What Is GERD?

elenaleonova / Getty Images
Medically reviewed by Jay N. Yepuri, MD
GERD, which stands for gastroesophageal reflux disease, is a gastrointestinal disorder that occurs when your stomach acid repeatedly flows back into your esophagus (the tube that carried food from your mouth to your stomach). This may cause symptoms such as heartburn, chest pain, and regurgitation into your mouth; however, some people do not experience any symptoms at all. As many as 28% of people in North America have GERD.
GERD is generally treated with a type of medication called a proton pump inhibitor (PPI). If you do not respond to this treatment or if your condition gets worse, your healthcare provider may order further testing.
While GERD is typically a chronic, lifelong condition, it can be managed with lifestyle changes, medications, and, in more significant cases, surgery. If you are diagnosed with GERD, you must follow your healthcare provider's instructions for medication therapy and lifestyle changes. Doing so can help alleviate your symptoms and improve your quality of life.
VectorMine / Getty Images
Types
GERD is classified into three different types, which are based on how much damage they've caused in your esophagus. These three different types include non-erosive reflux disease (NERD), erosive esophagitis, and Barrett's esophagus.
Non-Erosive Reflux Disease (NERD)
Non-erosive reflux disease is a type of GERD in which the esophagus is unharmed by stomach acid. It is the most common type of GERD and is seen in 60-70% of people with the condition. NERD may eventually worsen into a more erosive form of the disease. Left untreated, NERD can negatively impact your overall digestive health.
Erosive Esophagitis
Erosive esophagitis, which is seen in 30% of people with GERD, is inflammation or injury to the lining of the esophagus (esophageal mucosa) caused by the acid in your stomach that is refluxed into your throat. If left untreated, esophagitis can develop into a condition called Barrett’s esophagus and increase your risk for esophageal cancer.
Barrett's Esophagus
Barrett's esophagus is seen in 6% to 12% of people with GERD. This condition occurs when the tissue lining your esophagus is replaced with tissue that is similar to the lining of your intestines. This is a serious form of GERD and can lead to the development of a rare cancer called esophageal adenocarcinoma.
Symptoms of GERD
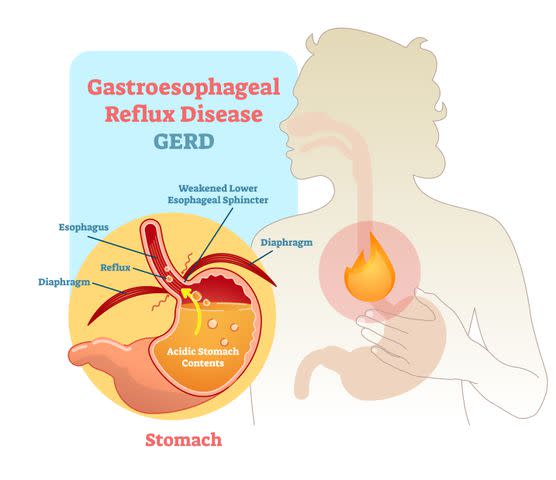
There is a band of muscles called the lower esophageal sphincter that works with the diaphragm to prevent your stomach contents from refluxing into your esophagus. If that barrier is relaxed at inappropriate times or is compromised in some way, you can develop GERD.
After repeated or prolonged exposure to stomach acid, you can start to exhibit symptoms of GERD. But, it is important to note that not everyone experiences GERD in the same way, and it is possible to not experience symptoms at all. Here are some potential symptoms of GERD:
Heartburn
Regurgitation of your stomach contents
Chest pain
Difficulty swallowing (dysphagia)
Chronic cough
Hoarseness
Unexplained weight loss
Sometimes people will experience what is known as a globus sensation, or a lump in their throat impacting swallowing. Although there is still a great deal of debate over the cause of globus, about 28% of people with reflux will have this sensation. However, should you encounter this feeling, it is important to be evaluated by your healthcare provider as it may be a symptom of a different underlying condition.
What Causes GERD?
Technically, there is no known cause as to why someone develops GERD; although, researchers have identified a number of possible explanations.
One possible explanation is motor abnormalities in your digestive system. Esophageal dysmotility is when the muscles in your digestive system do not work properly and your body experiences changes in the speed, strength, or coordination of your digestive organs. This can make it difficult for your body to clear the acid from your esophagus.
Another possibility is that the tone of the lower esophageal sphincter becomes chronically relaxed, leaving it open and making it easier for acid reflux to occur.
Scientists also speculate that gastroparesis, or delayed gastric emptying, could contribute to GERD. Gastroparesis occurs when your digestive system is slowed and it takes a longer period of time for your stomach and small intestines to pass their contents.
