Hyperglycemia Episodes: A Glance at the Short and Long-Term Effects
Also Known as High Blood Sugar
Medically reviewed by Kelly Wood, MD
Hyperglycemia is high blood glucose (sugar) levels. It is common in people with diabetes but can occur in people who have not been diagnosed with diabetes. It can develop slowly with no obvious symptoms.
This article describes symptoms of hyperglycemia and how to test for and manage high blood glucose levels. It also reviews hyperglycemia complications and prevention of hyperglycemia episodes.
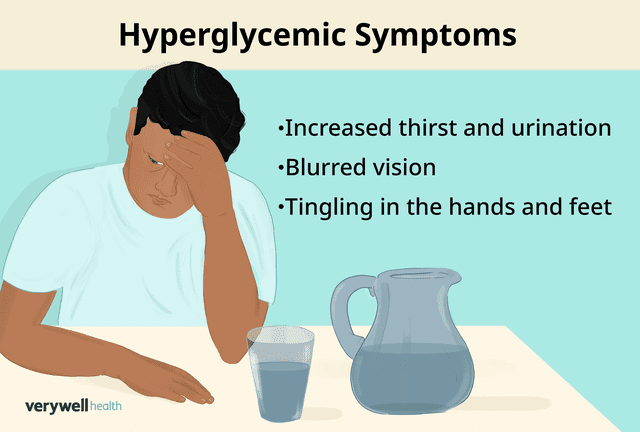
Illustration by Michela Buttignol for Verywell Health
Symptoms of a Hyperglycemia Episode
Depending on the cause of your hyperglycemia, you may not experience physical symptoms for months or years. This is because hyperglycemia can develop and progress slowly over time.
Other times, as with type 1 diabetes for example, symptoms can develop a lot quicker—in a matter of weeks.
Symptoms of hyperglycemia may include:
Increased thirst
Frequent urination
Increased hunger
Blurry vision
Tingling in the hands and feet
Unintentional weight loss
Fatigue
Sores or cuts that do not heal or that heal very slowly
Headache
What Is Hypoglycemia?
While hyperglycemia is when blood glucose levels are too high, hypoglycemia is the opposite—when blood glucose levels are too low. For most people with diabetes, this is a blood glucose level lower than 70 milligrams per deciliter (mg/dL).
You are more likely to experience hypoglycemia if you have diabetes or take medication that can lower your blood glucose. Other risk factors for hypoglycemia include being over age 65 or having other health conditions, such as kidney disease, heart disease, or cognitive impairment.
Why Do Some People Have Hyperglycemia?
In addition to having diabetes, hyperglycemia has many other risk factors. A risk factor is not necessarily a cause but may contribute to the development of hyperglycemia.
Risk factors for hyperglycemia are similar to those for type 2 diabetes. They include:
Being overweight or having obesity
Being 35 years old or older
Having family members with diabetes
Not being physically active on a regular basis
Having prediabetes (when glucose levels are high but not high enough to be considered diabetes)
Having had gestational diabetes (diabetes that develops during pregnancy) or giving birth to a baby weighing 9 pounds or more
Type 2 diabetes is diagnosed more often in the United States in people who are Black, Native American, Asian American, Latinx, or Pacific Islander.
There are several causes of hyperglycemia, which include:
Insulin resistance (when your cells don’t respond properly to insulin)
Reduced or lack of insulin production by the pancreas
Eating lots of highly processed foods with refined carbohydrates and saturated fats
Certain medications, such as corticosteroids, thiazide diuretics (water pills), some psychiatric medications, and certain human immunodeficiency virus (HIV) treatments
Genetic mutations
Hormonal diseases, such as Cushing’s syndrome or hyperthyroidism (overactive thyroid)
Damage or removal of the pancreas
How to Know If You Have Hyperglycemia
If you are experiencing any of the symptoms of hyperglycemia, you should get your blood glucose levels tested.
People with diabetes often have a home blood glucose monitor, also called a blood glucose meter or glucometer. This is a small device into which you insert a single-use test strip. Using a lancing device, you prick a clean fingertip and place a tiny drop of blood onto the test strip. Most glucometers display results within seconds.
Alternatively, you can get your blood glucose levels checked by a healthcare provider. They can determine if you have hyperglycemia and/or diabetes. For diabetes to be diagnosed, blood glucose levels must be:
126 mg/dL or greater while fasting (not eating for at least eight hours)
200 mg/dL or greater without regard to when you last ate
With or without diabetes, in general, hyperglycemia is regarded as too high when it is 160 mg/dL or greater than your personal blood glucose target. Ask a healthcare provider any questions you have about your personal blood glucose target.
If your blood glucose is 240 mg/dL or greater and you take insulin, check your urine with a urine ketone test kit. If ketones are present, follow your "sick day" rules (these rules are a course of action people with diabetes establish with their healthcare provider) or contact a healthcare provider if you are unsure what to do.
Hyperglycemia Treatment and Management
Several different approaches are used to treat and manage hyperglycemia. The base treatment includes lifestyle modifications, such as:
Modifying your diet: This may include increasing the amount of vegetables and fruits, lean protein, whole grains, and healthy fats while also decreasing refined grains, saturated and trans fats, sodium, and added sugars.
Staying hydrated: Water is the best source of hydration for your body. Avoid sugar-sweetened beverages, such as regular soda, juice, regular sports or energy drinks, or flavored coffee or tea drinks.
