Getting A Copper IUD Is Actually Better Than Taking Plan B For Emergency Contraception
"Hearst Magazines and Yahoo may earn commission or revenue on some items through these links."
Editor’s note: This article does not constitute individual medical advice, and you should consult with your doctor before deciding if any medical decisions are right for you.
At no time in the past 50 years has a broken condom had more dire consequences than it does now. On June 24, 2022, the U.S. Supreme Court issued a ruling in Dobbs v. Jackson Women’s Health Organization—a case that dealt with Mississippi’s 15-week abortion ban and ultimately challenged the long-standing Roe v. Wade, which granted the right to an abortion. The court’s decision to overturn Roe via Dobbs effectively unraveled 50 years of precedence, opened the floodgates for restrictions to abortion, and launched emergency contraception into a new stratosphere of importance. Now, in more than 20 states, abortion is either extremely difficult to access or illegal. Roughly one in three U.S. women live in states where abortion is simply not a viable option, according to the Guttmacher Institute.
Accidents happen. Contraception fails. And because abortion care is so restricted in so many places, these scenarios can be more stressful than ever. Thankfully, emergency contraception (though no replacement for abortion care) can be an effective tool for preventing pregnancy—if used correctly.
The problem is, there’s way too much misinformation out there about emergency contraception. As a physician and contraception researcher, I feel this is yet another disturbing sign of how twisted our conversation around women’s health has become. The laws and restrictions on abortion care are really about control and oppression—not health. Similarly, so much of the misinformation around contraception and emergency contraception, and Plan B in particular, stems from ideology, not science.
It’s time to clear things up. Here are the myths and facts about emergency contraception, including a full breakdown of the options, how they *actually* work, and how to get your hands on them.
Myth: Plan B is your only option.
When you need emergency contraception, you actually have multiple options to choose from. The first is the one everyone thinks of: Plan B, or levonorgestrel, which is also sold under generic names like Take Action and New Day. Levonorgestrel is a synthetic progestin, similar to what is in regular birth control pills and the hormonal IUD. Next is another pill, Ella, which contains ulipristal acetate, a selective progesterone receptor modulator. Both of these types of pills work to shift your natural hormone levels in order to interrupt the normal signaling in your brain that tells your ovaries when to ovulate. The result: the release of an egg (a.k.a. ovulation) is prevented or delayed.
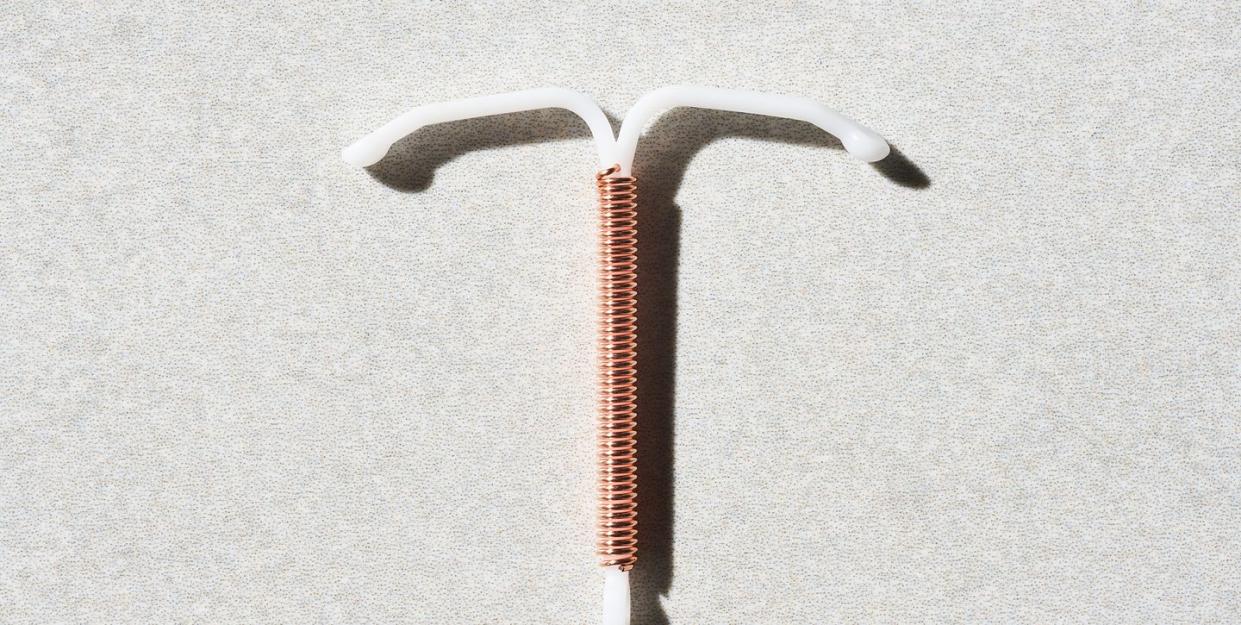
Then there’s the copper IUD. This option is often overlooked, and although it's not FDA-approved for this use, it’s actually the most effective form of emergency contraception. If you can get an appointment to have a copper IUD placed within five days of unprotected sex, it has a near 100 percent efficacy rate at preventing pregnancy. (You have up to seven days after if you know the unprotected sex wasn’t more than five days after you ovulated.)
