Hypokalemia Symptoms and How to Manage It
A Low Potassium Level Is Relatively Common and Treatable
Medically reviewed by Anthony Pearson, MD
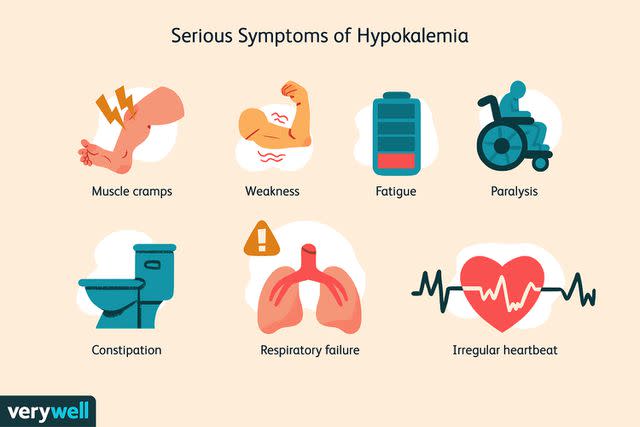
Hypokalemia refers to a lower-than-normal level of potassium found through a blood test. Symptoms of hypokalemia include muscle cramps, weakness, fatigue, and more.
The condition can result from many different medical problems, including those affecting the kidney or gastrointestinal tract. In some instances, it causes life-threatening problems, like abnormal heart rhythms. Hypokalemia is treated with oral or intravenous potassium.
This article looks at the symptoms and causes of hypokalemia, including how the condition is treated.
Verywell / Theresa Chiechi
Potassium in the Body
Potassium is one of the body’s important electrolytes. It is dissolved in your body’s fluids—both inside and outside the cells. However, its concentration is much greater inside cells than in the bloodstream itself.
Potassium and other electrolytes play several important physiological jobs, including sending electrical signals via the body’s nervous system. So it’s not surprising that abnormalities in potassium lead to signaling issues in the electrical systems of the heart and in the nervous system.
Hypokalemia Symptoms
Hypokalemia often doesn’t cause any symptoms, especially if it is minor and occurs in otherwise healthy adults. However, if the hypokalemia is severe, it can cause serious symptoms and problems. The nervous system, gastrointestinal system, kidneys, and heart can all be affected.
Symptoms of hypokalemia include:
Muscle cramps and pain
Weakness
Fatigue
Paralysis
Constipation or complete intestinal paralysis (ileus)
Respiratory failure
Abnormal heart rhythms are one of the most serious potential symptoms, as these can sometimes be deadly. Heart failure is also a possibility. These serious heart problems are much more likely to occur in someone who has underlying heart disease from another cause.
Over the long term, mild but persistent hypokalemia can also worsen other health conditions, such as chronic kidney disease and high blood pressure.
Causes of Hypokalemia
Hypokalemia can occur when something triggers more potassium than normal to move from the blood to inside the cells. In this situation, the total amount of potassium in the body might be normal, but there isn’t enough potassium in the blood. For example, this can happen when a person takes too much insulin.
Potential underlying causes of hypokalemia include:
Prolonged diarrhea or vomiting
Polydipsia (drinking a large amount of fluid)
Certain kidney issues (such as renal tubular acidosis)
Dialysis treatment
Hyperaldosteronism (adrenal gland disease)
Thyrotoxicosis (excess thyroid hormones)
Low levels of magnesium
Rare genetic syndromes (like familial hypokalemic period paralysis)
Hypokalemia may also be caused by certain medical interventions, such as when a person is given large amounts of intravenous fluids in the hospital that don’t contain enough potassium. Medications are also a major potential cause.
Some medications that might cause hypokalemia include:
Diuretics (particularly loop diuretics, thiazide diuretics, and osmotic diuretics)
Corticosteroids (like prednisone)
Laxatives
Insulin overdose
Certain antibiotics (including amphotericin B and penicillin)
Certain drugs for asthma (including albuterol)
How Common Is Hypokalemia?
Hypokalemia is a relatively common medical issue. It may occur in about 20% of hospitalized people and in a much smaller percentage of normal adults. It is the most common type of electrolyte abnormality in hospitalized patients.
