The Great Blood Sugar Boom: Is Everyone Regulating Glucose Without Me?

Channing Smith/Getty Images
If you took an informal poll among women you know—diabetics excluded—odds are they’d all say that until very recently, they didn’t actively spend time obsessing over their blood sugar levels or understanding how glucose impacts their weight, hormones, and overall health. But now, if you’re even tangentially active in wellness circles on Instagram and TikTok, it’s impossible to scroll through your For You page and not see graphics or detailed videos driving home the idea that balancing blood sugar is the secret to optimal health.
This is thanks in part to the rise in celebrities (and beauty editors) openly taking blood-sugar-managing medications like Ozempic. But it’s largely influenced by Jessie Inchauspé, otherwise known as the Glucose Goddess.
A French biochemist who regularly monitors her own glucose and shares charts and lengthy captions of her findings to social media, Inchauspé has gone viral for easy-to-understand science- and research-backed lifestyle hacks, tips, and recipes to help readers prevent glucose spikes throughout the day. She’s become such a sensation, in fact, that she’s written several best-selling books, including the New York Times bestseller The Glucose Goddess Method, and appeared on the January 2024 cover of Elle France.
Inchauspé’s success proves that there’s more to getting a comprehensive picture of what wellness looks like outside of diet and exercise. Even if you knew that blood sugar is important, you probably didn’t know why—or what to do about it.
Of course, understanding why blood sugar plays a role in overall health is more complex than following a few Instagram accounts so, below, we asked experts to break down everything you need to know.
What exactly is blood sugar, and why is it important?
“Blood sugar is glucose in your bloodstream," Florence Comite, MD, an endocrinologist and founder of the Center for Precision Medicine and Healthy Longevity, says. “It is your mind and body’s primary source of energy, and initially comes from food, in particular carbohydrates.”
As for why that matters? “Glucose provides the energy for the proper function of all your organs and to power your brain activity,” she says. “Playing such an important and all-encompassing role, sugar’s balance in your body needs to be properly maintained to remain regulated, without dramatic highs and lows that can compromise optimal health over time leading to disease of aging, diabetes, heart attacks, stroke, Alzheimer’s and others.”
Jacob Teitelbaum, MD, a board-certified internist and author of The Complete Guide to Beating Sugar Addiction, equates glucose with how a car requires gasoline. “Blood sugar is the main fuel that our cellular furnaces, called mitochondria, can burn. Just like gasoline is what a car burns for energy," he says. “If blood sugar levels go too low, it triggers panic and sugar cravings, just like suffocating would trigger air cravings. If it consistently goes too high, it can trigger diabetes and insulin resistance.”
Insulin resistance is another term you might be seeing more often. Insulin resistance goes hand in hand with blood sugar. “When blood sugar levels are consistently high, insulin resistance can develop, as cells stop optimally responding to insulin,” says Michelle Darian, MS, MPH, registered dietitian and marketing manager of science and product at personal health monitor InsideTracker. “This results in a buildup of blood glucose, or hyperglycemia, which continues to increase your fasting blood glucose. If left unaddressed, this can quickly become pre-diabetes, and eventually, type 2 diabetes.”
In short: When your muscle, fat, and liver cells stop properly responding to insulin, they can no longer use the glucose in your blood for energy or store it. Think of a car losing its ability to properly use gasoline. This results in your pancreas overcompensating and producing even more insulin (like when someone with oily skin stops using moisturizer, resulting in even oilier skin), which leads to elevated blood sugar, which can ultimately cause pre-diabetes and type 2 diabetes.
How does blood sugar affect your health otherwise?
Type 2 diabetes and pre-diabetes aren’t the only reasons to keep your glucose levels in check. According to Darian, unstable blood sugar can lead to sleep disorders, poor sleep over all, dizziness and lightheadedness, blurred vision, excess weight gain, fatigue and low energy, and—most well-known of all—mood swings. “An inefficient metabolism can affect energy production and hormone regulation in ways that lead to mood disorders,” she says. Many people also report simply feeling off.
Dr. Teitelbaum actually references the impacts of low blood sugar as the primary cause of “hanger” (angry hunger). “For low blood sugar, presume low blood sugar and adrenal fatigue if you get irritable when hungry, or hangry,” he says. “Make clear to your loved ones that when you get this way, they should not try to comfort, hug or console you. Instead, they should just feed you.”