Studies of Plan B (and generic counterparts) and Ella show effectiveness ranging between 60 and 90 percent. The hormonal IUD, which contains 52 milligrams of levonorgestrel, has also been studied for emergency contraception, but there is not enough evidence yet to determine whether it works well for that purpose.
The great thing about Plan B is that it is available over the counter without a prescription. Ella requires a prescription from a health care provider, but many practitioners will write a prescription so you can also have it on hand. (Both pills are effective for up to three to five years—take a look at the expiration date and keep it in a dry, temperature-stable location.)
Myth: Plan B is an “abortion pill.”
If you are already pregnant, no method of emergency contraception will cause an abortion. That’s just not how it works. During a normal menstrual cycle, your brain sends a signal (via a hormone called luteinizing hormone) to your ovaries (more specifically, to the dominant follicle in your ovaries) to release an egg into your fallopian tubes. Once the egg is released, there’s an opportunity for sperm to meet the egg and implantation to occur, which is the point at which pregnancy begins.
Both Plan B and Ella work by preventing or delaying the signal from the brain to release the egg. This ruins the perfect timing required for the sperm to meet the egg, making pregnancy impossible. (Note: Emergency contraception is the use of something—pill or an IUD—before you are pregnant, to prevent pregnancy. It's standard practice to rule out pregnancy before a copper IUD placement, and patients typically do a urine pregnancy test too.)
The copper IUD works as emergency contraception by creating an environment in the uterus that isn’t well suited for sperm, so that the sperm can’t make it to the egg, regardless of whether you’ve ovulated already or not. More specifically, the copper in the IUD increases cervical mucus that immobilizes sperm so it’s much harder for it to swim up into the uterus. The copper IUD also causes changes to the uterine lining, making it harder for a fertilized egg to implant.
It is really important for people to understand, especially for those living in states with abortion bans, that emergency contraception will not cause abortion. If you are pregnant and need to end your pregnancy, emergency contraception will not affect the embryo at all. You’ll need abortion care, either via a medication abortion that can be managed with misoprostol and mifepristone (both of which—for now—are still on the market via prescription), or a surgical abortion. Those living under bans may need to travel to access this care. Abortion funds and organizations like IneedanA.com, abortionfinder.com, and Aid Access can help connect you to resources for accessing care.
Myth: Plan B doesn’t work if you’re overweight.
This one’s tricky, but everyone, no matter their weight, definitely has options.
Let’s start with the bad news. Plan B, the most accessible option for emergency contraception, does appear to prevent pregnancy less often for those at a higher weight or higher body mass index. Overall, the research suggests Plan B is about three to four times less effective for those with a BMI higher than 30 (though Plan B does not acknowledge this research).
If your BMI is 30 or higher or your weight is 176 pounds or more, your best options for emergency contraception are going to be either the copper IUD or Ella. Remember, you can get an advanced prescription of Ella from your health care provider to have on hand. In my experience, many practitioners will do what it takes to fit you in ASAP for inserting the copper IUD for emergency contraception if that’s what you want.
All this said, while Plan B may not work as well for certain folks, it is the most easily accessible. So if you’re in a situation where you need emergency contraception and Plan B is your only option (say, you can’t get an appointment in time or a prescription for Ella), take it. Plan B may be less effective for those with a higher BMI, but it may not be completely ineffective for you. It’s better than not doing anything.
Myth: If you’re at a higher weight, you should take two Plan B pills.
In my research at Oregon Health & Science University, we looked at ways to improve Plan B efficacy by increasing the dose. Unfortunately, while taking two pills or increasing the dose did not cause issues or other side effects, it also did not improve how well levonorgestrel works to delay or stop ovulation. It’s unclear exactly why levonorgestrel isn’t as effective for some people at a higher weight, even at a higher dose. It seems there may be some other factor involved that’s stopping the drug from actually getting to the ovary or the brain to interrupt the signaling that releases the egg.
