What Is a Vaginal Yeast Infection?

Table of Contents
Overview | Types | Causes | Symptoms | Treatment | Prevention
When yeast infects your vagina (or a baby’s bottom or a man’s penis, for that matter), it can be extremely irritating. But there are effective yeast infection treatments and things you can do to minimize the risk of contracting another itchy, painful infection. For the lowdown on yeast down under, we asked doctors why women are vulnerable to yeast infections, what treatments really work, and what can be done to prevent this uncomfortable problem.
What is a yeast infection?
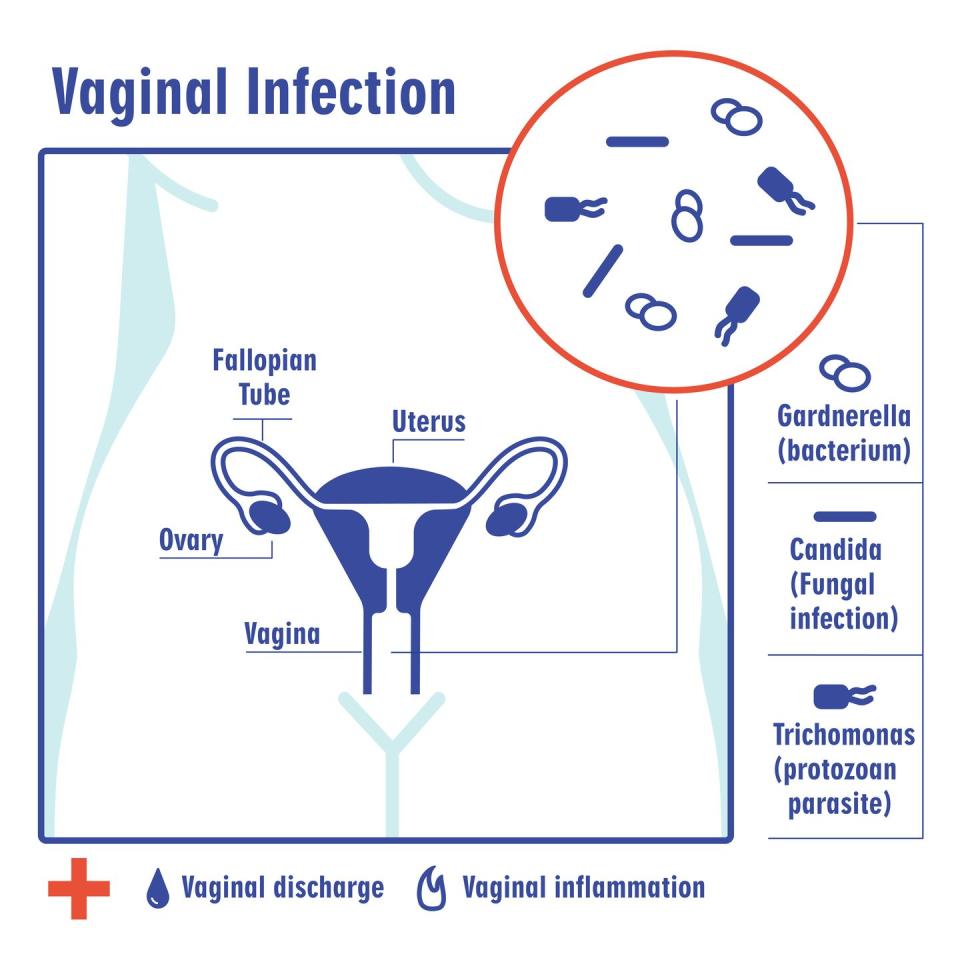
Yeast is a fungus that naturally lives on your skin and inside your mouth, gut, and vagina. But when these fungi overproduce, they can cause infection. There are different kinds of yeast infections, and symptoms vary depending on the part of the body affected. Babies can get infections in their mouths, and men on their penises. Most of the time, though, the term “yeast infection” refers to the itchy, vaginal type.
Yeast infections are the second most common type of vaginal infection, or “vaginitis,” in women, after bacterial vaginosis. It’s estimated that 75 percent of women will have a yeast infection in her lifetime, and 40 to 45 percent of women will have two or more infections.
What are the types of yeast infections?
An overgrowth of yeast can infect and irritate a person’s delicate mucous membranes and skin folds. Here are the main types of yeast infections:
Vaginal (or vulvovaginal) candidiasis
This is another name for the common vaginal yeast infection. Most of these itchy infections are due to an overgrowth of Candida albicans, but sometimes other Candida species or other yeasts are to blame.