But what you eat matters too, or else you only delay the inevitable (crash). “Elevated blood sugar after consuming a high-carbohydrate meal like a bowl of pasta or rice, or a sugary drink or snack or candy bar, is often followed by a significant drop in blood sugar due to rapid release of insulin, causing weakness, fatigue, hunger, anger, and a jittery feeling,” says Dr. Comite. “Over time, chronic hyperglycemia can damage the lining of your blood vessels, leading to conditions affecting your brain, kidneys, heart, skin, nerves, eyes, and feet, as well as contributing to aging and chronic, common diseases of aging like diabetes, heart disease, stroke, Alzheimer’s disease, and cancer.”
Hyperglycemia, or high sugar, also interferes with healing from infections, and from both viral and bacterial diseases (like COVID); it challenges responses to treatment and contributes to getting sicker as well, according to Dr. Comite.
What causes blood sugar spikes?
Glucose always rises and falls throughout the day, but certain habits and foods can make the spikes larger and more frequent than others. “Glucose normally fluctuates throughout the day, particularly after meals. The levels also fluctuate in response to what we eat and when we eat, exercise, stress, sleep, and more,” Dr. Comite says. “This is a normal response to your blood sugar. Higher glucose spikes and lower glucose valleys can increase fasting blood sugar over time, so it’s best to address them.”
Of course, for individuals without diabetes, occasional fluctuations and spikes within an acceptable range are generally not a cause for concern. “However, consistent or severe fluctuations warrant attention and are likely indicative of underlying health issues. It’s important for individuals, especially those at risk for diabetes, to be mindful of their lifestyle choices to help maintain stable sugar levels,” says Dr. Comite.
Some of those lifestyle choices include shifting your diet. “Foods high in refined sugars or simple sugars are quickly broken down into glucose and absorbed into the bloodstream,” she continues. “This causes a spike in your blood glucose and a subsequent spike in insulin, which can contribute to the development of insulin resistance over time.”
Carbohydrates such as bread, cookies, cake, rice, and pasta fairly universally raise blood sugar, though Dr. Comite asserts that it depends on the individual. “While one person may see a sugar spike triggered by eating a banana or another high fructose fruit, another person’s blood sugar won’t spike from eating the same food,” she points out.
Other essential lifestyle choices? Getting enough sleep and keeping stress under control. “Other triggers of a rise in blood sugar are compromised sleep and stress, which increase the hormone cortisol,” Dr. Comite says. “Elevated cortisol over time leads to increased blood glucose."
How to know if your blood sugar levels are imbalanced
“If you’re feeling shaky, sweaty, or having irritability before meals (especially if meals are delayed), your body might be giving you a heads-up that it’s hypoglycemic, or low blood sugar,” says Daryl Gioffre, celebrity nutritionist and author of Get Off Your Sugar. “You could also notice some dizziness, irritability, brain fog, or difficulty concentrating. Fatigue is relieved by eating, and your energy will fluctuate wildly, right along with your blood sugar. It’s your body’s way of saying, ‘Hey, I need a snack (read “glucose”)!’”
Elevated blood sugar, or hyperglycemia, can also make you feel super thirsty, resulting in you needing to take frequent bathroom trips, says Gioffre. “You may notice you’re more tired than usual, experience blurred vision, and/or find that cuts and bruises are taking longer to heal,” he says.
Feeling off after eating a high-carb meal like pasta or rice is also a good indicator. “Feeling jittery, hungry, weak, faint, or fatigued following a high-carbohydrate meal (even a simple breakfast of a banana and a bran muffin) is a delayed reaction indirectly due to the initial elevated sugar,” she explains. “These symptoms are triggered due to the subsequent rapid fall in sugar which follows the rapid release of insulin, peaking after the sugar high, after a pure carbohydrate meal.”
How to reduce blood sugar spikes
Less sugar, more fiber
To reduce glucose spikes, Dr. Teitelbaum suggests cutting down on sugar. “Especially sodas and fruit juices,” he says. “Instead, increase dietary fiber such as vegetables and whole grains.”
Darian agrees, reiterating the importance of fiber. “Soluble fiber-rich foods like oats and beans can help to slow the absorption of glucose into the bloodstream,” she says. “Another tip is to pair carbohydrate-containing foods with sources of protein and healthy fat. For example, serving brown rice with salmon. The addition of protein and fat also helps to slow the absorption of food and can result in lower spikes in glucose following the meal.” This is what the Glucose Goddess refers to as “putting clothes on your carbs.”
Oh, and no: This doesn’t mean no sugar. It’s just best to eat dessert after a meal full of fiber, protein, and fat (remember: the clothes!).
