HIV-1: What You Should Know
Predominant strain accounts for the majority of infections worldwide
Medically reviewed by Sameena Zahoor, MD
If you have been diagnosed with HIV, you will have more likely than not been infected with HIV-1. HIV-1 is one of two types of the virus, along with HIV-2, circulating around the world today.
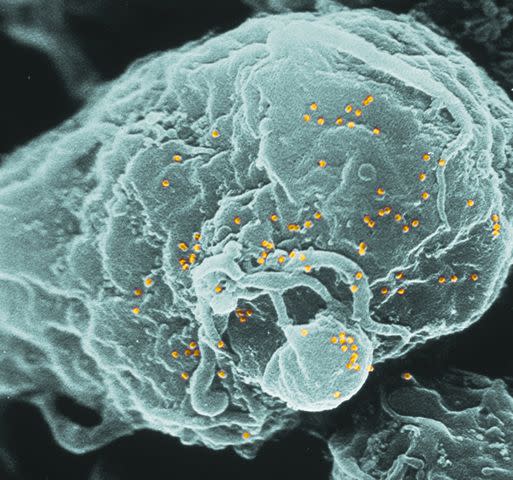
HIV-1 is similar to HIV-2 in that they both cause disease in the same way. They do so by entering the body and infecting a type of white blood cell—called a CD4 T cell—that is responsible for signaling the immune response.
As more and more of these cells are killed, the body becomes increasingly unable to defend itself against otherwise harmless infections, referred to as opportunistic infections.
Callista Images / Getty Images
But there are key differences between HIV-1 and HIV-2. This article takes a closer look at those differences and provides insights into how the virus is diagnosed, transmitted, and treated. It also explains how HIV progresses in stages and the symptoms it can cause as the immune system is gradually depleted of its defensive cells.
What Is HIV-1?
HIV-1 is the most common strain of the virus responsible for the majority of HIV infections worldwide. It is the predominant strain because it is far more infectious (able to be spread) and virulent (able to overcome the body's immune defenses) than HIV-2. As of 2020, less than 0.1% of all HIV infections are attributed to HIV-2.
Geneticists have traced the origin of HIV-1 to chimpanzees and gorillas in western Africa. By contrast, HIV-2 has been traced to the sooty mangabey, a monkey species also found in western Africa. As incidental as these genetic differences may seem, HIV-2 is far less infectious and virulent than HIV-1 and, as a result, is mainly confined to West Africa.
HIV-1 is also far more pathogenic (able to cause disease) than HIV-2. An HIV-1 infection tends to progress faster and is linked to a higher mortality rate overall. Even so, the majority of people with HIV-1 or HIV-2 will die due to the complications of the conditions if left untreated.
Recap
HIV-1 is the predominant strain of HIV in the world today. It is easier to transmit and more capable of causing rapid disease progression (and death) than HIV-2. Over 99% of HIV infections today are caused by HIV-1.
Related: How HIV-1 Differs From HIV-2
Diagnosis
HIV is typically diagnosed with blood tests that detect one of two things:
Antibodies: Defensive proteins produced by the immune system in response to the infection
Antigens: Proteins on the surface of the virus that trigger a disease-specific response
Fourth-generation tests detect both HIV antibodies and antigens. A positive result from a combination HIV antibody-antigen test is confirmed with another test known as a western blot. Together, these tests are extremely accurate in diagnosing HIV.
Generally speaking, the majority of people infected with HIV today are presumed to have HIV-1. However, if there are any indications a person may have been infected with HIV-2, a test called the Multispot HIV-1/HIV-2 Rapid Test is able to differentiate between the two.
Differential testing is generally considered when a person is of West African descent or a person has risk factors for HIV-2 (such as travel to West Africa with no response to HIV treatment).
Differential testing may also be considered if lab-based algorithms (mathematical calculations) indicate an increased likelihood of HIV-2 based on the results of combination antibody-antigen tests.
Recap
HIV-1 can be differentiated from HIV-2 with a test called the Multispot HIV-1/HIV-2 Rapid Test. Differential testing is considered when a person either has risk factors for HIV-2 or when combination HIV test results are suggestive of HIV-2 based on lab-based algorithms.
Related: How HIV Is Diagnosed
Causes
The human immunodeficiency virus (HIV) is passed (transmitted) from one person to the next through body fluids, including semen, blood, vaginal secretions, and breast milk. The causes of HIV-1 are the same as for HIV-2.
