarm water) promotes healthy gums and promotes healing. The mixture can dry out canker sores, kill bacteria, and reduce acidity that can irritate your mouth tissue.
Baking soda solution: A baking soda solution (one-half teaspoon of baking soda with 1 cup of water) can be used as a rinse to neutralize the oral pH and increase salivary output, which promotes healing.
Honey: Honey has healing effects that include antibiotic properties when used as a topical treatment for recurrent canker sores.
Coconut oil: Coconut oil has antimicrobial properties due to its high level of lauric acid ( a natural antibacterial agent). It may help treat mouth sores by reducing oral bacterial levels related to a mouth infection and reducing pain. Apply coconut oil directly onto the sore.
Hydrogen peroxide solution: Hydrogen peroxide can kill bacteria, which can promote healing. Use a cotton swab to apply a mixture of equal parts hydrogen peroxide and water to a mouth sore. Follow this with a dab of Milk of Magnesia (magnesium hydroxide) to the sore.
Clove oil: Clove oil has natural antibacterial and anti-inflammatory agents to promote healing. It also has therapeutic actions to reduce oral pain caused by mouth sores.
Alum powder: Alum powder, made from potassium aluminum sulfate, has astringent properties that may help dry out canker sores. Apply a paste (made of a small amount of alum powder and a drop of water) onto the sore. Rinse thoroughly after one minute.
Learn More: How to Get Rid of Canker Sores
Over-the-Counter Mouth Sore Treatments
Some mouth sores may improve with the use of over-the-counter (OTC) treatments. For best results, follow the manufacturer's instructions and only use products intended for your mouth. You can find the following options in grocery stores, pharmacies, and online retailers:
Local anesthetics: Topical gels or creams that contain lidocaine or benzocaine can relieve the pain when these oral products are applied directly to the surface of a mouth sore.
Nonsteroidal anti-inflammatory drugs (NSAIDs): NSAIDs may help relieve the pain and inflammation of mouth sores while they heal.
Mouthwashes with chlorhexidine or triclosan: These ingredients can help prevent the growth of germs that could delay healing or aggravate inflammation.
Mouth sores caused by infections or other medical conditions typically require stronger treatments, such as antibiotics, to eradicate the germs. When underlying conditions exist, treatment involves managing those symptoms and treating the mouth sores.
Learn More: Types of Mouth Infections and How to Treat Them
When to See a Healthcare Provider
While some types of mouth sores are minor and can quickly resolve on their own, contact a healthcare provider if any of the following characteristics apply to your condition:
You notice the mouth sore soon after starting a new medication or other type of medical treatment.
Large white patches form on the roof of your mouth or your tongue, indicating a possible infection.
The mouth sore does not improve within two weeks of eruption.
You have a weakened immune system from conditions such as HIV, cancer, or other diseases.
You have a fever, skin rash, drooling, or difficulty swallowing.
You have a personal history of alcohol use, smoking, or using smokeless tobacco.
You have had treatment involving chemotherapy, radiation therapy, a bone marrow transplant, or stem cell therapy.
Learn More: Recurrent Mouth Ulcers and Canker Sores in Children
Summary
It's difficult to known when a mouth sore indicates a mild or more serious problem. Many types of mouth sores have features that can look alike when viewed in the darkness of your mouth. Other factors like medications and your diet can impact the way a mouth sore looks in your mouth versus the norm.
No matter its cause, a painful mouth sore can affect how you eat and speak. Some can even change the way you look, adding to the stress and anxiety.
If you are unsure about the cause of a mouth sore or have a mouth sore that hasn't changed in two weeks, contact your primary care provider and/or your dentist. Getting the correct diagnosis as early as possible can help you get the best results when treating any mouth sore.
Read the original article on Verywell Health.