Eat protein
“In general, the intake of protein, fiber, and healthy fats prior to carbohydrates and reducing sugar and refined carbs intake will make a difference,” says Dr. Comite. “I recommend to patients that they begin every meal and snack with protein like Greek yogurt, cheese, walnuts, other nuts, or chicken breast, eggs, or other sources of protein such as edamame, pumpkin seeds, and more. Protein slows the absorption of the carbohydrates and works to keep blood glucose stable with a more balanced release of insulin to avoid spikes and dips.”
Protein also helps keep you fuller longer, preventing cravings. “Eating fiber and healthy fats are other ways to tamp down the glucose surge from starchy foods or foods high in simple, fast-absorbing carbs, such as sugar-sweetened beverages,” she says.
Stay active
“Physical activity, or lack thereof, will affect blood sugar levels,” says Gioffre. “Exercise can lead to increased glucose uptake by muscles, temporarily lowering blood sugar. On the flip side, a sedentary lifestyle with prolonged sitting may contribute to higher blood sugar levels.”
Dr. Comite also recommends weight training. “Muscle stores glucose in the form of glycogen, keeping the levels of sugar in your bloodstream stable. More muscle equals better sugar control,” she says, providing yet another good reason to increase your protein intake.
Walk after eating
Aside from weight training, walking is one of the best forms of exercises for blood sugar management—which Dr. Teitelbaum suggests doing outside. “Both exercise and vitamin D are associated with lower diabetes risk,” he says.
For bonus points (and better regulated glucose) try walking after eating each meal. Studies (and the Glucose Goddess findings) show that doing so helps regulate glucose levels.
Consider supplements
Dr. Comite notes that while individual responses to vitamins and supplements may vary, there is evidence that chromium, vitamin D, and magnesium may help with managing blood sugar, but that should be discussed with your doctor first.
“Chromium is a mineral involved in the metabolism of carbohydrates, and some studies suggest that chromium supplementation may help improve insulin sensitivity,” she says. “Adequate levels of vitamin D are important for overall health, while some research suggests a potential link between vitamin D deficiency and insulin resistance, and some studies have indicated a potential association between magnesium intake and improved insulin sensitivity.”
Get a continuous glucose monitor
At the end of the day, no two individuals are alike: What spikes someone else’s glucose might not do the same for you. “Each person is unique. Surprisingly, even identical twins do not necessarily respond the same,” Dr. Comite says.