Risk Factors
There are certain conditions and anatomical factors that can increase your risk of developing GERD. For instance, your risk increases if you have a hiatal hernia or an increase in intra-abdominal pressure. Other risk factors for GERD include eating a high-fat diet, smoking, and consuming alcohol.
There is also a greater chance you will experience GERD if you are pregnant or taking certain medications. For instance, 40%-85% of pregnant people experience GERD, which is most likely related to increased progesterone (a key reproductive hormone) causing relaxation of the lower esophageal sphincter. Meanwhile, the medications most commonly associated with GERD are non-steroidal anti-inflammatory drugs (NSAIDs), antibiotics like tetracyclines and clindamycin, and statins.
Diagnosis
Your healthcare provider may make an initial diagnosis based on your symptoms, especially if they are typical. In this case, they may have you try a medication known as a proton pump inhibitor (PPI) to see if your symptoms improve.
If you have some uncommon or atypical symptoms such as difficulty swallowing or unintended weight loss, your healthcare provider may need to order additional tests to confirm your diagnosis. Here are some of the tests you could potentially undergo.
Esophageal pH Monitoring
Measuring something's pH can tell you how acidic or how basic it is. During esophageal pH monitoring, a small tube with a pH sensor at the tip will be passed through your nose into your esophagus. Measurements of the acid exposure in your esophagus are collected over a 24-hour period. This can tell you how much acid is getting into your esophagus.
Typically, this test is ordered if a healthcare provider is not sure if your symptoms are related to GERD or if you have not responded to the medications prescribed.
Upper Endoscopy
This test is performed using an endoscope—a small camera on a tube—which is passed through your mouth and into the esophagus. It allows your healthcare provider to look at the lining of your esophagus and small intestine and take a biopsy (a tissue sample) if needed.
This invasive test is used when you exhibit alarm symptoms like difficulty swallowing, are unresponsive to PPI medications, or you have a high risk for Barrett's esophagus. Although, the results aren't definitive; 40-60% of people with GERD will have a normal result.
Esophageal Manometry
This test involves numbing you and then passing a small tube through your nose and into the esophagus. You will be asked to swallow once the tube is in position so that measurements of your esophageal function and lower esophageal sphincter can be taken. While this test does not diagnose GERD, it can let your healthcare provider see how well your esophagus and lower esophageal sphincter are working.
Esophageal Impedance pH Study
Although this test is not widely available, it functions much like the 24-hour pH monitoring test. It is also used when you have normal results from a 24-hour pH probe.
A tube is passed through your nose into your esophagus at the level of your lower esophageal sphincter. This test measures the liquid movement from your stomach into the esophagus. It typically detects whether or not you have a bile reflux instead of an acid reflux. Bile is a digestive fluid that is made by the liver and stored in the gallbladder.
Esophagogram
Sometimes called a barium swallow, an esophagogram is used to evaluate dysphagia (or difficulty swallowing) and is not often used to diagnose GERD because of its low sensitivity. Instead, this procedure is geared toward assessing hernias and gut motility disorders.
Treatments for GERD
GERD is a chronic disease that does not resolve on its own nor is there a cure. Long-term treatment and management are usually necessary. These treatments usually involve lifestyle modifications, medications, and sometimes surgery.
Keep in mind that over-the-counter medications provide temporary symptom relief and do not prevent the recurrence of your symptoms. They also do not allow an injured esophagus to heal. Here is a closer look at some of the treatments for GERD.
Lifestyle Changes
Many healthcare providers will recommend that you make lifestyle changes in order to reduce your symptoms. These might include quitting smoking, losing weight, and changing your eating habits. They also may recommend that you raise the head of your bed to help prevent nighttime GERD and improve your sleep hygiene. Sleep reduces transient lower esophageal sphincter relaxations and can reduce your GERD symptoms. Wearing loose-fitting clothing may also be helpful.
Medications
You may be prescribed medication if you continue to have GERD-related symptoms despite making lifestyle changes. A healthcare provider may recommend lifestyle changes and medications simultaneously if your symptoms are severe. Some common medications used include:
Antacids: These medicines neutralize acid in the stomach.
Histamine 2 receptor antagonists (H2RAs): These decrease the amount of gastric acid that is secreted in the stomach.
Proton pump inhibitors (PPIs): These reduce the amount of stomach acid that is made in the lining of the stomach.
Transient lower esophageal sphincter relaxer reducers (TLESR reducer): These medications help prevent the transient lower esophageal sphincter from relaxing, which prevents acid from entering the esophagus.