Increasing physical activity: Regular exercise can help improve insulin sensitivity and decrease blood glucose levels. However, if you have ketones in your urine, do not exercise, as this may raise your blood sugar levels.
Getting enough sleep: Aim for seven to nine hours of quality sleep each night.
Managing stress: This can be done through meditation, yoga, or relaxation techniques
If lifestyle modifications alone are not enough to manage your hyperglycemia, medication may be considered. Several different classes of medications are used to lower blood glucose levels. They may be oral (pills), injectable/infusion, and/or inhalable medication.
Whether your treatment plan includes lifestyle modifications alone or includes medication(s), it is important to adhere to it. Getting your blood glucose levels in a normal range is vital to help prevent complications from occurring.
If you are having trouble sticking to your treatment plan or are not tolerating a medication, talk with your healthcare provider. Regular follow-ups can allow adjustments in your treatment plan and increase your chances of successfully managing your hyperglycemia.
Complications of Mismanaged Hyperglycemia
Untreated hyperglycemia may lead to extremely high blood glucose levels. This could result in potential complications that are acute (meaning they develop rather quickly) but serious.
Complications include:
Diabetic ketoacidosis (DKA), especially in people with type 1 diabetes (insulin-dependent diabetes, in which the pancreas makes little to no insulin)
Hyperglycemic hyperosmolar syndrome (HHS), which usually occurs in people with type 2 diabetes who do not have their blood glucose levels under control
DKA develops when your body doesn’t have enough insulin to help glucose move from the blood into your cells for use as energy. When this happens, the liver breaks down fat and uses it for energy instead. This process creates acid byproducts called ketones.
These ketones can build up quickly to dangerously high levels in the body. Symptoms of DKA include increased thirst and urination, rapid and deep breathing, fruity-smelling breath, dry mouth, headache, fatigue, nausea, and vomiting.
HHS is a life-threatening complication of type 2 diabetes in which there are extremely high levels of blood glucose without the presence of ketones. It usually occurs alongside dehydration, making the blood more concentrated than usual. This leads to symptoms such as increased thirst and urination, weakness, nausea, dry mouth, fever, and confusion.
Seek emergency medical attention if you experience any symptoms of DKA or HHS.
Other complications of mismanaged hyperglycemia tend to take a lot longer to develop but are just as serious. Potential long-term complications of untreated hyperglycemia include:
Heart disease and stroke
Diabetic neuropathy (nerve damage)
Gum disease and other dental problems
How to Stay Ahead of Hyperglycemia Episodes
If you have risk factors for hyperglycemia, it's important to note that some of them are non-modifiable, meaning you can’t change them, such as your age or genetic makeup. However, there are several modifiable risk factors—those you may be able to change—that are usually related to lifestyle.
The best way to stay ahead of hyperglycemia episodes is to stick to your treatment plan if you have one. Following a healthy, balanced diet and regularly engaging in physical activity are two of the most important things you can do to keep your body healthy and blood sugar levels in a normal range. If you take medication, make sure you are taking it as prescribed.
Find yourself a support person (or persons) who can help keep you accountable between visits with your healthcare team. Support people can also applaud your successes and be a sounding board for bouncing ideas off when you are struggling with something.
Monitoring Glucose Levels
Managing your blood glucose levels is often a joint effort between you and your healthcare team. While you are in charge of the day-to-day management of your glucose levels, your healthcare provider can recommend an individualized treatment plan to help keep your blood glucose levels within a normal range.
This may include routinely self-monitoring your blood glucose levels at home. The first step is to purchase or get a prescription for a blood glucose monitor and test strips.
Your healthcare provider or a certified diabetes care and education specialist (CDCES) can teach you and/or a caregiver how to use it. They will instruct you on when and how often you need to test your blood glucose levels at home, such as when you first wake up before eating, two hours after a meal, or at bedtime.
Depending on your diagnosis, you might qualify for a continuous glucose monitor (CGM). This small, wearable device automatically checks your blood glucose levels throughout the day and night. Blood glucose levels are wirelessly sent to a separate receiver or smart device on which you can read the results.
Summary
Hyperglycemia is high blood glucose (sugar) levels. Symptoms include increased thirst and urination, blurred vision, and tingling in the hands and feet.
Hyperglycemia often occurs in people with diabetes but can also occur in people without diabetes. Causes of hyperglycemia include insulin resistance, lack of insulin production, certain medications, stress, and some medical conditions.
You can check your blood glucose level at home using a blood glucose monitor, and your healthcare provider can perform tests for hyperglycemia. Short-term complications of untreated hyperglycemia include diabetic ketoacidosis (DKA) or hyperglycemic hyperosmolar syndrome (HHS).
Long-term complications include heart disease and stroke, diabetic neuropathy (nerve damage), kidney disease, foot problems, eye disease, gum disease, and more.
Treatment for hyperglycemia may include lifestyle modifications such as following a nutrient-rich diet, exercising regularly, getting enough sleep, and managing stress. It may also include medication(s) and self-monitoring of blood glucose levels at home.
Regular follow-ups with your healthcare team are important in ensuring your treatment plan is working and still appropriate for you. Taking proactive steps today to prevent and manage hyperglycemia will help you keep your blood glucose levels in a normal range and benefit your overall health for years to come.
Read the original article on Verywell Health.