To know exactly how varying factors impact you, Dr. Comite recommends using a continuous glucose monitor (CGM) to learn your fasting glucose and unique response to activities, food, stress, and more. “Switch up food intake to assess your response with the CGM," she advises. “Try singular foods one at a time and meals to see what works best for your body profile.”
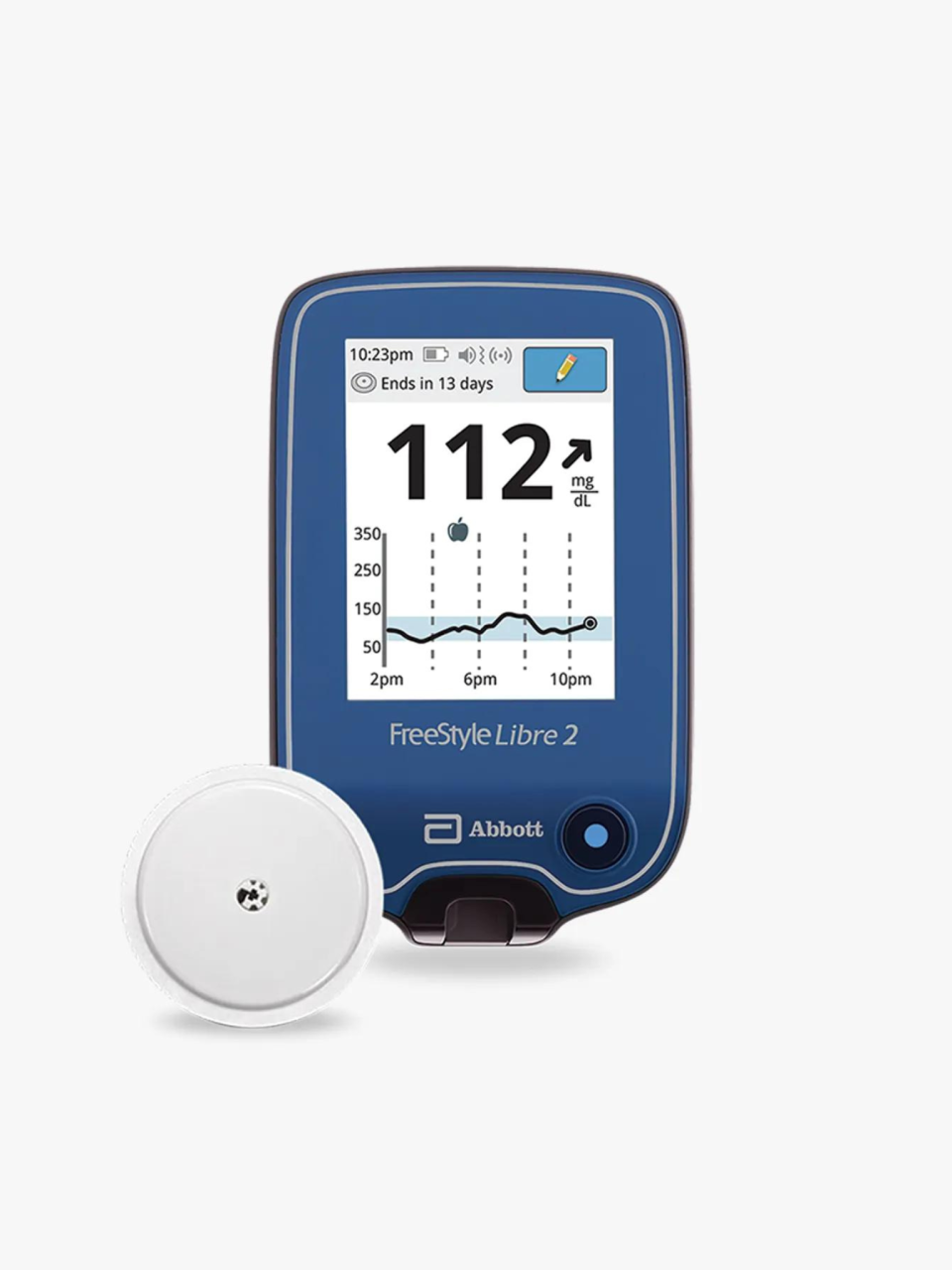
Abbott FreeStyle Libre 2
$.00, Walgreens
There are also finger-stick blood tests, which Dr. Comite notes are less comfortable and therefore a hurdle for most patients. “CGMs are so much easier and more convenient because they track interstitial glucose (the sugars in the fluid around your cells) and communicate that info in real time to your smartphone,” she says.
Dr. Comite is such a fan, in fact, that she’s been wearing a CGM for several years. “My CGM tells me in real time how food, sleep, stress, and my activities affect my glucose. I can better control my sugar levels to stay on an even keel,” she explains. “I recommend that all my patients use one because I’ve seen that everyone has a disorder of carbohydrate metabolism. We are all either diabetic or on a trajectory toward diabetes or insulin resistance unless we intervene to reverse it.”
Consult a medical professional
Finally, if your blood sugar levels are a concern, it’s best to schedule a visit with your doctor or a health care professional for further testing.
“They can conduct tests and provide guidance based on your individual health status,” Dr. Comite says. “Tests to gain insight into one’s glucose levels and risk for diabetes should be drawn after an overnight fast, ideally 12 hours but no less than 8 hours, and should include fasting glucose, fasting insulin, HbA1c (hemoglobin A1c) and OGTT, which stands for oral glucose tolerance test.”
Why is blood sugar trending now?
Just because something’s trending doesn't mean it’s trivial. That said, it’s up to you to do your own research.
During the past few years—mostly thanks to the COVID-19 pandemic—we’ve seen interest in overall health, wellness, and preventative lifestyle changes that boost them skyrocket. “Since COVID, there’s more of a heightened awareness around prevention and being more proactive toward your health,” Gioffre says. This includes the rise in GLP-1 medications like Ozempic that target glucose levels, says Dr. Comite. “The once-a-week GLP-1 agonist injectables has raised awareness [about blood sugar],” she says.
Consider the surge of celebrities shivering their way to well-being via cold plunge, the willingness to wince through daily shot of apple cider vinegar for “longevity,” or the fact that beauty, wellness, and health are now so intertwined that Glamour incorporated wellness into its Beauty Awards last year. Clearly, there’s been a cultural shift: People are prioritizing their health in a whole new way, which includes understanding their blood sugar levels.
Danielle Sinay is the associate beauty editor at Glamour. Follow her on Instagram @daniellesinay.
Originally Appeared on Glamour