The primary routes of HIV transmission are:
Shared use of injecting needles or syringes
Pregnancy and breastfeeding (mother-to-child transmission)
Occupational blood exposure (such as needlestick injuries)
Rare to unlikely causes of HIV transmission include oral sex (due to enzymes in saliva that neutralize the virus) and blood transfusions (due to the routine screening of the U.S. blood supply).
Anal sex and vaginal sex are the most common routes of HIV infection in most countries, including the United States. However, in Russia and parts of Eastern Europe and Central Asia, shared needles are the predominant route due to high rates of injection drug use.
You cannot get HIV from touching, kissing, sharing utensils, mosquitos, or toilet seats.
Recap
HIV is mainly transmitted through contact with body fluids during anal sex or vaginal sex. It can also be passed through shared needles, through occupational blood exposure, or to a child during pregnancy or breastfeeding.
Related: Cause and Risk Factors of HIV
Stages
HIV progresses in stages as the virus gradually kills off CD4 T cells, leaving the body increasingly vulnerable to opportunistic infections.
While HIV-1 and HIV-2 both work in the same way, HIV-1 is far more efficient at killing these defensive T cells. Compared to HIV-2, the amount of virus produced during the early stages of HIV-1 infection is between 10 and 28 times greater. This higher level of viral activity translates to a faster rate of T cell depletion and disease progression.
An HIV infection, whether HIV-1 or HIV-2, is divided into three stages:
Acute HIV infection: This is the earliest stage of HIV in which symptoms may develop within two to four weeks of exposure. Although the immune system will eventually bring the virus under control, the virus will still persist in both the bloodstream and hidden tissue reservoirs.
Chronic HIV infection: This is a period of low disease activity following the resolution of the acute infection. Although a person may be unaware they have HIV, the virus will continue to deplete T cells, leaving them susceptible to an increasing number of opportunistic infections. The chronic stage can last 10 years or more, although some people progress quicker.
Acquired immunodeficiency syndrome (AIDS): AIDS is the final, most severe stage of infection in which the body is fully immunocompromised. Because the virus has severely damaged the immune system, the body cannot fight off opportunistic infections. Without treatment, people with AIDS typically survive for around three years.
Recap
HIV infection is divided into three stages: the acute stage (the period immediately following exposure to the virus), the chronic stage (a period of low disease activity that can often last 10 years or more), and AIDS (the most advanced stage of infection).
Related: How Quickly Can HIV Progress to AIDS?
Symptoms
The symptoms of HIV vary by the stage of the disease and by the individual. For reasons not fully understood, some people will have few notable symptoms until the disease is advanced, while others may develop a life-threatening illness soon after infection.
People with HIV-1 are vulnerable to the same illnesses as those with HIV-2, although they tend to develop sooner. Some conditions, like HIV-associated kidney disease, are common in people with advanced HIV-1 infection but not HIV-2.
The symptoms of HIV can be roughly broken down by stages as follows:
Acute HIV infection: More than half of newly infected people will develop flu-like symptoms, including fever, chills, swollen lymph nodes, sore throat, fatigue, muscle or joint pain, and night sweats. A few may develop a diffuse rash.
Chronic HIV infection: During the chronic stage, also referred to as clinical latency, many people will experience few notable symptoms or develop non-specific symptoms easily attributed to other causes. Some of the more common include experiencing oral thrush, genital herpes, shingles, bacterial pneumonia, and HIV-associated diarrhea.
AIDS: During this advanced stage of infection, people are at risk of AIDS-defining illnesses (meaning those rarely seen in people with intact immune systems). There are 27 conditions classified as AIDS-defining by the Centers for Disease Control and Prevention (CDC) that can potentially affect every organ system of the body.
Recap
The symptoms of HIV can vary by the stage of infection. Although people with HIV-1 are vulnerable to the same illnesses as those with HIV-2, the progression of the disease tends to be faster.
Related: Symptoms of HIV by State
Treatment
HIV is treated with two or more antiretroviral drugs. Antiretroviral drugs work by blocking a stage in the virus' life cycle. Without the means to complete the life cycle, the virus cannot make copies of itself to infect other cells. In turn, the disease cannot progress.
If taken as prescribed, antiretroviral therapy can suppress the virus to undetectable levels where it can do the body little harm. The drugs do not "cure" HIV but rather keep the virus fully suppressed.