Oral thrush
This type of yeast infection, also known as oropharyngeal candidiasis, occurs when yeast overproduce in the mouth or throat. Thrush is common in babies whose immune systems are still developing. Adults with weakened immune systems due to cancer or HIV, for example, or who have certain medical conditions, like diabetes, are also prone to developing thrush.
Candida esophagitis
When oral thrush spreads to the esophagus, it makes swallowing difficult or painful. This is more common in people with HIV or AIDS.
Cutaneous candidiasis
This is another name for a yeast infection of the skin or nails. Warm, moist skin folds of the body, including the armpits, groin, breasts, and buttocks, are particularly vulnerable to infection. Yeast infections are the most common cause of diaper rash in babies.
Penile yeast infection
This is a type of cutaneous candidiasis. When yeast infects the moist skin of the penis, it can cause a condition called balanitis, an inflammation of the head of the penis. Uncircumcised men are especially vulnerable.
Invasive candidiasis
This is a very serious type of Candida infection affecting the blood, brain, bones, eyes, heart, or other parts of the body, according to the U.S. Centers for Disease Control and Prevention. It usually strikes people who are sick with other conditions.
What causes vaginal yeast infections?
The vagina is full of healthy, normal bacteria called lactobacilli. These so-called good bacteria keep the acidity, or “pH,” of the vagina low, and that can keep yeast in the vagina from running amok and causing infection.
“Any time you get out of balance”—say, your vagina lacks enough good lactobacilli or becomes overrun by bad bacteria—“then you can have a yeast infection,” says Emily Cunningham, MD, associate professor of obstetrics and gynecology at the University of Kentucky in Lexington.
What triggers such an imbalance? Hormones, medicines, or changes in a person’s immune system can alter the vaginal environment in a way that encourages yeast to grow, according to the U.S. Centers for Disease Control and Prevention.
Risk factors for developing vaginal yeast infections include:
What are the symptoms of a vaginal yeast infection?
How can a woman tell it’s a yeast infection? Itching is a telltale sign, explains Bilal Kaaki, MD, a specialist in female pelvic medicine and reconstructive surgery at UnityPoint Health in Cedar Falls and Waterloo, Iowa.
The type of discharge also yields important clues, he says. If it has a cottage cheese-like consistency, it’s likely to be yeast. Frothy, grayish discharge suggests it’s bacterial vaginosis (BV), the most common type of vaginitis. A fishy odor? It could be BV or trichomonas, a common sexually transmitted disease.
Doctors often diagnose yeast infections based on a woman’s medical history and findings from her pelvic exam. Sometimes, a swab of a woman’s vaginal discharge will be taken for examination under the microscope. One clue that it’s a yeast infection: The cells will appear in a characteristic “spaghetti and meatballs” pattern, Dr. Kaaki says.
A sample may also be sent to the lab for a fungal culture. (Since yeast can live in the vagina without causing problems, a positive result doesn’t necessarily mean a woman’s symptoms are due to yeast.)
Thick, white, curdy discharge
Redness and swelling of the vulva and vagina
Yeast infection treatment
Most women can easily self-treat a yeast infection.
“There are some very good medications for yeast infections available right over the counter,” Dr. Cunningham says.
Ask your pharmacist to guide you through the array of antifungal creams, ointments, and suppositories from which to choose. Most yeast infections will respond to one-, three-, or seven-day treatment regimens.
Non-prescription topical treatments
Over-the-counter options include clotrimazole, miconazole, and tioconazole.
Prescription medicines
For a severe infection or one that doesn’t respond to OTC treatments, your doctor may prescribe a topical antifungal cream or suppository, such as terconazole or butoconazole.
Fluconazole (Diflucan) is a single pill taken by mouth. Doctors can prescribe additional doses to treat severe or recurrent infections.
Some women prefer popping a pill to dealing with messy creams. But Dr. Cunningham says she isn’t a big fan of the oral option. “In my experience, it can take a good 24 hours, sometimes longer, to actually feel better, and that can be a very long, itchy 24 hours, whereas a cream can have more quick relief,” she says.
Plus, Dr. Kaaki adds, “If someone is pregnant, the pill is contraindicated. so their only option is the cream.”
Alternative treatments
Probiotics: The evidence on taking a probiotic supplement to treat yeast infections is sparse and not very rigorous. While larger, well-designed trials are needed, one review concluded that taking a probiotic alone or in combination with conventional antifungal treatment may be beneficial.
Boric acid: This natural substance, available as a vaginally inserted capsule, can be effective in treating stubborn or chronic infections when other treatments fail, according to one published review. The downside: it can produce a burning sensation. It’s not used very often, Dr. Cunningham says. Boric acid is the same substance used to kill roaches, she confirms. It can be poisonous if swallowed.
How to prevent yeast infections
You Might Also Like

