What Is Hypoglycemia?
Jomkwan / Getty Images
Medically reviewed by Josephine Hessert, DO
Low blood sugar, called hypoglycemia, results when the amount of sugar in the bloodstream drops below normal levels. Because the brain and body rely on sugar from the blood to function properly, hypoglycemia can be dangerous and cause some serious side effects.
While hypoglycemia commonly occurs in people with diabetes who have problems controlling their blood sugar, hypoglycemia can occur in people with or without diabetes. This article will cover symptoms, causes, and treatments for hypoglycemia, as well as when to see your healthcare provider.
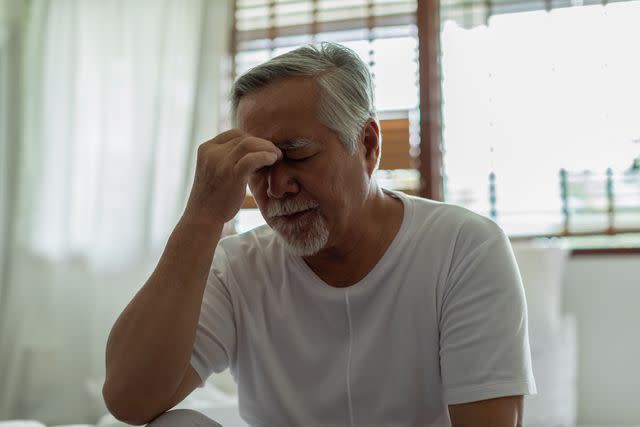
Jomkwan / Getty Images
Hypoglycemia Symptoms
Hypoglycemia can result in a variety of different symptoms that can vary in intensity depending on how low your blood sugar drops. Common symptoms of hypoglycemia include:
Dizziness
Irritability
Sweating
Anxiety
Headache
Trembling
Hunger
Palpitations
Confusion
Incoordination
Blurred vision
Symptoms of hypoglycemia are more likely to occur from situations that cause blood sugar to drop, such as fasting, waiting long periods of time between meals, exercising, and undergoing stressful events.
Severe Hypoglycemia Symptoms
Severe hypoglycemia occurs when blood sugar drops dangerously low, typically below 54 milligrams per deciliter (mg/dL) and often below 40 mg/dL. When this happens, the brain and other organ systems lose the energy supply they need to function properly.
Serious and life-threatening symptoms of severe hypoglycemia include severe confusion, seizures, or loss of consciousness. Without emergency medical treatment, severe hypoglycemia can result in coma or death.
Do Hypoglycemia Symptoms Mean Diabetes?
While hypoglycemia most commonly results as a complication of diabetes, problems with regulating control over blood sugar can also result from hormonal and metabolic conditions. These disorders affect the storage and breakdown of molecules into blood sugar, causing blood sugar to drop too low.
Hypoglycemia Causes
Hypoglycemia results when the body’s functions to maintain stable blood sugar levels stop working properly, resulting in blood sugar less than or equal to 70 mg/dL.
The most common cause of hypoglycemia is diabetes, a condition characterized by abnormally high blood sugar (hyperglycemia). High blood sugar remains elevated in people with diabetes due to the improper release of insulin from the pancreas.
Insulin is a hormone that controls the transport of sugar from the blood into muscles to use for energy. With diabetes, blood sugar remains chronically high when the body becomes less responsive to blood sugar changes and stops releasing insulin to keep everything under control.
To keep blood sugar under control, people with diabetes will typically take insulin to help regulate the control of blood sugar. Sometimes, when factors that normally lower blood sugar are combined with the taking of insulin, blood sugar levels can drop too low too quickly, resulting in hypoglycemia.
Hyperglycemia ("hyper" meaning "high") is high blood sugar while hypoglycemia ("hypo" meaning "low") is low blood sugar.