There are different classes of antiretroviral drugs used in combination HIV therapy. Each is named after the stage in the life cycle it blocks:
CCR5 antagonists
Fusion inhibitors
Integrase strand transfer inhibitors (INSTIs)
Non-nucleoside reverse transcriptase inhibitors (NNRTIs)
Nucleoside reverse transcriptase inhibitors (NRTIs)
Post-attachment inhibitors
Protease inhibitors (including pharmacokinetic enhancers)
Today, there are more than 25 different antiretroviral drugs approved for use in the United States and 22 fixed-dose combination drugs, some of which allow for once-daily dosing with only a single tablet.
In 2021, the Food and Drug Administration (FDA) approved the first once-monthly injectable therapy, Cabenuva, comprised of the antiretroviral drugs cabotegravir and rilpivirine. Cabenuva can suppress the virus as effectively as daily oral therapies with just two injections per month.
Because antiretrovirals were designed to treat HIV-1, the predominant strain, some are less effective in treating HIV-2. This includes NNRTIs, which HIV-2 appears largely resistant to.
Recap
HIV-1 is treated with a combination of antiretroviral drugs that prevent the virus from replicating. There are over 25 individual antiretroviral drugs approved for use in the United States as well as 22 fixed-dose combination tablets comprised of two or more antiretrovirals.
Related: How HIV Is Treated
Prevention
The traditional strategies of HIV prevention—including the consistent use of condoms and a reduction in the number of sex partners—remain key to avoiding the spread of HIV.
But there are two newer methods of prevention that are extremely effective if you want to avoid getting HIV or passing the virus to others:
Pre-exposure prophylaxis (PrEP): For people without HIV, a daily oral dose of either Truvada (emtricitabine/tenofovir disoproxil) or Descovy (emtricitabine/tenofovir alafenamide) can reduce their risk of getting HIV by as much as 99%. Apretude (cabotegravir) is an injection given monthly for the first two months and then once every two months. It's available for people who weight at least 77 pounds.
Treatment as Prevention (TasP); For people with HIV, maintaining an undetectable viral load with antiretroviral therapy reduces the odds of passing the virus to others to zero.
Despite their effectiveness in preventing HIV, neither PrEP nor TasP can prevent other sexually transmitted diseases (some of which may increase the risk of HIV transmission).
In addition, if you have been accidentally exposed to HIV (either through condomless sex or shared needles), you may be able to avert the infection with a 28-day course of antiretroviral drugs, referred to as post-exposure prophylaxis (PEP).
Recap
In addition to using condoms and reducing your number of sex partners. you can avoid getting HIV by taking once-daily pre-exposure prophylaxis (PrEP). If you have HIV, maintaining an undetectable viral load reduces the odds of infecting others to zero.
Related: 8 Simple Steps to Prevent HIV
Coping
Being diagnosed with HIV can be life-changing, but with consistent care and treatment, people living with the disease can expect to live long, healthy lives. Learning to cope is essential as it influences your ability to remain in care and take your pills every day as prescribed.
You can learn to live well—and even thrive—with HIV by taking a few simple steps:
Educate yourself: Learning how your drugs work and how the virus is transmitted can give you greater peace of mind by ensuring that your health and the health of others are protected.
Stay in care: By seeing your doctor regularly, you can avoid running out of medication, detect drug side effects before they turn serious, and ensure that your drugs are working effectively.
Adhere to treatment: Antiretroviral drugs require a high level of adherence to work effectively and avoid the development of drug resistance. If you struggle with adherence, speak with your doctor. There may be simpler, one-pill options you can be switched to or solutions (like electronic reminders, pillboxes, and adherence partners) that can help get you back on track.
Build a support network: Dealing with HIV on your own can be difficult, leading to isolation and depression. If struggling to cope, ask your doctor for a referral to a live or online support group. You should also reach out to family or friends with whom you can confide in confidence.
Make healthy choices: To avoid non-HIV-related complications common in people with HIV (including heart disease and certain cancers), it's important to see your doctor regularly and make healthy choices. This includes exercising regularly, maintaining a healthy weight, and taking chronic medications if needed to manage conditions like hypertension or high cholesterol.
Get financial assistance: Don't let finances get in the way of your care. If you are struggling to make ends meet, ask your doctor or a social worker to help enroll you in governmental or private financial assistance programs, including patient assistance programs and copay assistance programs.