Myth: You have to be 18 or older to get Plan B, and the best place to get it is the pharmacy.
There are no restrictions for Plan B or the 11 generic versions of the pill that are available on the market. It is available at the pharmacy to anyone who needs it at any age. This goes for male partners as well. You don’t have to identify as a woman to pick it up. Plan B is even available on Amazon!
If you are a minor and need to see a health care provider for a prescription for emergency contraception (whether that’s for Ella or a copper IUD), you can access contraceptive care without parental involvement in most states in most cases, according to the Guttmacher Institute.
Many options exist to order Ella without a “formal” clinic visit. In fact, most of the time you can just call your healthcare provider and they can send a prescription in for you. But let’s say you don’t have a go-to doctor or they won’t send in an Rx—or you’re worried your parents might have access to your health record. In those cases, you can access telehealth emergency contraception providers. These allow you to see a provider virtually or via phone, so you can access emergency contraception prescriptions online. Many telehealth emergency contraception providers will offer overnight shipping or same-day pickup, depending on the method and where you live.
Of course, another consideration is cost, which can vary widely. Plan B and its generic versions can cost anywhere from $10 to $50. While Ella may be cheaper because it can be covered by insurance, you also have to factor in the cost of a visit with a healthcare provider. (Telehealth services may be the most affordable, depending on your insurance situation.) Cost is another reason to secure a dose of either pill now to have it ready—you don’t want to waste time shopping around when you actually need it.
Myth: You only have 24 hours to take Plan B.
Emergency contraception is often referred to as “the morning-after pill.” It’s catchy, but it’s not quite accurate. You shouldn’t wait until the morning after—take it as soon as you can. This is the best advice for all of the available options because we know that the sooner you take an emergency contraception pill or get a copper IUD placed, the higher the average efficacy for preventing pregnancy.
This is why I recommend having the pills in your medicine cabinet already. Think of emergency contraception like a fire extinguisher. You hope you never have to use it, but it’s smart to have it immediately available in case you do.
That said, if you can’t take emergency contraception immediately, you still have time. For Plan B and its generics, you have up to 72 hours (three days) according to the FDA label, but data shows it can work up to 120 hours (five days) after sex. For Ella, you have 120 hours (five days) to take it. With the copper IUD, which again is the most effective of all your options, you may have up to seven days, depending on when you ovulated.
Myth: One Plan B pill protects you for an entire month.
Plan B and Ella protect you only for that one act of unprotected sex. If a condom breaks or slips later in the month, then you would need to take emergency contraception again. This is one of the top reasons for the failure of emergency contraception—people think it will continue to protect them for weeks afterward. The only emergency contraception method that continues to protect you from pregnancy is the copper IUD, because it’s also a very effective regular contraceptive method.
Myth: Taking Plan B too many times harms your fertility.
Using emergency contraception will not affect your fertility—whether you use it once or repeatedly. Remember that the ingredients in the pills are very similar to (if not the same as) what is used in regular birth control pills. The IUD is used by millions to safely prevent pregnancy and can be used for up to 3, 5, or even 10 years at a time, depending on the device. These medicines are FDA-approved and have been used for decades. There is no evidence that any of the options affect fertility down the line.
I wouldn’t recommend using emergency contraception as regular birth control—but that’s mostly because it can be inconvenient and get expensive if you use it that way. It would also be likely that your bleeding pattern would be very irregular (which is a total nuisance), and it’s worth noting that emergency contraception may cause more nausea than regular birth control pills. Plus, using emergency contraception like Plan B as regular birth control doesn’t work as well as other contraceptive methods. The bottom line: Even if you did use it every time you had sex, Plan B wouldn’t hurt you, your fertility, or a pregnancy once established.
Unfortunately, we are living through a moment when women’s health is tragically politicized. Myths about your reproductive health, and emergency contraception in particular, may continue—but knowing the facts ahead of time can help you make the decision that’s best for you when you need to.
How To Know Which Option Is Right For Me
You need emergency contraception. Do you want the most effective type?
Duh.
The copper IUD is nearly 100 percent effective as emergency contraception. Would you be open to having an IUD placed?
[accordion id= '88702c98-5f37-44d1-9ed9-e760da4c77c9'][/accordion]
Which option is more effective for you, based on your BMI?
[accordion id= 'f945a7db-7d28-49a1-a2c9-277be1ddd75c'][/accordion]
Alison Edelman, MD, MPH, is an ob-gyn with specialty training in complex family planning, a professor of obstetrics and gynecology at Oregon Health & Science University, and a researcher.
You Might Also Like

