Hemolytic Disease of the Newborn Overview
Medically reviewed by Gagandeep Brar, MD
Hemolytic disease of the newborn (HDN) is a condition of red blood cell mismatch between a birthing person and their baby. This occurs when the birthing parent's blood type is Rh-negative and the baby is Rh-positive. During the pregnancy the birthing parent produces antibodies that attack and destroy red blood cells, resulting in anemia in the fetus. A similar condition occurs with platelets called neonatal alloimmune thrombocytopenia.
Causes
Our red blood cells are coated with antigens, substances that induce an immune response. Some of these antigens give us our blood type (A, B, O, AB) and others our Rh group (positive, negative). The Rh group is also called the D antigen.
Birthing parents who are Rh-negative do not have the D antigen on their red blood cells. If the fetus is Rh-positive (inherited from the non-birthing parent), they have a D antigen present. When the birthing parent's immune cells are exposed to the blood cells of the fetus (which can occur during delivery, bleeding during the pregnancy, or due to previous miscarriage), their immune system recognizes the D antigen as "foreign" and develop antibodies against them.
The first pregnancy with an Rh-positive baby is not affected as the antibodies formed initially cannot cross the placenta. However, in future pregnancies, if the pregnant person's immune cells come into contact with the D antigen on the fetal blood cells, the immune system rapidly produces anti-D antibodies that can cross the placenta.
These antibodies attach to the fetal blood cells, marking them for destruction, causing anemia. A similar condition can occur when there is a mismatch in blood type called ABO incompatibility.
How the Infant Is Affected
As discussed above, in a first pregnancy with an Rh-positive baby, there are no problems. If this mismatch is unknown in the first pregnancy (occurs sometimes if first pregnancy results in a miscarriage) or if proper preventative measures (which will be discussed later) are not taken, future pregnancies can be affected. After the first affected pregnancy, the severity of hemolytic disease of the newborn worsens with each pregnancy.
Symptoms are determined by the severity of the red blood cell breakdown (called hemolysis). If the infant is only mildly affected, there may be minimal problems such as mild anemia and/or jaundice that do not require treatment. If the amount of hemolysis is severe, they will have significant jaundice (elevated bilirubin) shortly after birth.
Unfortunately, the hemolysis doesn't stop when the baby is born as the birthing parent's antibodies linger for several weeks. These excessive levels of bilirubin can cause damage to the brain. In some cases, the anemia is so severe in utero (prior to birth) that the liver and spleen enlarge to increase red blood cell production leading to liver failure. The hemolytic disease may also lead to hydrops fetalis with generalized edema (swelling), fluid around organs, and even death.
Prevention
Today all pregnant people receiving prenatal care have blood work drawn to determine their blood type and group. If they are Rh-negative, blood work is sent to determine if they already have anti-D antibodies. If not, they will receive a medication called RhoGAM.
RhoGAM or anti-D Ig is an injection given at 28 weeks, at any episodes of bleeding (including miscarriages after 13 weeks gestation), and at delivery. The RhoGAM is similar to the antibody the pregnant person would make to the D-antigen. The goal is for the RhoGAM to destroy any fetal red blood cells in the parent's circulation before they can develop antibodies.
If anti-D antibodies are found, RhoGAM will not be helpful but additional screening of the fetus will be performed as outlined below.
Treatment
If the pregnant person is determined to have anti-D antibodies and the non-birthing partner is Rh-positive, there is the possibility of hemolytic disease of the newborn. In this situation, testing is performed on the amniotic fluid or blood from the umbilical cord to determine the blood type and group of the fetus. If the fetus is found to be Rh-negative, no further treatment is required.
However, if the fetus is Rh-positive, the pregnancy will be monitored closely. Ultrasounds will be used to assess for fetal anemia and to determine the need for intrauterine transfusions (transfusion given to the fetus while still in the uterus).
The pregnant person's blood will be tested serially during pregnancy to determine how much antibody they are producing. If the fetus is found to be anemic, blood transfusions can be given during the pregnancy to prevent complications (intrauterine transfusions). If the fetus is found to be anemic and is near full term, early delivery might be recommended.