Read Next:Hypoglycemia vs. Hyperglycemia
Factors that increase the risk of having a hypoglycemic episode include:
Taking too much insulin
Waiting too long between meals or fasting
Not eating enough carbohydrates
How much fat, protein, and fiber are in your meal
The amount and intensity of exercise
Drinking alcohol
Hot and humid weather
High altitudes
Hormonal changes with puberty or menstruation
Other conditions that can affect the ability of insulin to control blood sugar levels include:
Congenital hyperinsulinism: A genetic condition that allows the uninhibited release of insulin
Adrenal insufficiency: Malfunctioning of the adrenal glands affecting their ability to produce steroid hormones, primarily cortisol, that regulate raising blood sugar levels
Glycogen storage diseases: Metabolic conditions that inhibit the breakdown and or/storage of glycogen, a stored energy source in muscles, into glucose (sugar), or the conversion of lactose into glucose
Nocturnal hypoglycemia occurs when your blood sugar levels drop too low while sleeping at night. This is more likely to occur from skipping dinner, exercising before bedtime, or drinking alcohol before bedtime.
What Is Reactive Hypoglycemia?
Reactive hypoglycemia, also called postprandial hypoglycemia, occurs when your blood sugar drops after eating. It typically produces mild or no symptoms. If symptoms are present, they typically resolve on their own as blood sugar levels return to normal.
Because reactive hypoglycemia is associated with diabetes and prediabetes, following healthy lifestyle habits can help reduce the likelihood of reactive hypoglycemia from recurring.
How to Test for Hypoglycemia
Testing your blood sugar levels will be able to determine if you have hypoglycemia. The easiest at-home method involves pricking your finger and using a glucose monitor to calculate your blood sugar.
Alternatively, a continuous glucose monitoring device can be used to provide blood sugar readings 24 hours a day. These devices send signals from an application that is attached to your arm to a monitor to continuously track your blood sugar.
Hypoglycemia Treatment
The most common form of treatment for hypoglycemia is administering glucose either orally, intramuscularly through an injection, or intravenously through an infusion to raise your blood sugar. If your hypoglycemia is mild, it can typically be treated by consuming a fast-digesting carbohydrate source.
To follow the 15-15 rule if your blood sugar is between 55 and 69 mg/dL, consume 15 grams of carbohydrates and check your blood sugar again 15 minutes later. If your blood sugar is still less than 70 mg/dL, repeat the steps. Things that contain approximately 15 grams of carbohydrates include:
4 ounces (one-half cup) of juice
1 tablespoon of sugar, honey, or syrup.
Three to four glucose tablets
One dose of glucose gel (1 tube)
If your blood sugar is 54 mg/dL or lower, it is considered severely low and you will need help from another person. Your healthcare provider may prescribe you an injectable glucagon kit for a friend or family member to give you an injection to raise your blood sugar. After giving the injection, your friend or family member should call 911 for emergency medical treatment.
If your hypoglycemia is due to the effect of diabetes medication lowering your blood sugar too much, talk to your healthcare provider. You may need your dose adjusted to prevent your blood sugar from dropping too low, or you may be prescribed a different medication.
Metformin is a common medication used to lower blood sugar in people with diabetes and is considered at low risk for causing hypoglycemia.
When Should You See a Healthcare Provider for Hypoglycemia?
You should see a healthcare provider if your hypoglycemia continues to occur even after avoiding triggers and following the 15-15 rule. Severe hypoglycemia is a medical emergency requiring immediate treatment if you:
Have severe confusion
Have a seizure
Lose consciousness
Daily Hypoglycemia Management
Hypoglycemia may naturally improve by avoiding triggers, especially going long periods of time between meals, to help keep your blood sugar levels stable. If you are following healthy lifestyle habits and managing your diabetes through diet and exercise, you may also find that you have better control over your blood sugar and may need adjustments to your insulin and/or diabetic medication dosages.
Managing hypoglycemia will involve finding a balance between self-management and standard treatment with a healthcare provider.