Seek professional help: If you are unable to cope, do not hesitate to ask your doctor for a referral to a therapist or psychiatrist who can offer group or one-on-one counseling. The same applies if you require treatment for an alcohol or substance abuse issue.
Recap
You can learn to cope with HIV by educating yourself, building a support network, staying in care, making healthy choices, accessing financial aid if needed, and seeking professional help from a therapist or psychiatrist if things get especially rough.
Related: Coping and Living Well With HIV
Risks
Certain factors can increase a person's risk of getting or transmitting HIV. Some of the factors are physiological (pertaining to the body), while others are related to sexual practices. Social, cultural, racial, and economic factors also contribute.
Among the risk factors that can compound a person's odds of infection are:
Anal sex: Anal sex is the most efficient route of HIV transmission, in part because the lining of the rectum is fragile and protected by only a single column of epithelial cells (unlike the vagina, which has many).
Condomless sex: Those at the highest risk of infection are the receptive ("bottom") partners during anal or vaginal sex, although the insertive ("top") partner can also be infected.
Sexually transmitted infections (STIs): Some STIs like syphilis and genital herpes cause ulcers that allow HIV easy access to the body. Others like gonorrhea and chlamydia cause inflammation that increase the concentration of T cells that HIV can target and infect.
Sharing needles: Sharing needles and other drug paraphernalia allows the direct transmission of HIV-tainted blood from one person to the next. Drugs can also impair a person's judgment and increase the likelihood of risky sex.
HIV stigma: The fear of disclosure, homophobia, and stigma discourage many people from getting tested or treated for HIV. On the flip side, HIV "blame and shame" is linked to an increased risk of depression, drug use, multiple sex partners, and sexual risk-taking in people diagnosed with HIV.
Poverty: Poverty limits a person's access to health care and the educational, social, and medical interventions designed to prevent HIV (including PrEP and addiction treatment). Black and Latinx communities are disproportionately affected by poverty and, in turn, HIV.
Recap
Condomless sex, shared needles, and having an STI can all increase a person's risk of getting or passing HIV. Social factors like HIV stigma can often discourage people from seeking testing or treatment, while poverty not only limits a person's access to health care but also to preventive interventions like PrEP or addiction treatment.
Related: The High Risk of Gay Black Men Getting HIV
Summary
HIV-1 is the predominant strain of HIV in the world today, accounting for 99% of all new infections. HIV-1 is not only more virulent but is also associated with faster disease progression than its cousin, HIV-2.
HIV-1 also differs in its genetic origins. Whereas HIV-2 is believed to have originated from the sooty mangabey monkey, HIV-1 is thought to have made the leap from chimpanzees and apes to humans.
HIV-1 can be differentiated from HIV-2 using a blood test called the Multispot HIV-1/HIV-2 Rapid Test. While the symptoms and stages of HIV-1 are the same as for HIV-2, they tend to develop sooner. The modes of transmission are exactly alike.
HIV-1 is treated with antiretroviral drugs that block the virus' ability to replicate. The risk of transmission can also be reduced with antiretroviral drugs, both for people with HIV (by reducing their infectivity with an undetectable viral load with PEP) and people without (by reducing their susceptibility with PrEP).
Condoms and a reduction in sex partners are also important preventive tools. Identifying your vulnerabilities to HIV (such as condomless sex or shared needles) allows you to take steps to minimize your risk.
If you have HIV, you can better cope by educating yourself, staying in care, building a support network, accessing financial aid, and making healthy choices.
A Word From Verywell
While the chances are good that if you have HIV, you have HIV-1, you should advise your doctor if you have any risk factors for HIV-2. This includes being of West African origin, living in or traveling through West Africa, or having sex or sharing needles with someone with risk factors for HIV-2.
Although combination antibody-antigen tests are pretty good a predicting the odds of HIV-2 infection, they are not infallible. By letting your doctor know about your risk of HIV-2, you can undergo differential testing and be placed on medications that may be more effective if you do have this uncommon HIV type.
Frequently Asked Questions
What is the difference between HIV-1 and HIV-2?
HIV-1 accounts for the vast majority of infections worldwide and is more transmissible and virulent than HIV-2. HIV-2 is less transmissible and virulent and mainly confined to West Africa. With HIV-1, the progression of the disease tends to be faster and the symptoms more severe.
Read the original article on Verywell Health.