Diagnosing Hypokalemia
Hypokalemia may be diagnosed using a blood test.
The normal concentration of potassium in the blood is between 3.5 mmol/L and 5.1 mmol/L. If the concentration is less than that, the individual has hypokalemia. Levels between 3.0 mmol/L and 3.5 mmol/L often don’t cause symptoms. Below 2.5 mmol/L is considered severe hypokalemia.
Hypokalemia itself can be easily diagnosed as part of a common set of blood tests, a basic metabolic panel, or through a slightly larger set of tests called a complete metabolic panel. These tests check the concentrations of several substances in the blood, including electrolytes like potassium. These panels are often run as part of an initial medical workup or as part of general monitoring while a person is hospitalized.
Urinalysis may also be performed to measure how much potassium is in the urine. This test can help your healthcare provider determine the cause of hypokalemia.
Other Tests
Other tests may also be needed if additional symptoms point to specific underlying causes. They include:
Thyroid function tests, if symptoms of thyrotoxicosis are present.
EKG, especially if a person has symptoms from hypokalemia, extremely low potassium, known heart disease, or other conditions that worsen the risk of heart rhythm problems.
Treating Hypokalemia
Minor cases of hypokalemia may be treated with oral potassium. Oral potassium generally carries less risk of causing hyperkalemia. Depending on the situation, this can be taken over a few days to a few weeks. A variety of different preparations of oral potassium are available, and your healthcare provider can prescribe a specific version.
Trying to increase potassium intake through the diet may also be helpful. For example, some of the following foods are high in potassium:
Dried fruits
Nuts
Spinach
Potatoes
Bananas
Avocados
Bran cereals
However, oral supplements of potassium for a period are usually needed as well, unless the hypokalemia is very mild.
Intravenous Potassium
Severe cases of hypokalemia require rapid treatment with intravenous potassium. That is the quickest way to get the potassium in the blood up to the normal level.
However, this needs to be monitored with repeat potassium blood tests and sometimes with continuous monitoring via an EKG. If a person is given too much potassium too quickly, it can lead to hyperkalemia, leading to potentially serious symptoms as well.
Takeaway
Seek immediate medical care if you are taking potassium supplements and experience symptoms like muscle weakness, heart palpitations, or a pins and needles sensation. These might be life-threatening signs of severe hyperkalemia. You should not keep taking potassium long term unless your healthcare provider advises it.
Addressing Other Underlying Issues
Sometimes it’s also appropriate to adjust medications or treat underlying health conditions that may be contributing to the problem. This includes:
Adjusting diuretics: It may be necessary to stop taking a certain diuretic, or switch to a different type of diuretic that isn’t likely to decrease potassium levels.
Treating magnesium levels: If someone has low levels of magnesium in the blood as well as hypokalemia, they will also need treatment with magnesium. Because of the way these two electrolytes are co-regulated in the body, levels of one affect the other.
Treat an underlying condition: For example, someone might develop hypokalemia from Cushing syndrome that developed from a type of tumor of the adrenal gland. One needs to treat this issue to address the hypokalemia as well.
Prognosis
Fortunately, symptoms of hypokalemia usually go away after adequate treatment with potassium. A single instance of hypokalemia doesn't usually cause long-term problems.
However, it's important to note that some individuals who experience an abnormal heart rhythm due to hypokalemia do die. For people with an underlying heart condition, like congestive heart failure, it's especially important to get hypokalemia treated promptly. That's because having hypokalemia in addition to such a condition may increase the risk of death.
Summary
Hypokalemia refers to a lower-than-normal level of potassium in the blood. It's a common medical issue, one often picked up on a laboratory test done for routine testing. Fortunately, it’s usually not a major problem. But it is one that needs to be taken seriously, particularly if it is severe or if you have an existing heart condition.
Symptoms of hypokalemia may include muscle weakness, fatigue, constipation, and irregular heartbeat. If detected, talk to your healthcare team about your treatment plan. The condition can be treated with oral or intravenous potassium.
Read the original article on Verywell Health.