Prokinetics: These promote motility in the digestive tract, which can help with conditions like gastroparesis.
Of all the medications available, PPIs are considered the most effective choice for GERD due to their consistent acid suppression. One of the most commonly prescribed drugs in this class is Prilosec (omeprazole). PPIs are the most widely-prescribed medication for NERD and erosive esophagitis.
Surgery
Surgery is considered for people who do not want to take medications for an extended period of time or who are intolerant to available medications. This approach has become increasingly popular since laparoscopic anti-reflux surgery was introduced. The success rate is relatively high, particularly for people with heartburn, regurgitation, and trouble swallowing.
Related: Here's Everything You Need to Know About the Complications of GERD
Prevention
While some cases of GERD may be caused by your age or the way your body is structured and functions (which are outside of your control), there are other things you can do prevent the likelihood of developing GERD. For instance, you are more likely to experience GERD if you have a high body mass index (BMI), smoke, or are not physically active.
Taking steps to stop smoking or to remove secondhand smoke from your home is a good first step toward preventing GERD. In fact, a 2016 study found that nearly 44% of people who quit smoking reported fewer episodes of GERD one year after quitting.
Managing your weight also can help prevent GERD—especially since a significant number of people with a high BMI experience GERD.
You also can try incorporating moderate physical activity into your daily regimen. Research shows that consistently engaging in exercise can be beneficial for preventing GERD as well as reducing the likelihood of experiencing symptoms if you have already been diagnosed with the condition. That said, vigorous activity may exacerbate the condition in people predisposed to developing GERD, so you should experiment to see what level of exercise works best for you.
Related: 9 Things That Could Be Giving You Acid Reflux
Related Conditions
GERD often occurs alongside a number of other conditions or may even lead to the development of some medical conditions. For instance, research shows that people with GERD are more likely to wake up at night and may even experience sleep disorders. People with GERD are more likely to experience insomnia, sleep dissatisfaction, difficulty initiating sleep, and major depressive disorder.
A 2017 study found that anxiety and depression were significantly more common in people with GERD. As many as 42% of people with a psychological disorder experience GERD, but it's unclear which contributes to the other or if they have an inverse relationship. Having a psychological comorbidity also reduces the likelihood that your GERD symptoms will resolve. It is hypothesized that anxiety and depression can negatively affect your response to PPIs, which are used to treat GERD.
Other GERD comorbidities include high blood pressure, high cholesterol, and type 2 diabetes.
Living With GERD
If you have been diagnosed with GERD, it is important to follow your healthcare provider's instructions, particularly if they have prescribed medication or recommended lifestyle changes like smoking cessation, weight loss, and physical activity. There also are other things you can do to reduce your symptoms and alleviate your discomfort.
For instance, there is some evidence that modifying your diet may be helpful. You may want to limit highly acidic or spicy foods, alcohol, and unhealthy fats as well as ensure you are eating plenty of fruits and vegetables, lean protein, and healthy fats.
You can try chewing gum (not spearmint or peppermint) to increase your saliva production and reduce the amount of acid in your esophagus. You also want to ensure you have good posture, especially after eating. Try not to lie down for two hours after eating; instead, stand, move around, and sit up straight. Elevating the head of your bed if help if you experience GERD at night.
Frequently Asked Questions
Can GERD heal on its own?
If you have GERD, it is important to note that it will not go away on its own. Your esophagus needs time to heal, and the best way for that to happen is to make lifestyle changes and follow a healthcare provider's advice when it comes to medications. Prescription medications, such as proton pump inhibitors, may be recommended as well as maintaining a healthy weight.
GERD usually resolves in infants by their first birthday. Fewer than 5% of children will still have GERD by the time they reach toddlerhood.
Can anxiety activate GERD?
It is possible that stress and anxiety can exacerbate or even prompt your symptoms of GERD. A 2018 study of 19,000 people found that those with anxiety were more likely to experience GERD. Researchers speculate that increased anxiety may reduce pressure in the lower esophageal sphincter, making it easier for acid to flow into the esophagus. High anxiety also increases your acid production, increasing the likelihood of GERD.
How long does a GERD flare-up last?
To be diagnosed with GERD, you need to experience symptoms at least twice a week on a consistent basis. But, the duration of GERD symptoms varies from person to person depending on how recent your diagnosis is and your treatment plan.
Ongoing symptoms that do not respond to initial treatment with proton pump inhibitors may require additional testing. Even once you receive a diagnosis, there is a risk that your symptoms will linger for long periods of time. In fact, about one-third of people with GERD do not improve with the use of PPIs.
For more Health news, make sure to sign up for our newsletter!
Read the original article on Health.