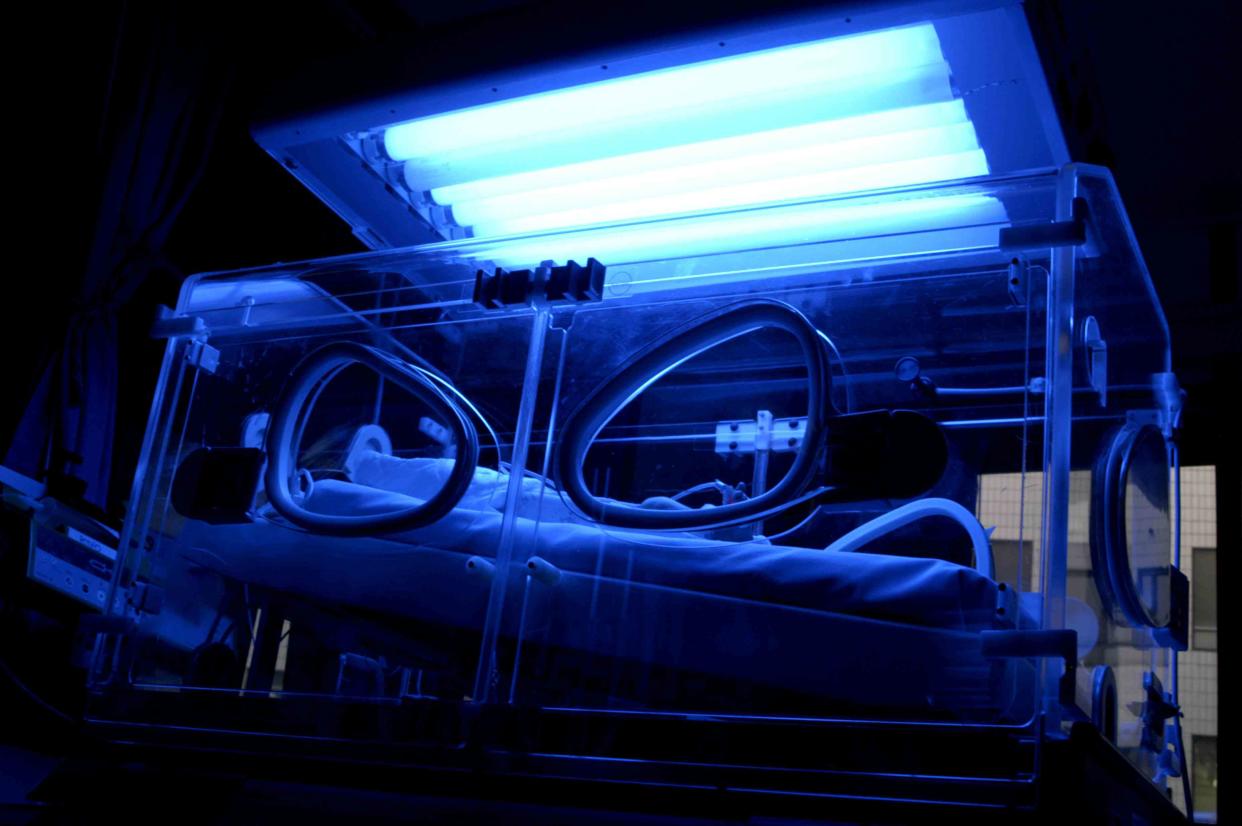
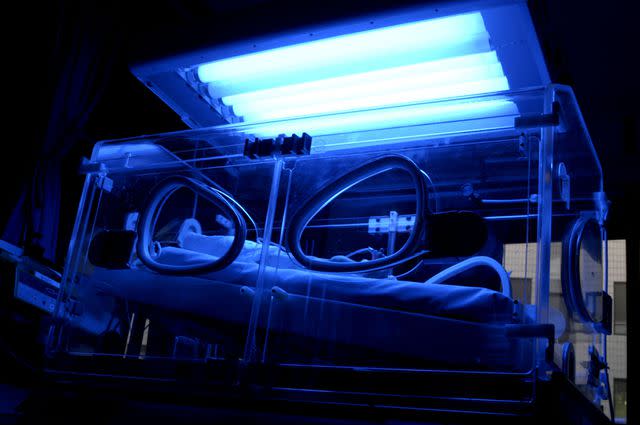
After the baby is born, blood work is sent to monitor for anemia and bilirubin levels. The breakdown of red blood cells doesn't stop as soon as the baby is born so the bilirubin can rise to dangerous levels in the first couple of days. The elevated bilirubin levels (jaundice) are treated with phototherapy where the baby is placed under blue lights.
The lights break down the bilirubin allowing the body to get rid of it. Transfusions are also used to treat anemia. If the anemia and jaundice are severe, the baby is treated with an exchange transfusion. In this type of transfusion, small amounts of blood are removed from the baby and are replaced by transfused blood.
Once discharged from the hospital, it is important to have close follow-up with the pediatrician or hematologist to monitor for anemia. The birthing parent's red blood cell antibodies can cause destruction for 4 to 6 weeks after delivery and additional transfusions may be needed.

